We report the case of a 61-year-old woman with a 10-year history of adrenal insufficiency, osteoporosis, and hypercholesterolemia, treated with prednisone at average doses of 20mg/day. The patient presented with a soft, mobile, painful pre-sternal mass that had appeared 4 months previously. An ultrasound was performed that revealed a hypoechoic nodular image, with no evidence of vascularization, measuring 29×21mm, suggestive of fibrolipoma. The mass was resected surgically and confirmed in the histological study to be lipoma. Seven days after the procedure, the wound opened spontaneously and began to suppurate. The wound was cleaned, samples were taken for cultures, and oral antibiotic therapy was started. Culture results were negative.
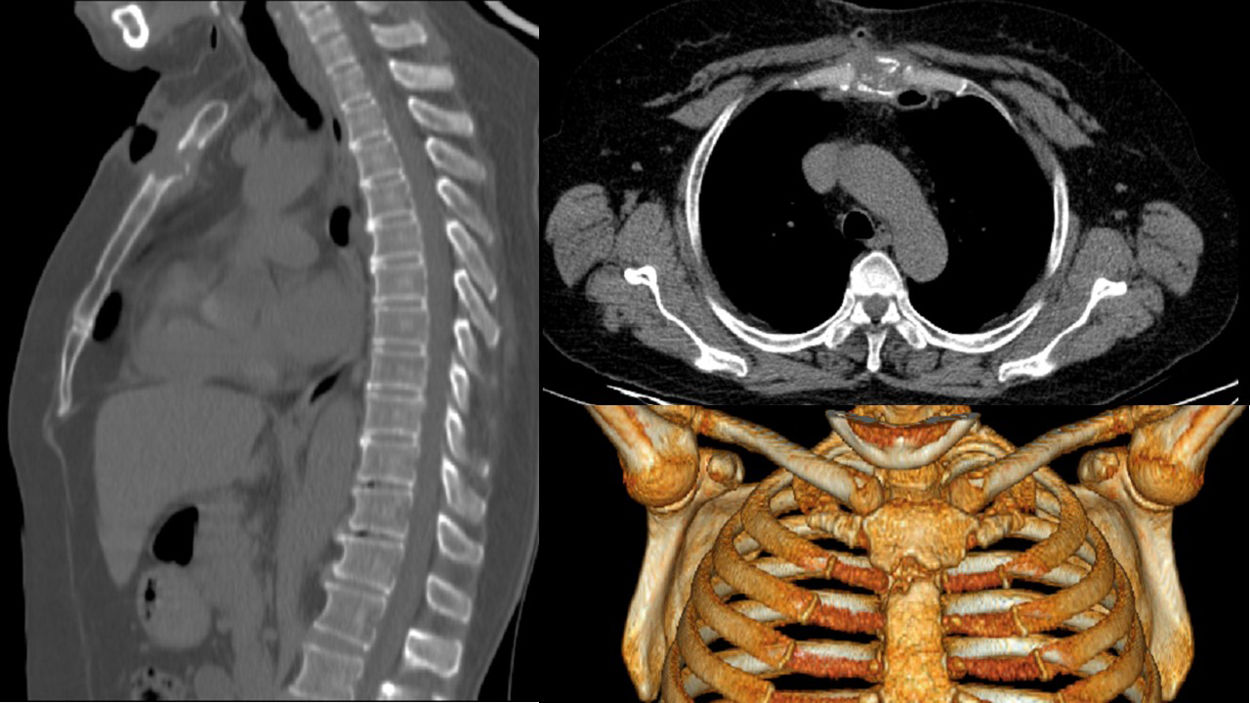
The wound failed to heal and suppuration of purulent fluid persisted, so a computed tomography (CT) scan of the chest was requested (Fig. 1), which revealed a soft tissue tumor located in the pre- and retrosternal region measuring 55×45×46mm, with heterogeneous uptake of contrast medium, areas of necrosis, and a pathological fracture of the sternum, with no pulmonary parenchymal involvement. On the basis of the tomographic findings, a surgical biopsy was performed, and specimens were sent for culture, KOH, PCR for tuberculosis (Xpert® MTB/RIF), and pathology studies, all of which were negative. The wound still failed to heal despite multiple attempts to close it, and the patient developed fever (38°C), so intravenous broad-spectrum antibiotic treatment was started, and the dose of prednisone was reduced (7.5mg/day), with partial clinical outcomes (resolution of fever, but no closing of the wound).
Given the patient's lack of progress and the high suspicion of a malignant tumor of the sternum, the CT was repeated, showing an increase in the size of the lesion. We performed a complete resection of the sternal tumor with reconstruction of the anterior chest wall with bilateral pectoralis major flaps. The surgical specimen was sent to pathology, and the report identified a granulomatous reaction with formation of caseifying granulomas and positive PCR for tuberculosis (Xpert® MTB/RIF). The results of the cultures confirmed the diagnosis of tuberculosis (growth of 17 colonies), sensitive to rifampicin (R), pyrazinamide (Z), ethambutol (E), and isoniazid (H).
The patient was treated with a 2 HREZ 4 HR regimen, and her symptoms improved within a few weeks of starting. The first phase of treatment has now been completed, with good progress and complete closure of the wound.
Tuberculosis of the sternum is a rare entity, with about 25 cases reported in the literature. Twenty of these were in developing countries, especially India, and 5 cases in developed countries. It is more common in men (16 men compared to 9 women) and 6 cases were associated with significant comorbidities. The age of presentation was variable, ranging from a child of 9 months to a patient of 74 years. Most cases are associated with lung infections, cardiac surgeries, vaccination with BCG, and immunosuppression, as was the case with our patient.1–5
Sternal involvement is believed to be due to hematogenous spread from a primary focus in the lung, but only in 4 cases could another location in addition to the sternal site be identified. In our patient, it is possible (although not confirmed) that the etiology of her adrenal insufficiency was also tuberculous.1,2
Most patients consult with a history of months of clinical symptoms, characterized by a painful sternal tumor, sometimes with the formation of fistulas, fever, profuse sweating, weight loss, or spontaneous sternal fracture, as was the case with our patient.1,2
Chest X-ray is generally not very useful, whereas CT and magnetic resonance imaging (MRI) techniques are more useful for characterizing the lesion. Cortical thickening with periosteal reaction, osteomyelitis, and heterogeneous tumors of soft tissues can be seen on CT, in addition to inflammation of the medullary cavity of the sternum characterized by low intensity images in T2 on MRI. The definitive diagnosis is performed by analyzing the sternal tissue, but this tends to be complicated and more than 1 complementary method is often required. In the published cases, diagnosis was by histopathology in 11 cases, by polymerase chain reaction in 5 (90% sensitivity and 80% specificity), by culture in 5, and positive smears in 4.2–11
The aim of treatment is to cure TB and prevent bone deformities. It is based on the use of rifampicin (R), pyrazinamide (Z), ethambutol (E), and isoniazid (H) in a regimen of 2 HREZ plus 4–10 months of HR. In general, the regimen is the same as for pulmonary tuberculosis, with or without surgical debridement of lesions (only 7 published cases required surgery).1–14
In conclusion, we report the case of an immunosuppressed patient who presented tuberculosis of the sternum with no pulmonary focus. This presentation is very rare, but it must be taken into account among the differential diagnosis of sternal tumors.
Please cite this article as: Vélez NP, Cabrera OL, Carrasco MT, Albornoz JV, Calle JCO. Lesión lítica esternal por tuberculosis. Arch Bronconeumol. 2020;56:260–261.