Arrhythmias and electrocardiographic abnormalities have been documented to be the first manifestation of cardiac infiltration by different tumors, including primary lung cancer.1 We describe the case of a lung cancer in the left upper lobe invading a coronary artery bypass graft (CABG) and presenting as refractory atrial flutter (AF). Interestingly, AF was the only clinical symptom prior to the suspicion and diagnostic confirmation of malignancy. Although very rare, supraventricular arrhythmias may be the presenting symptom of lung cancer, and physicians should keep this important differential diagnosis in mind when patients have an unexplained persistent supraventricular arrhythmia, especially in cardiac patients with risk factors for lung cancer.
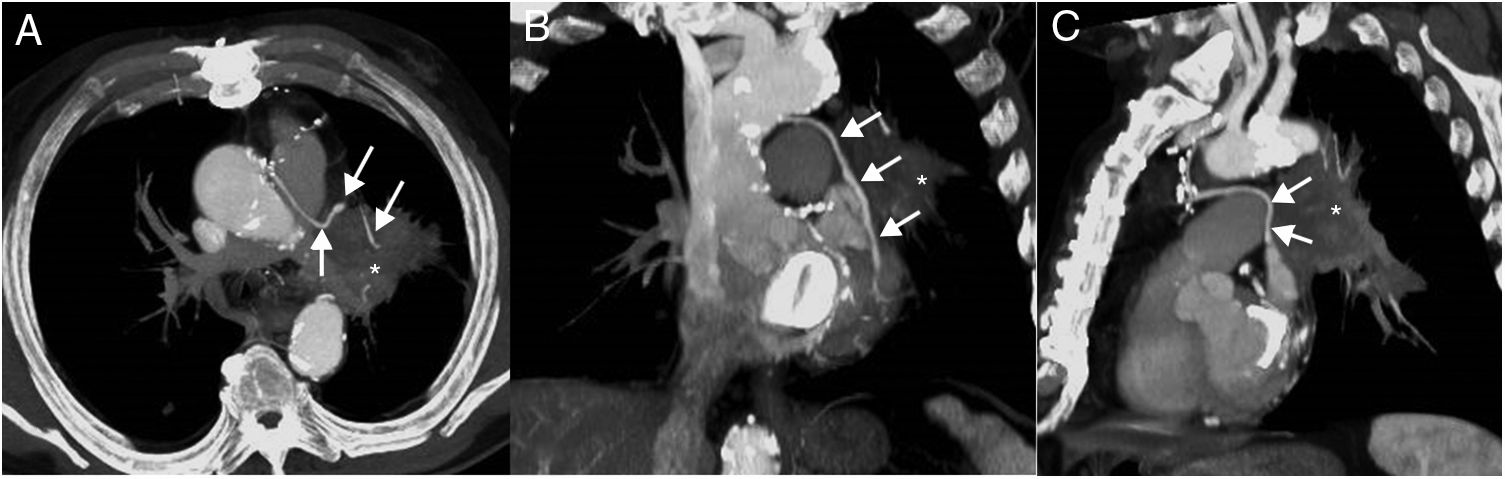
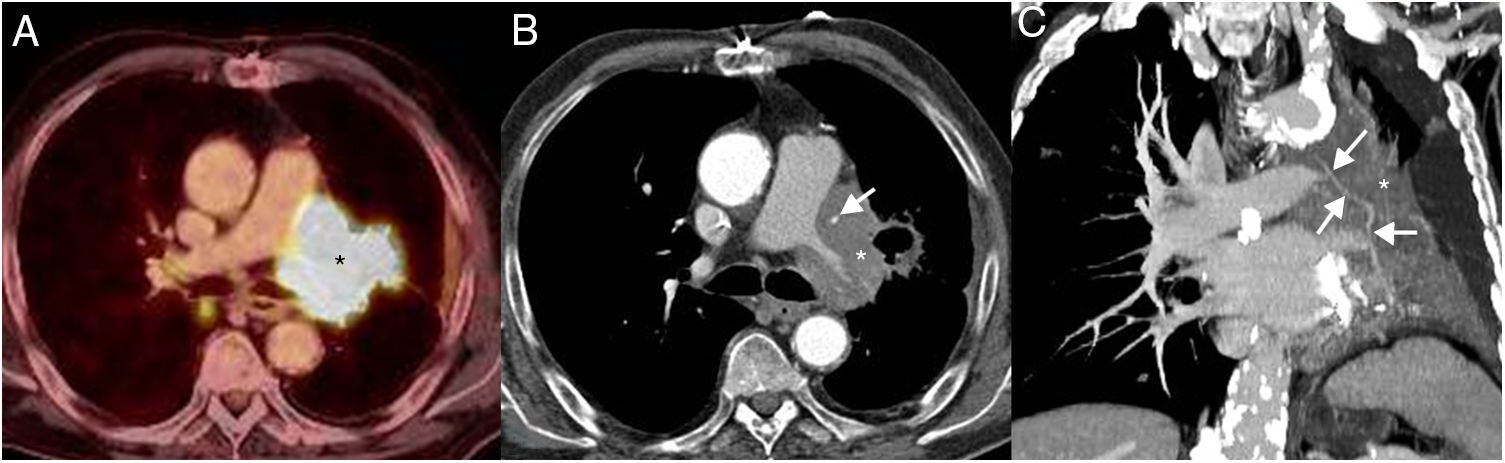
A 70-year-old ex-smoker man (45 pack-year history of smoking; quit smoking 4 years earlier) presented to our hospital with a new-onset symptomatic AF. His past medical history was significant for coronary artery disease (treated with CABG four years earlier), mitral valve disease (treated with mitral valve replacement at the same time of the CABG), hyperlipidemia, and chronic obstructive pulmonary disease. Since the AF episodes became persistent in spite of medical treatment, a cavotricuspid isthmus (CTI) ablation was planned. The CTI ablation procedure was successful for controlling the patient's AF. A chest radiograph performed at that time showed a subtle left parahilar opacity that was presumed to be of infectious origin (Fig. 1); however, given the absence of thoracic symptoms, a thoracic computed tomography (CT) was recommended. A chest CT was performed 2 weeks later and showed a left hilar mass invading the mediastinum and the left internal mammary artery (LIMA) graft to the left anterior descending coronary artery, consistent with a lung cancer (Fig. 1). The patient denied any chest pain, hemoptysis or coughing in the previous weeks, and an electrocardiogram (ECG) performed at that time (post-CTI) did not show any abnormalities. A bronchoscopic biopsy confirmed a large cell undifferentiated lung carcinoma. A contrast-enhanced whole-body positron emission tomography (PET)/CT detected small liver and adrenal metastases, consistent with a stage IV lung cancer. The patient was started on systemic chemotherapy, but unfortunately the cancer did not respond to treatment. A follow-up PET/CT performed 3 months later showed an increase in the size of the lung mass, a decrease in the diameter of the LIMA graft secondary to an encasement by the surrounding tumor (Fig. 2). Shortly after this follow-up study, the patient presented to the Emergency Department with tachycardia, chest pain, a new ST elevation on ECG in the precordial and lateral leads, and elevation of cardiac troponin levels, consistent with an extensive myocardial infarction. The patient was admitted to the oncology unit and died from cardiac arrest 24h later.
Axial fused PET/CT image (A) demonstrates a hypermetabolic mass (asterisk). Axial CT image (mediastinal window) from the CT portion of the PET/CT (B) study shows an increase in the size of the left hilar mass (asterisk) and a greater secondary encasement of the left internal mammary artery graft (arrow) with respect to the previous imaging study. Coronal CT image (mediastinal window) from the CT portion of the PET/CT (C) better depicts the encasement of the coronary artery bypass graft (arrows) by the mass (asterisk).
Arrhythmias and electrocardiographic abnormalities, although rare, have been documented to be the first manifestation of cardiac infiltration by different tumors.1 AF is well known to be associated with a variety of medical conditions, such as valvular heart disease, coronary artery disease, aging, hypertension, or thyroid dysfunction, among others.2 However, AF associated with lung cancer has been rarely reported.3 What makes our case unique compared with previous cases is that AF was the only clinical symptom prior to the suspicion and diagnostic confirmation of malignancy. We hypothesize that the possible pathogenesis of AF occurring in this patient could be the ischemic effect on the electric activity of the heart of the stenotic CABG by the encasing lung cancer as well as the enhanced micro-reentry activity when cancer cells infiltrate the left superior pulmonary vein and/or the left atrium.
Although very rare, supraventricular arrhythmias may be the presenting symptom of lung cancer. We believe that physicians should keep this important differential diagnosis in mind when patients have an unexplained persistent AF, especially in cardiac patients with risk factors for lung cancer.