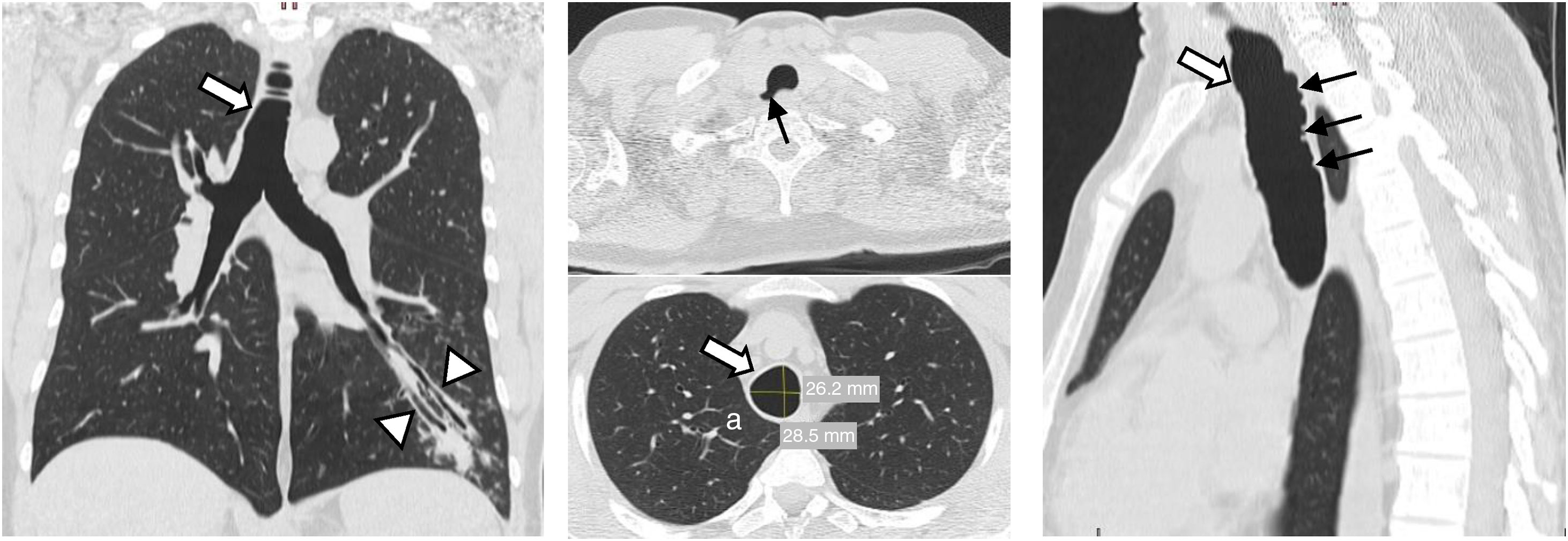
A 40-year old never-smoker, caucasian male, with no relevant past medical history and normal respiratory function tests, was observed due to the persistence of fever, cough, and sputum despite being treated with antibiotics for 5 days. A computed tomography was performed, which revealed a dilated trachea (26.2cm×28.5cm, as coronal and sagittal diameters), tracheal diverticula and bronchiectasis (Fig. 1). These findings were consistent with the diagnosis of Mounier-Kuhn Syndrome.
Mounier-Kuhn Syndrome, or idiopathic tracheobronchomegaly, is a congenital disorder, first reported in 1932 by Mounier-Kuhn and is characterized by trachea and proximal bronchi enlargement. Patients are frequently diagnosed between the 5th and 6th decades of life. This syndrome has an evident male preponderance.1 Tracheal diameters superior to 25mm×27mm in men and 21mm×23mm in women (coronal and sagittal diameters) are the diagnostic criteria.2 Clinical presentation is usually subtle but frequently involves recurrent infections and decreased mucociliary clearance.
The cause of this condition is poorly understood, but it is thought to be related to the atrophy of elastic fibers leading to thinner smooth muscle layer resulting in tracheobronchial dilatation. Also, the presence of expiratory collapse, tracheal diverticula, and bronchiectasis is common. It can be found in association with connective tissue diseases. In this case, the patient did not show any symptom or physical abnormality to consider those diagnoses.
The treatment approach in this pathology is focused on preventing respiratory infections and optimizing mucociliary clearance.