The effectiveness of needle aspiration in the initial treatment of primary spontaneous pneumothorax has been widely studied. The objective of this research was to compare digital with manual aspiration in a randomized clinical trial.
MethodsWe designed a blinded parallel-group randomized clinical trial with a 1:1 allocation ratio. The clinical trial is reported in line with the guidelines of the CONSORT group. The primary outcome variables were immediate success and hospital admission, while the secondary outcome measures were relapse, re-admission and need for surgery, and length of hospital stay. A satisfaction survey was also carried out among clinicians who perform these 2 types of aspiration.
ResultsA total of 67 patients were included in the study (n = 36, control group; n = 31, experimental group) with no losses to follow-up. In both groups, 58% of procedures were immediately successful, avoiding hospital admission. No differences were found in rates of relapse, re-admission, need for surgery, or length of hospital stay. Overall, 80% of clinicians who performed aspiration preferred the digital system, and this preference rose to 100% among clinicians who performed more than 5 procedures a year.
ConclusionsBoth manual and digital aspiration provide good immediate results avoiding hospital admission, while digital drainage is preferred by clinicians responsible for first-line treatment of pneumothorax.
La efectividad de la punción aspiración en el tratamiento inicial del neumotórax espontáneo primario ha sido ampliamente estudiada. El objetivo de este trabajo es comparar la aspiración digital frente a la manual en un ensayo clínico aleatorizado.
MétodosSe ha diseñado un ensayo clínico aleatorizado paralelo con ratio 1:1 y evaluación ciega. El ensayo clínico se adapta al estándar del grupo CONSORT. El resultado primario se define como éxito inmediato e ingreso hospitalario, y los secundarios, como recidiva, reingreso, necesidad de cirugía y días de ingreso. Se realiza encuesta de satisfacción entre los profesionales que realizan los dos tipos de punción.
ResultadosSesenta y siete pacientes han sido incluidos en el estudio (n = 36 grupo control, n = 31 grupo intervención) con un seguimiento del 100%. Ambos grupos presentan un éxito inmediato del 58%, evitándose el ingreso hospitalario. No se observan diferencias en cuanto a recidiva, reingreso, necesidad de cirugía o días de ingreso. El 80% del personal que realiza la técnica de punción prefiere la aspiración digital, siendo el 100% entre el personal que realiza más de 5 punciones al año.
ConclusionesTanto la punción aspiración manual como la digital ofrecen buenos resultados inmediatos que evitan ingresos hospitalarios; la aspiración digital es el método preferido por quienes realizan dicha técnica.
El estudio AMVADI fue registrado con el número ISRCTN46137912 en el ISRCTN Registry de BioMed Central.
Pneumothorax is defined as the presence of air in the pleural space, and can be acquired (iatrogenic and traumatic) or spontaneous, depending on its etiology. These categories are, in turn, divided into primary (no obvious cause), secondary (underlying pleuropulmonary disease as an obvious cause), and catamenial (associated with the menstrual cycle).
It is difficult to determine the real extent of the incidence of primary spontaneous pneumothorax, although figures in the literature suggest that the incidence is 16.7/100,000 per year in men and 5.8/100,000 per year in women, according to Gupta et al.,1 or 7.4–18/100,000 per year (adjusted for age) in men and 1.2–6/100,000 per year (adjusted for age) in women, according to Noppen and De Keukeleire.2
The initial treatment of the first episode of primary spontaneous pneumothorax ranges from observation3,4 to surgery.5,6 However, in cases of large pneumothorax or unstable patients, the clinical practice guidelines recommend active ambulatory treatment.7 Needle aspiration and the use of external devices such as minichest tubes or Heimlich valves offer greater advantages in terms of avoiding admissions without increasing recurrence.7–10. In spite of this, other guidelines do not include this approach as the first line of treatment,11 and in other studies needle aspiration is presented as a therapeutic strategy with low adherence.12,13
Our aim in this study was to demonstrate the advantages of digital needle aspiration (by reducing the human factor of aspiration) versus standard manual aspiration in order to improve acceptance and increase the uptake of this strategy.
Materials and methodsStudy design and participantsThe AMVADI study is a parallel randomized trial with a 1:1 randomization and blind evaluation. The clinical trial meets CONSORT standards for parallel-group randomized trials.14
The AMVADI study was registered under number ISRCTN46137912 in the ISRCTN BioMed Central Registry.
The study subjects were patients with a first episode of primary spontaneous pneumothorax (presence of air in the pleural space, without prior trauma or iatrogenesis and without underlying pleuropulmonary disease) in whom active treatment with needle aspiration was indicated.
Inclusion criteriaPatients with a first episode of primary spontaneous pneumothorax with symptoms (uncontrolled pain or dyspnea) or lung collapse greater than 20% as measured by the Light index.
Exclusion criteria- •
Acquired pneumothorax (traumatic or iatrogenic).
- •
Suspicion of secondary pneumothorax based on clinical and radiological criteria.
- •
Suspicion of catamenial pneumothorax based on clinical and radiological criteria.
- •
Previous episodes.
- •
Bilateral pneumothorax.
- •
Tension pneumothorax.
- •
Immunosuppression.
Interventions in both groups were performed by staff of the general emergency department (where manual needle aspiration has been performed since 1997). Both groups are described below.
Control groupA Pleuropath® pleural tube was placed in the second intercostal space, clavicular midline. After placement, a 50 cc syringe was used to manually aspirate up to 3500 cc or until air was no longer aspirated (whichever occurred first). The chest tube was closed and a chest X-ray was performed at 6 h (a 4−12 h range was accepted to ensure the patient's night rest). If lung expansion or marginal apical pneumothorax was observed on the X-ray, the drain was removed and the patient was discharged from hospital. If it persisted on X-ray, the tube was connected to a water seal and the patient was admitted to the hospital.
Experimental groupThe procedure was the same as in the control group, with the difference that once the Pleuropath® was placed, it was connected to a digital suction system at ↓10 cmH2O aspiration pressure until the flow ceased (two measurements separated by 5 min. with 0 ml/min flow) or maximum 30 min. (whichever occurred first). If aspiration persisted for more than 30 min, the patient was admitted. If aspiration stopped before 30 min, the chest tube was closed and a chest X-ray was performed at 6 h (a 4−12 h range was accepted to ensure the patient's night rest). If lung expansion or marginal apical pneumothorax was observed on the X-ray, the drain was removed and patient was discharged from hospital. If it persisted on X-ray, the tube was connected to a water seal and the patient was admitted to the hospital.
The suction system used was Thopaz®.
Study variablesPrimary outcome variables. Primary outcome variables were immediate success and admission to hospital. Immediate success was defined as aspiration (manual or digital), closure of the chest tube followed by removal of the tube and discharge home.
Secondary outcome variables. Variables such as days of admission, need for surgery, recurrence, and readmission within the first 30 days were also measured.
Demographic variables. Data were collected on the age of the participants, sex, weight, height, smoking history, pneumothorax side, and percentage collapse measured by the Light index.
An anonymous survey was also administered to the staff of the emergency department who carried out the needle aspiration to ascertain the number of aspirations performed and the preferences for use.
Recruitment and sample sizeAll subjects treated who met the study criteria and gave informed consent were included in the study.
It was estimated that between 60 and 100 patients would be recruited during the study period (3 years). This sample size was guided by the volume of care and the calculated volume of the previous retrospective study. A formal sample size calculation was not performed because the efficiency of the automatic drainage system was entirely unknown.
RandomizationA computer-based randomization sequence was developed. This sequence was kept in the clinical epidemiology department of the Hospital Universitario Donostia, so that the investigator recruiting the patients did not know in advance to which group the patient would be assigned (hidden randomization sequence). Once the patients had been evaluated by the general emergency staff, and if they met the criteria for inclusion in the study and signed the consent form, an opaque envelope was opened showing the intervention to be performed (manual [control group] or digital [intervention group]).
MaskingDue to the characteristics of the interventions, masking was not possible, but if there was any doubt about resolution on the follow-up X-ray, a member of the thoracic surgery department was asked to decide. This surgical staff member was unaware of the patient’s assigned group.
StatisticsA descriptive analysis of variables using mean and standard deviation for quantitative variables and absolute and relative frequencies for categorical variables was performed. The distribution of the variable of interest among the 2 groups (manual aspiration and digital aspiration) was analyzed using the Chi-square test (χ2) and Student’s t-test for categorical and quantitative variables, respectively. The impact of the type of intervention on time to recurrence was analyzed using the Kaplan-Meier test and log-rank test. Version 14.1 of the STATA® statistical program was used for this purpose.
Ethical considerationsThe risk was similar in both the intervention group and the control group. However, as this is an experimental study, it required the approval of the Guipúzcoa Clinical Research Ethics Committee (CREC) (see Annex). The patients, or in the case of minors, their parents or guardians, were informed of the study and asked to sign the informed consent. The collected data were processed and used in accordance with good clinical practice guidelines and the principles of the Data Protection Law.
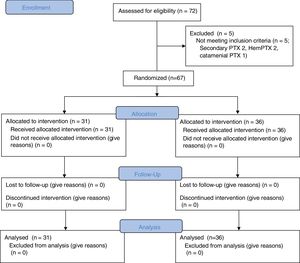
ResultsOver a period of 38 months (November 16, 2011 to January 7, 2015), 72 patients with a first episode of primary spontaneous pneumothorax were initially included as potential candidates for randomization. After the exclusion criteria were checked, 5 were excluded and the remaining 67 were included in the study. Of these, 36 were assigned to the control group and 31 to the intervention group. Fig. 1 shows how patients included in the study were recruited and randomized.
No patients were lost to follow-up. Seven months after study inclusion was complete, all patients were contacted to verify their status, so the follow-up range is between 7 and 45 months.
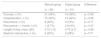
The characteristics presented by patients in both groups (Table 1) were analyzed first, and it was determined that they do not differ in age, sex, pneumothorax side, body mass index (BMI), smoking habit, or pack-year index, as expected in an RCT. These data revealed that the typical patient in our study was a young male, smoker or former smoker, with a right pneumothorax. Indeed, this pattern coincides with the typical patient with spontaneous idiopathic pneumothorax.
Patient characteristics.
| Manual group | Digital group | Difference | |
|---|---|---|---|
| (n = 36) | (n = 31) | ||
| Age, mean (SD) | 29.72 (10.33) | 27.58 (10.12) | p = 0.4 |
| Sex, M/W | 29/7 | 28/13 | p = 0.8 |
| Side, R/L | 22/14 | 18/13 | p = 0.5 |
| BMI, mean (SD) | 22.25 (3.61) | 20.86 (1.93) | p = 0.08 |
| Smoking habit: smoker/former/never | 18/14/13 | 21/1/9 | p = 0.32 |
| PYI, mean (SD) | 8.6 (9.14) | 12.22 (8.58) | p = 0.15 |
| Light index, Average (SD) | 52.44 (23.92) | 46.25 (20.97) | p = 0.27 |
BMI: body mass index, calculated by weight (kg)/height (m)2; L: left; M: men; PYI: pack-year index, calculated by number of packs smoker per day multiplied by number of years; R: right; SD: standard deviation; smoker/former/never: active smoker/former smoker/never smoker; W: women.
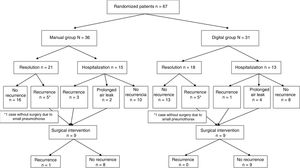
Secondly, the main study variables were analyzed (Table 2). Resolution with ambulatory management was observed in 58% of the patients, distributed equally among both groups. Neither the recurrence rate, readmission rate, nor days of admission show statistically significant differences between the groups. Need for surgery was indicated according to the criteria normally used in the hospital for primary spontaneous pneumothorax (recurrence, prolonged air leak > 5 days, at-risk professions). Of the 18 patients who underwent surgery, 12 were for ipsilateral recurrence and 6 for prolonged air leak. Surgical procedures included bullectomy with abrasion on 14 occasions and bullectomy with pleurectomy on 4 occasions. Postoperative recurrence rate was 5.5% (1 case).
Main study outcome variables.
| Manual group | Digital group | Difference | |
|---|---|---|---|
| (n = 36) | (n = 31) | ||
| Success, n (%) | 21 (58%) | 18 (58%) | p = 0.98 |
| Hospitalization, n (%) | 15 (42%) | 13 (42%) | p = 0.98 |
| Recurrence, n (%) | 8 (22%) | 6 (19%) | p = 0.77 |
| Recurrence < 1 month, n (%) | 1 (2.7%) | 2 (6.4%) | p = 0.47 |
| Length of stay, mean (SD) | 2.73 (1.6) | 4.76 (2.7) | p = 0.98 |
| Need for intervention, n (%) | 9 (25%) | 9 (29%) | p = 0.71 |
Success: resolution of symptoms by ambulatory needle aspiration.
Hospitalization: need for hospital admission with a fine tube connected to a water seal.
Recurrence: episode of pneumothorax in the same hemitorax (includes all patients who recur, including patients who recur in the first month).
Recurrence < 1 month: recurrence within the first month of admission.
Length of stay: number of days admitted to the hospital.
Need for intervention: patient operated for pneumothorax; criteria for surgery: recurrence, prolonged air leak, at-risk professions (pilot or professional divers).
Fig. 2 describes the management of randomized study patients.
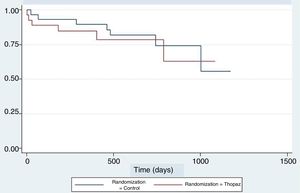
An analysis of recurrences during follow-up was also performed using the Kaplan-Meier test. Fig. 3 shows that the patterns of both graphs are similar throughout the follow-up period.
The absolute risk of success or resolution of the episode without admission in the digital aspiration group in our study was 58%. With our sample size, this means that with a 95% confidence interval the success of this technique can be estimated at between 34% and 91%.
The study was not designed as a non-inferiority study, but had we performed such an analysis we would have had to establish a minimum value in order to consider the technique successful. We could assume success to mean that in one-third of patients with primary spontaneous pneumothorax the condition is resolved without admission, as occurred in our retrospective cohort study. Based on this assumption, taking the lowest value of the confidence interval for digital aspiration (34%) we would be above the minimum value, so in a no-difference study, digital aspiration would be at least as effective as manual aspiration.
An anonymous satisfaction survey was conducted among emergency department staff who performed the needle aspiration. Twenty professionals answered the question of how many aspirations they performed each year and whether they felt more comfortable with the manual or digital aspiration. A total of 80% of professionals preferred the digital method, and all professionals who performed more than 5 aspirations/year (8 emergency doctors) chose this option.
DiscussionStudies are regularly published on the initial treatment of primary spontaneous pneumothorax, indicating its importance. Treatments for a first episode range from simple observation, ambulatory management with needle aspiration or Heimlich valves, to hospital management with chest drains and surgical intervention.3–11
In most published papers, observation is reserved for stable patients with pneumothorax involving a lung collapse of less than 20%. However, some studies question whether pneumothorax size should be the criterion for deciding whether patients with pneumothorax should be observed or treated.4
If active treatment has been decided, it seems clear that there is no difference in recurrences or readmissions between placing a chest tube and admitting a patient and performing ambulatory needle aspiration, while the use of needle aspiration could prevent two-thirds of admissions, as demonstrated by two systematic reviews.10–15 Another clinical trial with 56 randomized patients subsequently showed very similar results, confirming that needle aspiration does not increase recurrence rates.16 Unlike other clinical trials, this study recruited patients with traumatic pneumothorax, and this variable was an independent factor for good prognosis at resolution. Female gender was also seen to be an independent factor, with women showing better resolution data than men.
Even with all the scientific tests available, needle aspiration is rarely undertaken as the first step in the management of pneumothorax in many countries,12,13 and few emergency departments perform it in Spain. The low reliance on evidence in this setting may be a criticism of the small number of patients enrolled in clinical trials. In fact, the systematic review only retrieved 331 patients from 4 clinical trials.10 However other trials have continued to corroborate these results,16 and the lack of evidence supporting an approach other than ambulatory management leads us to think that other factors prevent the implementation of a needle aspiration strategy in hospitals.
The lack of strict protocols means that needle aspiration is less used. A retrospective cohort study conducted by our group found that hospital admissions could have been avoided in twice as many patients if needle aspiration had been part of routine clinical practice.17 The human factor was also identified as one of the possible reasons for this reduced uptake, along with the absence of protocols.
In contrast, in the same hospital with the same emergency department staff, after the AMVADI study has been designed, the decrease in admissions as a result of needle aspiration was the same as that reported in other published papers. In this study, 58% of patients who underwent needle aspiration (manual or digital) were managed in an ambulatory setting without admission.
The clinical trial failed to demonstrate that eliminating the human factor from aspiration and performing it with a digital device further reduces admissions. If we were to apply a non-inferiority principle, the digital system would have been shown to be not inferior to the manual intervention, with a 95% confidence interval of 31%–91%. In our study both options reduced admissions by 58%, in line with published literature.10–15 Pneumothorax recurrence data after 7–45 months’ follow-up show reasonable figures ranging from 19% in the digital aspiration group to 22% in the manual aspiration group.
The limitations of these data must be taken into account: for example, a larger sample size might provide smaller confidence intervals and even reach statistical significance in some of the results. The fact that this is a practical study performed in a single center could make it difficult to extrapolate results to clinical practice. However, in centers where manual needle aspiration is already performed, transition to a digital system should not be a problem if nurses were given a short training course (15−20 min clinical session). The different aspiration techniques of the 2 methods makes it difficult to select the same volume/time criteria for both. However, manual aspiration of up to 3500 cc is the standard volume used in different RCTs17 and wall suction in pneumothorax was performed at ↓10 cmH2O for 30 min maximum. We also believe that the different protocols do not alter the outcome, as patients with intact pleura are resolved with both protocols, and if the pleura is not intact, the problem will not be resolved with either protocol.
The digital system is increasingly used as a support technique in thoracic surgery departments. It has proven to be beneficial and convenient for both patients and caregivers. In 1 paper, 15 staff members of the thoracic surgery department in a hospital in Birmingham were asked for feedback on the convenience of using the digital system in patients with diverse surgical conditions; 67% rated it as very good or excellent.18 Similarly, a survey conducted in the emergency department found that 80% of respondents prefer to use the digital system in routine practice. Among the group of respondents, all physicians performing needle aspiration procedures more than 5 times a year prefer the digital system. Other studies confirm that these systems are useful in the management of pneumothorax in different phases.19 Based on these results, we believe that digital aspiration may facilitate the applicability of this strategy.
Cost-effectiveness studies show that the implementation of this strategy is of the utmost importance. In a study of 60 consecutive patients with pneumothorax, 48 were aspirated with a pigtail drain, resulting in an estimated reduction in hospitalization costs of 114,000 euros.20 The economic impact of needle aspiration in England has been analyzed, and estimates show that not performing aspiration in 10% of patients costs the English national health system more than £438,412 per year. The authors also found that application of the ACCP protocol (drainage and admission without needle aspiration) in England would entail an additional annual cost of £3.9 million.21
In conclusion, we believe that digital aspiration systems can be an effective alternative and that this approach increases user satisfaction. This could facilitate the expansion and wider implementation of the technique.
Conflict of interestsThe authors state that they have no conflict of interests.
Please cite this article as: Aguinagalde B, Zabaleta J, Fernández-Monge A, Lopez I, Izquierdo JM, Redin JA, et al. Aspiración manual versus aspiración digital en el tratamiento inicial del neumotórax espontáneo primario: estudio AMVADI. Ensayo clínico aleatorizado. Arch Bronconeumol. 2020;56:637–642.