Pathologies acquired after the establishment of an artificial airway include stenosis, granulomas and the formation of pseudomembranes, to name a few. The most common form of presentation in adults is circumferential stenosis, which often requires therapeutic endoscopic measures to achieve resolution.
This Case Report describes the case of an obstructive inflammatory tracheal pseudomembrane secondary to repeated intubations that was resolved with conservative treatment.
The clinical presentation of this entity generally includes the appearance of respiratory infection and/or atelectasis after the withdrawal of the orotracheal tube as a consequence of the accumulation of secretions between the tracheal wall and the pseudomembrane. Inflammatory pseudomembranes can resolve spontaneously with the help of glucocorticoids, although on occasion they require an invasive endotracheal procedure depending on the evolution.
Dentro de las patologías adquiridas tras la instauración de una vía aérea artificial tenemos: las estenosis, los granulomas, la presencia de pseudomembranas y la formación de tabiques traqueales, entre otros. La forma más habitual de presentación en el adulto es la estenosis circunferencial y muchas veces requiere para su resolución medidas endoscópicas terapéuticas.
En esta Nota clínica se describe el caso de una pseudomembrana traqueal inflamatoria obstructiva secundaria a intubaciones repetidas y que se resolvió con tratamiento conservador.
La presentación clínica de esta entidad generalmente incluye la aparición de infección respiratoria y/o atelectasia tras la retirada del tubo orotraqueal, siendo consecuencia del acúmulo de secreciones entre la pared traqueal y el tabique formado. Los tabiques traqueales inflamatorios se pueden resolver espontáneamente con ayuda de glucocorticoides, otras veces requieren de un procedimiento endotraqueal invasivo en función de la evolución.
We present the case of a woman with obstructive inflammatory tracheal pseudomembrane secondary to repeated intubation, with complete resolution within a few days using conservative treatment based on respiratory physiotherapy and anti-inflammatory drugs (glucocorticoids), without requiring a more complex bronchoscopic procedure. The interest of this case lies in the unusual presentation of a post-intubation tracheal inflammatory reaction, as well as its subsequent evolution.
Clinical ObservationThis is the case of a 74-year-old woman, smoker with a cumulative dose of 60 packs/year, with a history of chronic obstructive pulmonary disease (COPD) and kyphoscoliosis. Her most recent functional tests revealed moderate airflow limitation, predominantly obstructive (FVC 1.0l (58% of ref.), FEV1: 0.630l (54% of ref.), FEV1/FVC ratio: 63%).
She arrived at the emergency department after being intubated at home due to severe respiratory failure with a decreased level of consciousness. Her family members reported that the patient had presented coughing with rusty sputum, progressive drowsiness and dyspnoea on minimal exertion over the previous 72h. Once in the intensive care unit (ICU), empirical treatment was initiated with broad spectrum antibiotics, glucocorticoids (intravenous methylprednisolone 60mg/day) and bronchodilators. She initially progressed well and was extubated 48h later. However, the patient deteriorated again within a few hours, presenting respiratory failure and hypercapnic acidosis that was not corrected with non-invasive mechanical ventilation, and which required reintubation. Two days later, she accidentally removed the tube, before being reintubated as the severe respiratory failure persisted. In the following days, she again progressed well, and was extubated definitively about 10 days after the first intubation and then transferred to a conventional hospital ward.
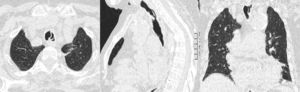
Once on the Respiratory Medicine ward, a chest radiograph was performed, which showed volume loss in the left lung. Videobronchoscopy was therefore indicated, in which the presence of a tracheal pseudomembrane of inflamed tissue that formed a septum of around 2cm in length, dividing the middle third of the endotracheal lumen, was observed (Fig. 1A and B). It also revealed the presence of mucous secretions retained in the bronchial tree, especially in the left side, interpreted as atelectasia of the left lung secondary to mucous retention due to the presence of the tracheal pseudomembrane described. A chest computed axial tomography (CT) scan was performed, showing an inflammatory infiltrate in the lingula, probably in resolution, and also confirming the presence of an intratracheal septum that raised the differential diagnosis of tracheal duplication, traumatic sequelae and reaction to a foreign body (due to repeated intubations) (Fig. 2). In the following hours, treatment was intensified with respiratory physiotherapy and she remained on antibiotic and glucocorticoid therapy. The possibility of performing a therapeutic endotracheal procedure was raised in the following days, but was never carried out due to the patient's gradual improvement. The endoscopic check-up a few days later confirmed that the intratracheal septum had completely disappeared (Fig. 1C). Curiously, the patient reported that the day before this test, she had expelled a dense material with coughing. The patient received the following glucocorticoid treatment in total: intravenous methylprenisolone 60mg/day for 8 days, followed by 40mg/day for 2 days; she was then changed to oral prednisone 30mg/day, in a tapered regimen until discontinuation.
Evolution of the tracheal pseudomembrane. (A and B) Tracheal pseudomembrane in the form of a longitudinal septum, connected to the anterior and posterior wall of the trachea, 2–3cm long and located in the middle third of the trachea. (C) Resolution of the pseudomembrane with the presence of some remaining mucus.
The patient was discharged and sent home with the following diagnoses:
- 1.
Hypercapnic respiratory failure secondary to exacerbation of chronic lung disease (COPD+kyphoscoliosis).
- 2.
Mechanical ventilation (with repeated intubations).
- 3.
Lingular pneumonia.
- 4.
Left pulmonary atelectasia and retention of secretions secondary to an obstructive tracheal pseudomembrane resolved with conservative treatment.
The presence of pseudomembranes and tracheal inflammatory reactions due to various causes is a well-known finding. The interest of the case presented lies partly in the clinical presentation, in the form of a longitudinal tracheal septum of a significant size that compromised the lumen and movement of secretions, as well as its complete resolution within a few days of using conservative treatment based on respiratory physiotherapy and anti-inflammatory drugs (glucocorticoids). In our case, extraction or mechanical treatment of the lesion using more complex therapeutic bronchoscopic procedures were unnecessary. Unfortunately, and as a limitation, the histological analysis of the lesion described, which could have provided useful information on its tissue characteristics, is not available.
Among the conditions acquired after the introduction of an artificial airway (intubation or tracheostomy), post-intubation stenosis is the most common in adults,1 and is due to extensive scarring in an area of the airways in which a transmural lesion was produced on intubation. Most of these stenoses are circumferential (tranverse membrane, in the form of a bottleneck or granuloma) and surround the tracheal wall, although it can rarely present in the form of a septum, as occurred in this clinical case. The appearance of tracheal pseudomembranes is not an uncommon finding for bronchoscopists in patients with long periods of intubation. However, when we review the literature on this condition, there are few cases reported and/or articles that explain its incidence, physiopathology and treatments used.
It is known that among the factors that could contribute to increasing the risk of the aforementioned disorders are: traumatic or prolonged intubation, repeated intubations (as happened in our case), an excessively large tube, tube movements and local infection. Added to these causes are possible predisposing factors, such as autoimmune mechanisms,2 administration of glucocorticoids and the effect of gastro-oesophageal reflux.3,4 Other authors suggest that the presence of intratracheal septa or pseudomembranes represents an early stage of ischaemic lesion in the tracheal wall related with the high pressure of the cuff on intubation. This endotracheal pressure exerted by the tube produces inflammation, infarction and finally, necrosis of the tracheal mucosa with the secondary development of tracheal stenosis.5,6 These inflammatory lesions sometimes resolve spontaneously or aided by glucocorticoid treatment (although there are no formal guidelines in this respect). However, most cases require the application of interventionist endoscopic techniques (rigid bronchoscopy, laser resection or electrocauterization, etc.).7,8 In other cases, this complication has a fatal outcome, despite a history of short-duration intubation.6 Therefore clinicians, especially those who work with the airways, must be alerted to this little known complication within endotracheal intubation.
Please cite this article as: Crespo-Lessmann A, Torrego-Fernández A. Tabique traqueal inflamatorio. Arch Bronconeumol. 2013;49:402–4.