Home Mechanical Ventilation in Europe started as tracheostomy ventilation in the late 1970s1; it remained under-utilized and restricted to specialized centres in France.
Due to the transition to non-invasive ventilator support, patients under Home Mechanical Ventilation (HMV) have grown worldwide.2
Indeed, HMV became widespread in Europe and a survey (Eurovent) presenting data from 2001 to 2002 in 16 European countries (including a total of 483 centres), showed a global prevalence of 6.6 per 100,000 with a wide variation between countries.3
In 2010, the European COPD audit (surveying 13 countries), showed that although a majority of centres offered invasive and noninvasive ventilation, 40.5% of centres declared not to have the capacity to ventilate at home all eligible patients.4
In fact, organization varies widely in Europe, in countries like Denmark, where patients are referred to only 2 respiratory care units (RCU)5 or Sweden where there are a wide number of outpatient clinics that take care of the patients and report to the Swedish HMV Register (Swedevox), owned by the Swedish Society of Chest Medicine and financially supported by the National Board of Health and Welfare.6
The Swedevox registry is a well-functioning national structure for implementing, monitoring, and securing valid prescription and management of both HMV and Longterm Oxygen Therapy.7
In 2011, the British Thoracic Society Respiratory Critical Care Group, strongly suggested that National registries should be implemented to reduce variations in care and improve patient safety.8
In a recent cross-national, cross-sectional study comparing one Australian and one Canadian predominantly publicly funded HMV services, there were marked regional differences in the clinical characteristics of individuals receiving assisted ventilation and the care practices used to support them. Yet, in spite of these differences Health Related Quality of Life was not different between the two sites. There were also considerable differences in the proportions of individuals using invasive ventilation, and undergoing PSG, home implementation of NIV, or using routine airway clearance techniques.9
Based on assistance activities, technical and human resources, accredited training in ventilation, teaching and research activity the Spanish society of Pulmonology (SEPAR) has recently established the minimum requirements for a HMV centre, defining basic units (BU), Specialized Units (SU) and High Complexity Multidisciplinary Units (HCMU).10,11 Currently there are in Spain, 13 HCMU, 12 SU and 9 BU.12
In Portugal based on the same criteria we have characterized 18 HMV units (60% response rate) in 3 HCMU, 14 SU and 1 BU.13
According with German Guidelines for Chronic Respiratory Failure, 3 types of centres are defined: weaning centre, HMV centre with expertise in invasive HMV and HMV centre with special focus on NIV.14
Additionally, the network “WeanNet”, founded in 2007 within the German Society of Pneumology and Respiratory Medicine (DGP), has undergone a certification process and by October 2018, 53 weaning centres have been certified.15
For complex patients (like invasively ventilated or under 24h noninvasive ventilatory support) a home care package (including professional caregivers) is highly recommended. However, an adequate home care package (HCP) with professional caregivers is not available in the majority of European countries which unnecessarily delays hospital discharge and puts informal caregivers into a huge burden.
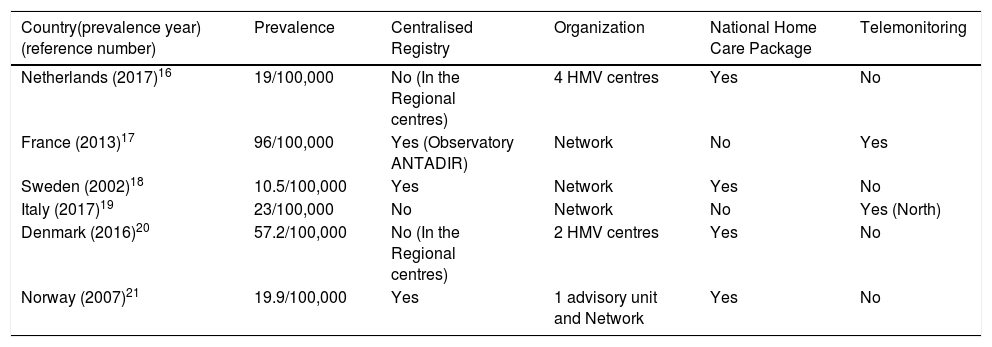
The table included shows a number of organizational aspects of some European countries together with the most recent available prevalence of HMV16-21. Countries like the Netherlands and Denmark have a centralised HMV organization, whereas Sweden, Norway, France and Denmark have registries established more than 15 years ago. A national HCP for complex patients is established in the Netherlands, Sweden, Denmark and Norway (highly dependent on municipalities). Telemedicine is being applied in Italy and France (Table 1).
Number of organizational aspects of some European countries.
| Country(prevalence year) (reference number) | Prevalence | Centralised Registry | Organization | National Home Care Package | Telemonitoring |
|---|---|---|---|---|---|
| Netherlands (2017)16 | 19/100,000 | No (In the Regional centres) | 4 HMV centres | Yes | No |
| France (2013)17 | 96/100,000 | Yes (Observatory ANTADIR) | Network | No | Yes |
| Sweden (2002)18 | 10.5/100,000 | Yes | Network | Yes | No |
| Italy (2017)19 | 23/100,000 | No | Network | No | Yes (North) |
| Denmark (2016)20 | 57.2/100,000 | No (In the Regional centres) | 2 HMV centres | Yes | No |
| Norway (2007)21 | 19.9/100,000 | Yes | 1 advisory unit and Network | Yes | No |
Necessarily there will be centres with more experience in patients with neuromuscular disease, some with expertise in chronically critically ill patients, compared with others specialized in integrated programmes for COPD or obesity related respiratory failure.
The diversity of HMV organization throughout Europe demonstrates that no ideal model has yet been found. However we should move towards a more uniform pathway in order to achieve better outcomes, picking the best experiences from each country and constructing a more balanced European HMV network.
Given the increasing numbers of patients, a European Observatory for HMV could serve as a tool to set up the standards.
Accreditation of HMV units in Europe requires consideration to ensure equal access to treatment for patients, based on knowledge, best practices and justice among geographical distribution.