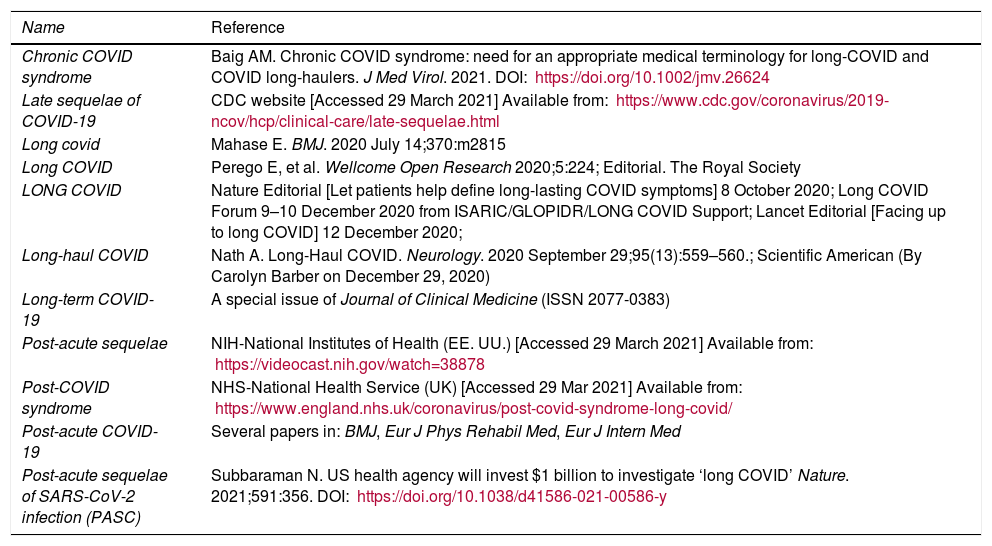
Coronavirus disease 2019 (COVID-19) is still far from over1. At the end of spring 2020, when the first wave of cases began to be controlled, something unusual was observed: some COVID-19 patients still had symptoms weeks after the initial infection had passed. They reported symptoms that included fatigue, dyspnea, chest pain, palpitations, gastrointestinal symptoms, mental confusion, anxiety, and depression, and more than 150 other possible associated symptoms2 that persisted for weeks or months. This was surprising, because some patients who had less severe disease initially and were treated only in primary care or remained practically asymptomatic during acute infection, were eventually among the most sick3. The terminology for this phenomenon varies (Table 1). The WHO currently recommends calling it a “post-COVID-19 condition”, as this name does not attribute causality or duration, and there are already specific ICD-10 (U09) and ICD-11 (RA02) codes to identify it4. Beyond the name, a universal definition agreed by consensus with societies, organisms, and patients, is necessary5.
Repository of suggested names for post-COVID-19 condition.
| Name | Reference |
|---|---|
| Chronic COVID syndrome | Baig AM. Chronic COVID syndrome: need for an appropriate medical terminology for long-COVID and COVID long-haulers. J Med Virol. 2021. DOI: https://doi.org/10.1002/jmv.26624 |
| Late sequelae of COVID-19 | CDC website [Accessed 29 March 2021] Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/late-sequelae.html |
| Long covid | Mahase E. BMJ. 2020 July 14;370:m2815 |
| Long COVID | Perego E, et al. Wellcome Open Research 2020;5:224; Editorial. The Royal Society |
| LONG COVID | Nature Editorial [Let patients help define long-lasting COVID symptoms] 8 October 2020; Long COVID Forum 9–10 December 2020 from ISARIC/GLOPIDR/LONG COVID Support; Lancet Editorial [Facing up to long COVID] 12 December 2020; |
| Long-haul COVID | Nath A. Long-Haul COVID. Neurology. 2020 September 29;95(13):559–560.; Scientific American (By Carolyn Barber on December 29, 2020) |
| Long-term COVID-19 | A special issue of Journal of Clinical Medicine (ISSN 2077-0383) |
| Post-acute sequelae | NIH-National Institutes of Health (EE. UU.) [Accessed 29 March 2021] Available from: https://videocast.nih.gov/watch=38878 |
| Post-COVID syndrome | NHS-National Health Service (UK) [Accessed 29 Mar 2021] Available from: https://www.england.nhs.uk/coronavirus/post-covid-syndrome-long-covid/ |
| Post-acute COVID-19 | Several papers in: BMJ, Eur J Phys Rehabil Med, Eur J Intern Med |
| Post-acute sequelae of SARS-CoV-2 infection (PASC) | Subbaraman N. US health agency will invest $1 billion to investigate ‘long COVID’ Nature. 2021;591:356. DOI: https://doi.org/10.1038/d41586-021-00586-y |
Estimates of how many people develop post-COVID-19 condition vary. Curiously, it seems to affect more middle-aged adults than elderly people, but so far no one knows for certain why it occurs or who is most likely to be affected, and with more than 126 million cases of COVID-19 to date worldwide, the number of people at risk is increasing6. Many post-COVID-19 patients, individually or jointly in associations such as SOSCOVID, Persistent COVID-19 Collective Madrid, and others, report that their primary care doctors (and pulmonologists) initially ruled out and ignored their symptoms, thus aggravating their suffering7. This phenomenon also occurs in children, to their parents’ despair. Multidisciplinary clinics to treat these patients have now sprung up in hospitals and clinics in the United Kingdom and Italy8.
SARS-CoV-2 is not the first virus to cause lasting symptoms or new associated syndromes9. Previous epidemic viral outbreaks such as Zika, chikungunya, SARS, and MERS, and before them, the 1918 flu (wrongly called the Spanish flu) left many people weakened for months, sometimes years. In these patients, the virus is no longer live or active, but they present persistent symptoms. In terms of causative mechanisms, we have some possible suspects.
Excess inflammation: this is the primary candidate, as abnormally high levels of inflammation are seen in many patients.
Autoimmune response: raised levels of autoantibodies have been found in patients with post-COVID-19 condition. And certain autoimmune diseases, such as lupus and rheumatoid arthritis, commonly cause fatigue and digestive problems.
Nervous system problems: dysautonomy, which refers to the deregulation of the autonomic nervous system, affects blood flow, including to the brain, and can cause fatigue, headaches, mental confusion, and exercise intolerance.
Blood clots and vascular damage: many patients with elevated d-dimer blood levels improve with the administration of prophylactic anti-coagulation. Autopsies of people who died of COVID-19 have revealed widespread clots.
This brings us to the question of how these patients should be treated. Many need to be seen by various specialists, from respiratory medicine experts to cardiologists, gastroenterologists, and of course, primary care physicians10–12. After magnetic resonance imaging, tomography, blood analyses, and other tests have been performed, the goal of treatment must be to identify underlying problems, control symptoms, and improve functional capacity.
The post-COVID-19 condition is a new challenge13, caused by a new virus. New studies will soon provide some answers. Meanwhile, the best way to protect yourself is … avoid infection. If you contract COVID-19, be sure to take enough time to recover before returning to your normal activity. We know from Zika, chikungunya, SARS, and MERS, and from patients with chronic fatigue syndrome (now called systemic exercise intolerance disease) that putting on too much pressure on sufferers can cause recurrence and a slower than expected recovery. The good news is that after 6 months a gradual improvement is seen in most series of patients, including those who were admitted to the ICU14. Paraphrasing George Bizet’s Carmen (1845): “Prends garde de faire un faux pas!!” — “Watch out … for the post-COVID-19 condition!”
Please cite this article as: Soriano JB, Ancochea J. Sobre la nueva condición post COVID-19. Arch Bronconeumol. 2021. https://doi.org/10.1016/j.arbres.2021.04.001