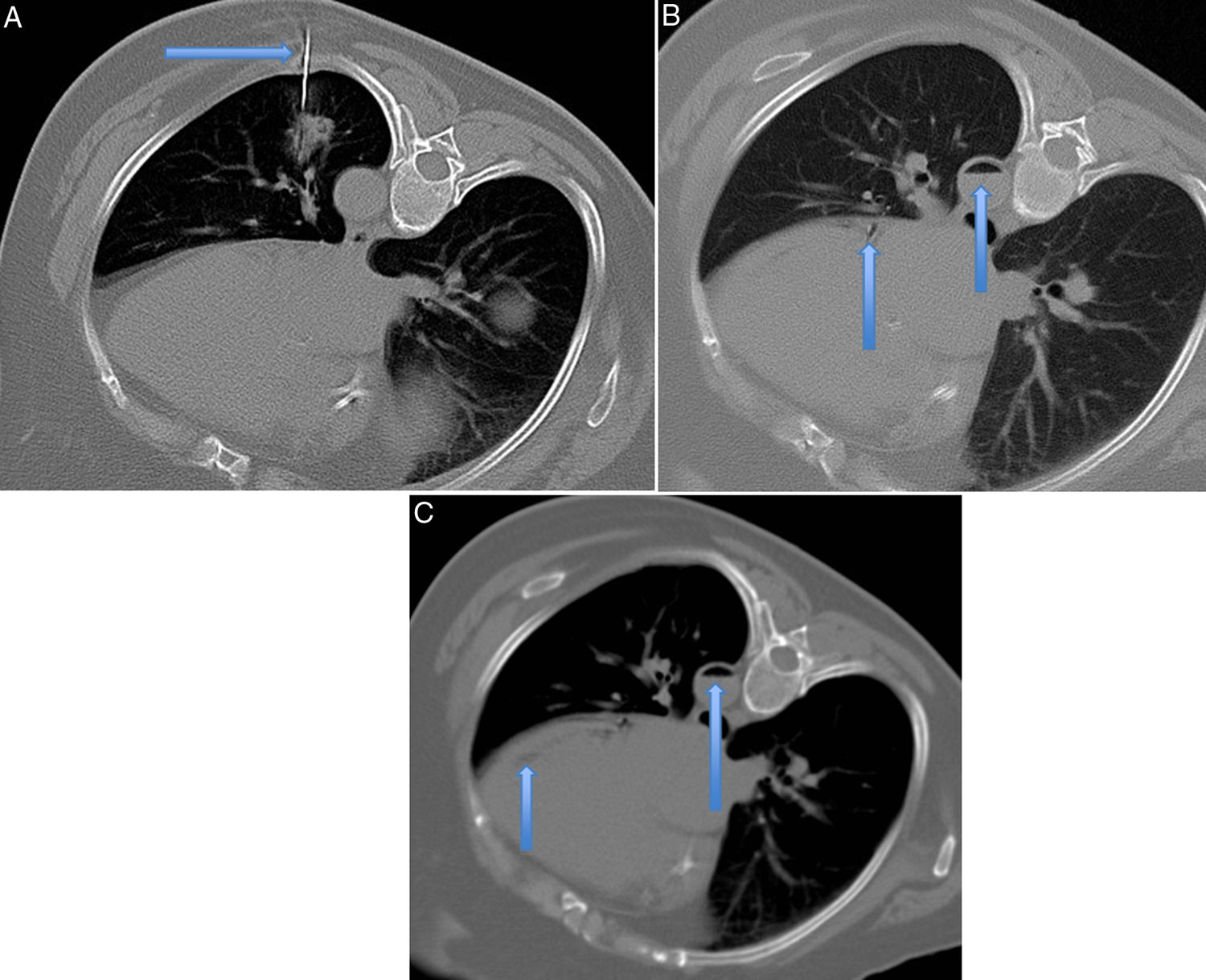
We report the case of a 72-year-old woman diagnosed in 2015 with T3N0M0 adenocarcinoma of the sigma, who presented 4 years later with a pulmonary nodule in the left lower lobe. Biopsy was requested (Fig. 1A). The procedure was performed in the right lateral decubitus position, because the lesion could not be approached from the supine position: the patient could not tolerate prone decubitus, and a colostomy prevented left lateral decubitus.
Axial CT slices for performing lung biopsy with the patient positioned in the right lateral decubitus position. A) The upper left image shows the Tru-Cut needle entering the lesion located in the lower left lobe (arrow). B) The upper right image shows the presence of air within the descending aorta artery and the circumflex artery (arrows). C) The lower image shows the presence of air inside the left ventricle (arrow).
CT-guided biopsy was obtained in a single pass using a coaxial needle and 20G Tru-Cut needle.
Immediately after the aspiration, the patient developed cough with bloody sputum, and symptoms of sweating, chest pain, and respiratory distress with O2 saturation of 96%. CT revealed a minimal pneumothorax and air in the descending thoracic aorta and circumflex artery (Fig. 1B).
Blood pressure was monitored and O2 was administered at 100%, after placing the patient in the Trendelenburg position to avoid cerebral embolism.
Minutes later, she showed clinical improvement. A new CT scan was performed which showed that the air in the descending aorta had decreased, while a minimal amount remained in the left ventricle (Fig. 1c).
The patient was admitted to the ICU and was discharged after 48h without symptoms.
Post-biopsy arterial embolism of the pulmonary nodule is a rare complication, but it is potentially lethal as it can be associated with angina pectoris.1 Incidence ranges from 0.02% to 0.4% of procedures, although in most cases it is an asymptomatic, undiagnosed complication.2
Please cite this article as: Lendoiro SL, Armentia ES, Rodríguez CM. Angor debido a embolismo aéreo arterial tras biopsia pulmonar. Arch Bronconeumol. 2020;57:71.