Non-small cell lung cancer (LC) accounts for 80%–85% of all the varieties of this neoplasm, with adenocarcinoma being the most common histological type.1 The prognosis of this disease is poor due to low survival and high recurrence rates.2 We present here a patient who presented oligo-recurrences during the course of his disease, which were treated surgically.
This is a male, 42-year-old smoker investigated due to a lung shadow appearing on an unrelated chest X-ray. Computed tomography (CT) showed central radiodensity 4cm×2cm in the upper left lobe, without adenomegalies. Fiber optic bronchoscopy and aspiration cytology gave a diagnosis of epithelial type LC, confirmed by frozen section biopsy during thoracotomy, which was complemented by left upper lobectomy and mediastinal lymphadenectomy (stations 5–7 and 10). The post-operative histopathological result showed predominantly solid, mucin producing, poorly differentiated invasive adenocarcinoma, with no epidermal growth factor receptor overexpression or mutation and metastases in two aortopulmonary window lymph nodes. Treatment was complemented with sequential chemotherapy.
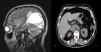
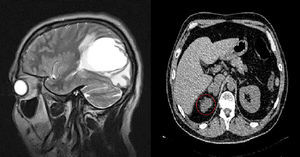
Nine months later, the patient presented visual disturbances and vertigo. Magnetic resonance imaging of the head with contrast medium was performed and a single tumor lesion was found in the left temporal lobe (Fig. 1, right panel). Metastasectomy with adjuvant radiotherapy was performed. Five months later, abdominal tumoration of the right adrenal gland was detected on an abdominal ultrasound (Fig. 1, left panel), confirmed on a CT scan with contrast. Adrenalectomy was performed. The patient is currently in follow-up, 5 years after the last procedure.
The terms oligo-metastasis, proposed by Hellman and Wechselbaum in 1995 and revised by Niibe et al. in 2006 to oligo-recurrence2,3 are LC stages in which metastases or recurrences (between 1 and 5 lesions) can be treated with local treatments. The differences originate in the control of the primary tumor and how it appeared: in oligo-recurrence, the primary tumor is controlled and recurrence is metachronous; in oligometastases, the opposite occurs. In brief, oligo-recurrence is a metachronous, oligometastatic state where the primary tumor is controlled.3
Positron emission tomography has reduced the diagnosis of oligo-recurrences, since many of them are metastatic in the initial diagnosis. However, despite being included in the diagnostic protocols, these imaging studies are not available in some countries.
Control of the primary tumor, nutritional status, histological type and the number of metastases are factors which impact on the treatment of oligo-recurrence.3–5 However, a determinant factor for survival is the presence or absence of metastatic lymph node involvement (0%–35%).4,5
In view of the current technological advances and the use of local and systemic treatments, surgery3–5 is appropriate for some patients with oligo-recurrences. Our patient, despite having N2 lymph nodes, has had good survival, reinforcing the “seed and soil” theory of interaction between the cell and host in LC or in any other type of cancer.
Please cite this article as: García Rodríguez ME, Armas Pérez BA, Armas Moredo K. Oligorrecurrencia a partir de un adenocarcinoma del pulmón. Utilidad de la resección. Arch Bronconeumol. 2014;50:46–47.