Since it was first described in 1965, the Montgomery T-tube has become a highly valuable tracheal prosthesis in benign tracheal stenosis, because of its ease of placement and low incidence of serious complications. However, patients need regular follow-up to clean these prostheses and monitor the frequent development of endoluminal granulomas. We report the 25-year experience of our respiratory endoscopy unit in the use of Montgomery T-tubes (MTT), from 1993 to 2018.
During this period we used MTTs in 53 patients, 30 women and 23 men, with an overall mean age of 50 years (SD: 21.6). These devices were used in cases of tracheal stenosis who were not candidates for surgery or in whom other treatments failed.
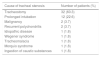
The etiologies prompting MTT placement in our series are shown in Table 1, the most common being tracheal stenosis caused by tracheostomy (32; 60.3%) and prolonged intubation (12; 22.6%).
Indications for MTT placement in our series.
| Cause of tracheal stenosis | Number of patients (%) |
|---|---|
| Tracheostomy | 32 (60.3) |
| Prolonged intubation | 12 (22.6) |
| Malignancy | 2 (3.7) |
| Recurrent polychondritis | 2 (3.7) |
| Idiopathic disease | 1 (1.8) |
| Wegener syndrome | 1 (1.8) |
| Tracheomalacia | 1 (1.8) |
| Morquio syndrome | 1 (1.8) |
| Ingestion of caustic substances | 1 (1.8) |
The method initially selected in 32 cases (60%), depending on the characteristics of the stenosis or the patient, was MTT. In the remaining 21 cases, other approaches were attempted first (tracheal prostheses in 12, tracheostomy cannulas in 7, and surgical techniques in 2 cases), but poor patient response led to the placement of an MTT. The MTT was placed using rigid bronchoscope (RB) in 11 individuals (20.7%), while in the remaining patients, it was introduced directly through the tracheal stoma.
In 15 cases (28.3%), patients were followed up in other centers after prosthesis placement because most (12 cases; 22.6% of the total) presented motor deficits, paraplegia, or tetraplegia, usually as a result of traffic accidents.
In terms of changes over time, an analysis of 5-year periods shows that the use of this device has steadily diminished: 15, 14, 10, 8 and 6 cases respectively in each period. All MTTs were placed by 1 of the 3 members affiliated with the unit during the 25-year period.
A median of 20 (11.5; 38) examinations were performed in the 38 patients followed in our hospital, taking into account those performed before and after MTT, and the median follow-up was 49 months. In 72% of cases, the device needed to be replaced. The median number of replacements per patient was 3.5 (1; 9).
Complications, defined as those that required intervention by our unit (excluding accumulation of secretions, bacterial colonization of the MTT, or subcutaneous tissue infection), occurred in half of the cases. The most frequent were inflammatory reaction or granulomas, usually proximal, which required replacement of the MTT by another with a shorter proximal branch. In one case, the prosthesis migrated to the airway, a rare but highly significant complication, which logically led to the removal and replacement of the MTT.
MTT was the final treatment in 32 cases, and the device was withdrawn in the remaining patients. The tracheostomy was closed in 17 patients after withdrawal of the device (42.5%).
MTT was developed by the otolaryngologist William Montgomery and used for the first time in a cervical tracheal surgical procedure in 1964.1 The prototype was made with a rigid material that made it difficult to insert, so in 1965 Professor Montgomery developed a flexible model, consisting of a single piece of silicone, which was first used in a case of post-tracheostomy subglottic stenosis.2 In 1968, Boston Medical Products developed the “Safe T-Tube” and its use became widespread.
This prosthesis consists of two branches, a vertical tube that is placed in the tracheal lumen and a horizontal tube that exits via the tracheostoma. The latter part has several circumferential ridges to prevent displacement. The surface is smooth and polished to prevent the retention of secretions and the formation of granulation tissue.
Its indications vary widely, although it was initially conceived for surgical interventions such as tracheal stenting prior to definitive surgery.3 Given the increasing incidence of benign tracheal stenosis resulting from tracheostomy and intubation, the use of MTT in interventional pneumology is growing.4,5 It has also been used in other less common airway conditions, such as recurrent polychondritis6 or mucopolysaccharidosis.7
Prior study of the airway anatomy by CT before placement is essential to select an appropriate device length and internal diameter. The traditional method involves general anesthesia and use of an RB that would allow patient ventilation and treatment of stenosis, with adjustment to the airway size. Montgomery, however, also described another method8 that does not require RB: the lower branch is inserted through the stoma at the distal end of the trachea using forceps, then the proximal branch is placed once correct positioning has been confirmed by flexible bronchoscopy. Other insertion methods have been developed to solve some of the problems that occur with this system.9
Advantages over other tracheal prostheses include less risk of displacement than other devices, such as the Dumon stent.10 Other important advantages over tracheal cannulas is the preservation of phonation11 and the esthetic appearance.
Complications associated with MTT must be mentioned. The most common is granulation tissue formation at the distal and proximal ends that may require replacement of the prosthesis. Most are mild, but others are more serious, such as breakage of one of the branches or prosthesis migration, which involves urgent interventional management.
In conclusion, although case series with larger populations have been reported,12 we describe a series of MTT from one of the interventional pulmonology units in Spain with most experience in the management of tracheobronchial and airway prostheses, and report indications, follow-up, and management resulting from a 25-year experience.
Please cite this article as: Margallo Iribarnegaray J, García Luján R, Pina Maíquez I, Revuelta Salgado F, Alfaro Abreu J, de Miguel Poch E. Prótesis en T de Montgomery para el tratamiento de la estenosis traqueal: experiencia de una Unidad de Endoscopia Respiratoria y revisión de la literatura. Arch Bronconeumol. 2020;57:72–73.