The pandemic caused by the coronavirus and its resulting infection, COVID-19, has had a major impact in all areas of Spanish public health. Despite social distancing and confinement (enforced to varying degrees in different countries), we are still suffering the consequences of the outbreak and will continue to do so for the rest of the year.
Each hospital contends with the pandemic at different levels. Reference centers, which have a greater number of cases, have had to vacate wards and intensive care units to make room for patients infected with the coronavirus, so the impossibility of transferring surgical patients from regional to tertiary hospitals to receive specialized care and the waiting list delays caused by the suspension of scheduled operations will soon have an impact on patients with lung cancer (LC) not infected by this virus.
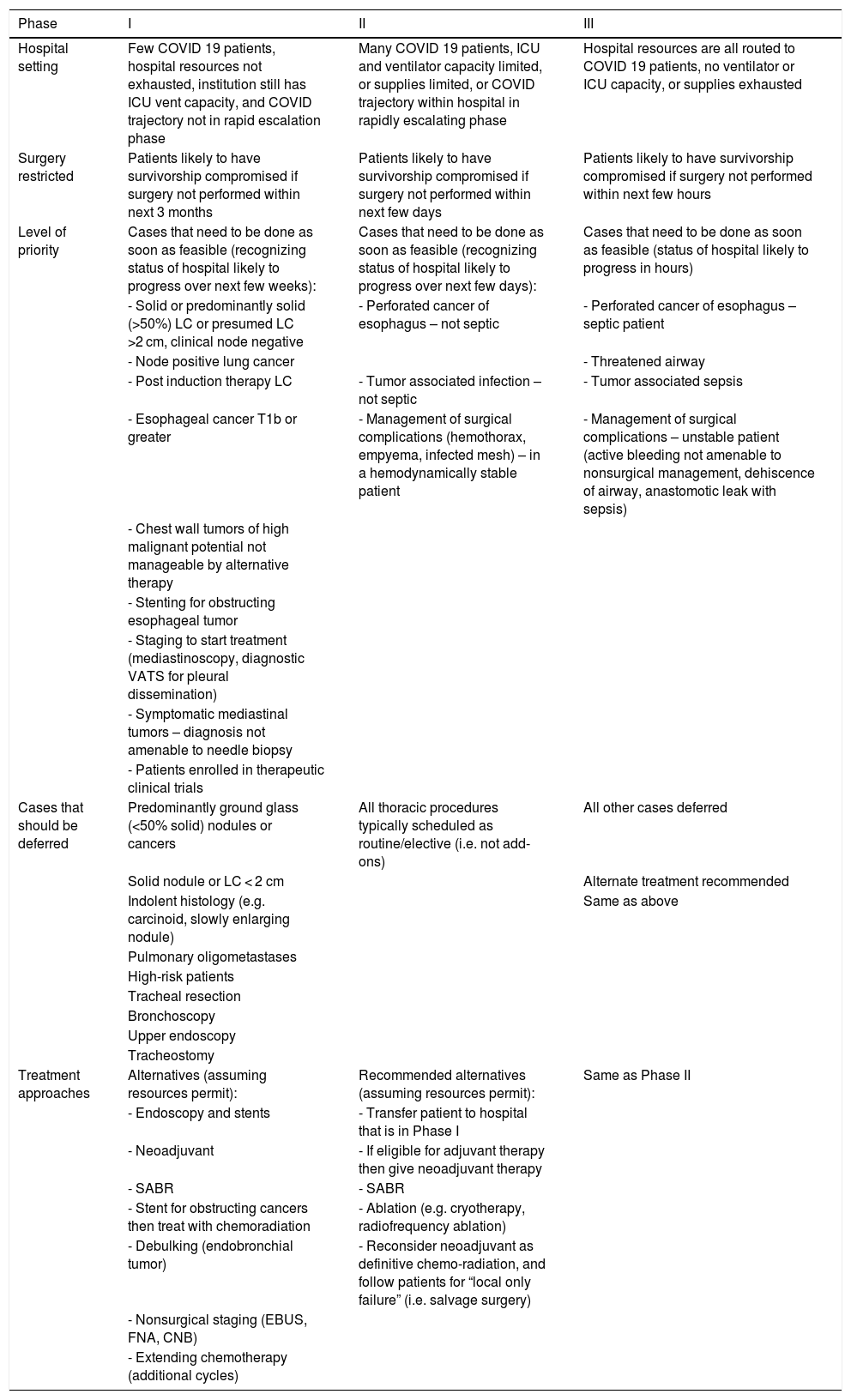
The American College of Surgeons (ACS),1 in their recently published guidelines on the management of patients scheduled for thoracic surgery, categorize the general status of hospitals into 3 phases according to the number of COVID-19 patients admitted: phase 1 - preparation; phase 2 - urgent setting; and phase 3 - extreme emergency (Table 1). In these guidelines, priority is given to patients with a life-threatening emergency (perforated cancer, tumor-associated infection or surgical complications), a histological diagnosis of cancer, greater disease extension, symptomatic patients, or patients enrolled in clinical trials. Alternative, non-surgical treatment approaches should also be considered.
Summary of COVID-19 guidelines for triage of thoracic surgery patients.
| Phase | I | II | III |
|---|---|---|---|
| Hospital setting | Few COVID 19 patients, hospital resources not exhausted, institution still has ICU vent capacity, and COVID trajectory not in rapid escalation phase | Many COVID 19 patients, ICU and ventilator capacity limited, or supplies limited, or COVID trajectory within hospital in rapidly escalating phase | Hospital resources are all routed to COVID 19 patients, no ventilator or ICU capacity, or supplies exhausted |
| Surgery restricted | Patients likely to have survivorship compromised if surgery not performed within next 3 months | Patients likely to have survivorship compromised if surgery not performed within next few days | Patients likely to have survivorship compromised if surgery not performed within next few hours |
| Level of priority | Cases that need to be done as soon as feasible (recognizing status of hospital likely to progress over next few weeks): | Cases that need to be done as soon as feasible (recognizing status of hospital likely to progress over next few days): | Cases that need to be done as soon as feasible (status of hospital likely to progress in hours) |
| - Solid or predominantly solid (>50%) LC or presumed LC >2 cm, clinical node negative | - Perforated cancer of esophagus – not septic | - Perforated cancer of esophagus – septic patient | |
| - Node positive lung cancer | - Threatened airway | ||
| - Post induction therapy LC | - Tumor associated infection – not septic | - Tumor associated sepsis | |
| - Esophageal cancer T1b or greater | - Management of surgical complications (hemothorax, empyema, infected mesh) – in a hemodynamically stable patient | - Management of surgical complications – unstable patient (active bleeding not amenable to nonsurgical management, dehiscence of airway, anastomotic leak with sepsis) | |
| - Chest wall tumors of high malignant potential not manageable by alternative therapy | |||
| - Stenting for obstructing esophageal tumor | |||
| - Staging to start treatment (mediastinoscopy, diagnostic VATS for pleural dissemination) | |||
| - Symptomatic mediastinal tumors – diagnosis not amenable to needle biopsy | |||
| - Patients enrolled in therapeutic clinical trials | |||
| Cases that should be deferred | Predominantly ground glass (<50% solid) nodules or cancers | All thoracic procedures typically scheduled as routine/elective (i.e. not add-ons) | All other cases deferred |
| Solid nodule or LC < 2 cm | Alternate treatment recommended | ||
| Indolent histology (e.g. carcinoid, slowly enlarging nodule) | Same as above | ||
| Pulmonary oligometastases | |||
| High-risk patients | |||
| Tracheal resection | |||
| Bronchoscopy | |||
| Upper endoscopy | |||
| Tracheostomy | |||
| Treatment approaches | Alternatives (assuming resources permit): | Recommended alternatives (assuming resources permit): | Same as Phase II |
| - Endoscopy and stents | - Transfer patient to hospital that is in Phase I | ||
| - Neoadjuvant | - If eligible for adjuvant therapy then give neoadjuvant therapy | ||
| - SABR | - SABR | ||
| - Stent for obstructing cancers then treat with chemoradiation | - Ablation (e.g. cryotherapy, radiofrequency ablation) | ||
| - Debulking (endobronchial tumor) | - Reconsider neoadjuvant as definitive chemo-radiation, and follow patients for “local only failure” (i.e. salvage surgery) | ||
| - Nonsurgical staging (EBUS, FNA, CNB) | |||
| - Extending chemotherapy (additional cycles) |
LC: lung cancer; CNB: coarse needle biopsy; EBUS: endobronchial ultrasound; FNA: fine needle aspiration; ICU: intensive care unit; MV: mechanical ventilation; N: nodes; SABR: stereotactic ablative radiotherapy.
As a result of this situation, LC patients will receive non-standard treatment that will lead to uncertainties in terms of overall disease-free survival.
The Society of Surgical Oncology2 also issued a message from its president that contained certain recommendations to consider in the treatment of these patients. As in the case of the ACS, hospitals are urged to consider "triage" for a number of reasons, such as the potential shortage of qualified personnel and the potential lack of materials and beds due to these resources being diverted to treat patients with COVID-19. A very recent retrospective review3 of COVID-19-affected cancer patients reported that most (25%) of the 28 patients in the series had LC. The symptoms they presented were fever (23, 82.1%), dry cough (22, 81%) and dyspnea (14, 50.0%), together with lymphopenia (23, 82.1%), raised C-reactive protein (CRP) (23, 82.1%), anemia (21, 75.0%), and hypoproteinemia (25, 89.3%). As can be seen, several of these symptoms rule out surgery in waiting list patients. The authors concluded that cancer patients show deteriorating conditions and poor outcomes, and recommend that CB patients receiving antitumor therapy should undergo vigorous screening for COVID-19 infection4,5 (clinical-epidemiological history, RT-PCR, serology), and that treatments that cause immunosuppression, including surgery, should be avoided.
What will happen to our patients who have been on the waiting list for at least 1, 2 or 3 months? Will their cancer be treated at its pre-pandemic stage? Or will supplementary testing need to be updated due to the delays in medical treatment? Will their tumor need to be restaged?
Given the characteristics of public health in our country, many hospitals might look to these recommendations for guidance. However, we believe that although the clinical guidelines published so far give us an idea of "what to do" with our waiting lists, the circumstances in each hospital will differ, and these guidelines merely offer theoretical recommendations on "what to do" or "how to do it in the best possible way". We call for guidelines that allow us to treat all patients in this situation - not only those with LC, but also those with other thoracic tumors that require surgical or multimodal treatment. Such guidelines would help us plan and treat patients currently on the waiting list within a reasonable time frame of less than 3 months.
Certain details need to be taken into account, such as the patient's willingness to undergo surgery at the current time, their family situation, or even the possibility that some patients have or have had COVID-19, in which case the best moment to re-schedule surgery must be carefully selected. On the other hand, we may need to screen all waiting list patients for coronavirus infection. What should we do? We urgently need organization, prioritization, and treatment guidelines for the future management of these patients. We need to prioritize, not only on the basis of knowledge, but also in the knowledge that we are doing the right thing.
Please cite this article as: Isea de la Viña J, Mayol J, Ortega AL, Alcázar Navarrete AN. Pacientes con carcinoma broncogénico en lista de espera en plena crisis del COVID-19: ¿y ahora qué hacemos? Arch Bronconeumol. 2020;56:602–604.