The aim of this study was to analyze current data on the population's level of knowledge about COPD and to evaluate certain diagnostic interventions, such as the use of spirometry.
Material and methodsAn epidemiological, observational, cross-sectional study by telephone interview, with random dialing of landline telephone numbers, was conducted in November 2019, in a nationally representative sample of adults over 40 years of age.
ResultsFrom a total of 51,079 telephone calls, a total of 1920 individuals responded. Mean age was 61.9 years and 31.6% were men. Overall, 19.4% were current smokers and 13.4% reported respiratory disease (5% reported COPD). In total, 27.9% had spontaneous knowledge of COPD, which is a relative increase from the 17% observed in 2011. The most frequent information channel was the media (35.5%), with a significant presence of social networks and the Internet (25.7%). Almost one fifth (18.1%) had chronic respiratory symptoms. Of these, 59.3% had requested medical care, and 66.2% had undergone spirometry. Spirometry was performed less frequently in subjects treated in primary care compared to respiratory medicine departments (51.9% versus 79.1%; P < .001).
ConclusionsKnowledge of COPD is still scarce, and strategies are needed to increase awareness and the importance of assessing respiratory symptoms and increased use of spirometry.
El objetivo de este estudio es analizar los datos actuales del nivel de conocimiento de la población sobre la EPOC y evaluar algunas actuaciones diagnósticas, como el uso de espirometría.
Material y métodosEstudio epidemiológico, observacional y transversal mediante entrevista telefónica, con marcación aleatoria de números de teléfono fijos, realizado en noviembre del 2019, con una muestra representativa a nivel nacional en adultos mayores de 40 años.
ResultadosDe un total de 51079 contactos telefónicos se obtuvo un total de 1920 encuestados. La edad media era 61,9 años con 31,6% de hombres. 19,4% eran fumadores actuales y un 13,4% referían tener alguna enfermedad respiratoria (5% referían una EPOC). El 27,9% tenía conocimiento espontáneo sobre la EPOC, lo que supone un aumento relativo respecto al 17% observado en el 2011. El canal de información más frecuente eran los medios de comunicación (35,5%), con importante presencia de redes sociales e internet (25,7%). Un 18,1% tenían síntomas respiratorios crónicos. De ellos, un 59,3% solicitaron atención médica, y 66,2% se realizó la espirometría. La espirometría era realizada con menor frecuencia en sujetos atendidos en atención primaria respecto a neumología (51,9% versus 79,1%; P < .001).
ConclusionesEl conocimiento de la EPOC es todavía escaso, y son necesarias estrategias para aumentar la concienciación y la importancia de evaluar los síntomas respiratorios y el mayor uso de la espirometría.
Chronic obstructive pulmonary disease (COPD) is a health problem of the first magnitude due to its high prevalence and mortality and heavy health and social welfare burden, yet the rate of underdiagnosis remains significant1,2.
The IBERPOC study3, conducted in Spain in 1997, revealed that 78.2% of study cases confirmed by spirometry had no previous diagnosis of COPD. The EPISCAN I study4 carried out 10 years later reported an underdiagnosis rate of 73%, while the preliminary results of the recent EPI-SCAN II study5, also conducted in Spain, suggest that this trend will continue and could reach a rate of 81.7%. This represents a significant proportion of patients who, due to a lack of diagnosis, are not receiving specific treatment and active interventions for the prevention of infections and smoking cessation that would improve their prognosis.
The factors that affect this underdiagnosis are multiple and complex, and greater insight into the issues involved will lead to the implementation of efficient strategies for improving COPD diagnosis based on encouraging the public to recognize and prioritize symptoms and to seek healthcare, while raising awareness among health professionals of the need to evaluate respiratory symptoms by requesting spirometry.
Studies conducted in Spain in 20056 and 20117 revealed that knowledge of COPD is limited, that many people with respiratory symptoms do not seek medical attention, and that spirometry was underused. In the last 10 years, scientific societies and health authorities have conducted strategic interventions, including public awareness and outreach campaigns, and have implemented training programs and provided equipment to improve the practice of spirometry. However, in spite of these actions, the preliminary data of the EPI-SCAN II study5 suggest that underdiagnosis remains a problem.
The aim of this study was to update our information on the level of knowledge of COPD and associated diagnostic interventions among the general population and to compare the results with the available evidence.
MethodologyCONOCEPOC II is an epidemiological, observational, cross-sectional study sponsored by the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR) and conducted in November 2019. The design was identical to that of the studies carried out in 20056 and 20117, and consisted of a telephone survey conducted in all regions of Spain. Participation was voluntary, confidential and anonymous, and data were collected by calling landline telephone numbers at random.
Subject selectionThe inclusion criteria were men and women aged 40 years and over who agreed to complete a telephone questionnaire. Sampling was carried out according to the following stratification criteria: age according to 10-year groups (40−50, 51−60, 61−70 and >70 years) and population strata (rural: ≤10,000 inhabitants; and urban: >10,000 inhabitants). Data sets equally distributed by age and place of residence were obtained from the 5 established geographical areas (southern region: Andalusia, Extremadura, and the Canary Islands; northern region: Asturias, Cantabria, Galicia, La Rioja, Navarra, and the Basque Country; eastern region: Catalonia and Aragon; western region: Valencia, Balearic Islands, and Murcia; and central region: Castille-La Mancha, Castille and Leon, and Madrid), with a total of 384 responses from each region. The distribution of respondents by provinces is shown in Appendix 1 (Annex 1). This sample size allowed us to accurately estimate population size by geographic area for a 5% error and an 80% power for a 5% or greater prevalence of different variables. Thus, the overall sample is representative of the country as a whole and of each geographical region.
Field workTelephone interviews were organized by Saatchi & Health and conducted by trained, qualified interviewers. Calls were placed between 14:00 h and 21:30 h on weekdays, and each interview lasted approximately 15 min. After dialing landline telephone number at random in the relevant geographical area, several things could happen: if the number did not correspond to a residence or home, that number was randomly replaced; if no-one answered after a maximum of 4 attempts, the call was considered a non-contact; another possibility was refusal to participate. Finally, if an eligible person was absent when the call was placed, the number was recorded and then called back on the day or at the time the participant was expected to be at home.
Data collectionThe questionnaire on respiratory symptoms and diagnoses used in the survey was based on the European Commission for Steel and Coal (ECSC) questionnaire8 translated and validated in Spanish, to which questions on knowledge of COPD, use of spirometry, and perception of severity of other chronic diseases were added, as in the previous studies6,7. Spontaneous knowledge of COPD was assessed by asking interviewee what they knew about the disease, without any guidance from the interviewer. Respondents who demonstrated a spontaneous knowledge of COPD were asked to list the symptoms that are directly related to the disease. “Suggested” knowledge of COPD was investigated in respondents who had no spontaneous knowledge of the disease. Perceived level of health and disease severity was assessed on a scale of 0–10 points, where the higher the score, the greater the perceived health and severity level. Breathlessness was assessed by the modified Medical Research Council (mMRC) scale9. Questions on new forms of tobacco use were also included. The full questionnaire can be found in Appendix 2 (Annex 2).
Statistical analysisIn the descriptive analysis, qualitative variables are presented with their frequency distribution; quantitative variables are summarized with their mean and standard deviation (SD); and quantitative variables showing an asymmetric distribution are summarized with the median and interquartile range. Comparisons are made between study groups (by smoking history, spirometry, and reported diagnosis of COPD, including the terms “emphysema” and “chronic bronchitis”). A high risk of COPD was defined as an accumulated tobacco consumption of at least 20 pack-years with reported chronic respiratory symptoms in subjects aged 55 years or older. The association between qualitative variables was evaluated with the chi-squared (χ2) test or Fisher's exact test, if more than 25% of expected frequencies were less than 5. For quantitative variables, mean values were compared using the Student’s t-test or ANOVA variance analysis (in groups with more than 2 categories) or the Mann-Whitney U test or the Kruskall-Wallis test (in groups with more than 2 categories) when quantitative variables did not conform to a normal distribution. A multinominal regression was performed to predict the level of knowledge. All statistical comparisons with a probability of error of less than 5% were considered significant. Data processing and analysis were performed using the IBM SPSS Statistics V21 statistical package (IBM Corporation, Armonk, NY, USA).
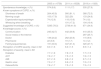
ResultsA total of 51,079 telephone calls were placed, and 8788 homes with adults over the age of 40 were identified, yielding a final sample of 1920 participants, with a response rate of 21.8%. The STROBE flow diagram is shown in Fig. 1.
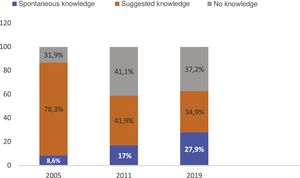
Population characteristicsOverall, 31.6% participants were men, and the mean age was 61.9 years; 14.5% were current smokers and 4.5% had tried other forms of tobacco consumption. A total of 13.4% reported having respiratory disease, including 5% who reported COPD. The clinical and demographic characteristics of the individuals surveyed are presented in Table 1.
Clinical and demographic characteristics of the survey population.
| Total (n = 1920) | |
|---|---|
| Men, n (%) | 607 (31.6) |
| Age (years), mean ± SD | 61.9 ± 13.5 |
| Smoking history | |
| Accumulated exposure (pack-years), mean ± SD | 21.0 ± 22.7 |
| Never smokers, n (%) | 1136 (59.2) |
| Former smokers, n (%) | 505 (26.3) |
| Active smokers, n (%) | 279 (14.5) |
| Have you ever tried other forms of smoking? n (%) | 87 (4.5) |
| Perceived level of healtha, mean ± SD | 7.4 ± 1.8 |
| Reports having some respiratory disease, n (%) | 258 (13.4) |
| Reports respiratory disease, n (%) | |
| COPD | 99 (5) |
| Asthma | 67 (3.5) |
| Other | 94 (4.9) |
| Reports some chronic respiratory symptoms, n (%) | 354 (18.4) |
Data expressed as mean ± standard deviation or by absolute (relative) frequencies depending on the nature of the variable.
A total of 354 (18.4%) participants reported at least 1 chronic respiratory symptom, a third of whom reported 2 or more symptoms. Shortness of breath was reported by 13.1% of the respondents. The percentage of individuals with respiratory symptoms was higher among current and former smokers (P < .001). Over half (59.9%) of the active smokers had attempted to quit, with 3.1 ± 4.6 (mean ± SD) attempts; 19.7% of the active smokers reported having tried some other form of tobacco use compared with 5% of the former smokers (P < .01). Overall, 20.4% of active smokers vs. 12% of former smokers believe that alternatives to conventional smoking can help stop the habit (P < .05).
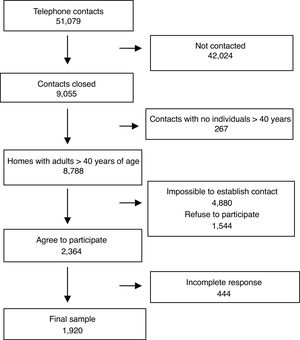
Among respondents who reported respiratory symptoms, 210 (59.3%) had seen a doctor, more often in primary care (61.4%) than in the respiratory medicine department (38.6%), and 45 (12.7%) reported attending the emergency department for respiratory problems. Spirometry had been performed in 139 (62.2%) respondents who reported respiratory symptoms and had consulted a doctor. No geographical differences were detected in reported clinical management. The clinical and demographic characteristics of the individuals surveyed are shown in Table 2.
Characteristics of survey respondents according to smoking history.
| Total (n = 1920) | Never smokers (n = 1136) | Former smokers (n = 505) | Active smokers (n = 279) | |
|---|---|---|---|---|
| Sex (men), n (%) | 607 (31.6) | 246 (21.7) | 250 (49.5)b,c | 111 (39.8)e |
| Age (years), mean ± SD | 61.9 ± 13.5 | 63.6 ± 14.2 | 61.5 ± 12.2a,d | 55.9 ± 10.6 f |
| Pack-years, median (P25−75) | 15 (5−30) | – | 15 (5−30) | 17.7 (6−22.5) |
| Attempted smoking cessation, n (%) | – | – | – | 167 (59.9) |
| No. of attempts, mean ± SD | 3.15 ± 4.61 | |||
| Have you tried other forms of smoking? n (%) | 87 (4.5) | 7 (0.6) | 25 (5)b,d | 55 (19.7)f |
| Electronic cigarette | 56/87 (64.4) | 4/7 (57.1) | 15/25 (60) | 37/55 (67.3) |
| Vaping | 16/87 (18.4) | 1/7 (14.3) | 2/25 (8) | 13/55 (23.6) |
| Attitude regarding alternatives to conventional smoking (%) | ||||
| Very favorable | 0.4 | 0.4 | 0.6 | 0 |
| Favorable | 6.5 | 5.5 | 5.9 | 11.8 |
| Not known | 38.8 | 43.3 | 34.5 | 28.7 |
| Unfavorable | 34.3 | 30.5 | 38.8 | 41.9f |
| Very unfavorable | 19.9 | 20.4 | 20.2 | 17.6 |
| Do you think they can help quit smoking? (%) | ||||
| Yes | 12.8 | 11.3 | 12c | 20.4f |
| No | 55.4 | 50.6 | 62.4 | 62.4 |
| Don’t know | 31.8 | 38.1 | 25.5 | 17.2 |
| Do you think they have health risks? (%) | ||||
| Yes | 60.9 | 56.8 | 64.3 | 71.7 |
| No | 9.5 | 10.4 | 8.7 | 7.5 |
| Don’t know | 29.6 | 32.8 | 26.9 | 20.8 |
| Reports some chronic respiratory symptoms, n (%) | 354 (18.4) | 170 (15) | 104 (20.6)b,d | 80 (28.7)f |
| No. of respiratory symptoms (%) | ||||
| 0 | 81.6 | 85 | 79.4b,d | 71.3f |
| 1 | 12.5 | 10.7 | 14.9 | 15.8 |
| 2 | 2.5 | 1.9 | 2.4 | 5.4 |
| 3 | 2.1 | 1.3 | 2.4 | 4.7 |
| 4 | 1.4 | 1.1 | 1 | 2.9 |
| Respiratory symptoms, n (%) | ||||
| Chronic cough | 133 (5.9) | 49 (4.3) | 30 (5.9)d | 34 (12.2)f |
| Chronic expectoration | 102 (5.3) | 40 (3.5) | 31 (6.1)a,c | 31 (11.1)f |
| Wheezing or noises in the chest | 93 (4.8) | 44 (3.9) | 23 (4.6)d | 26 (9.3)f |
| Shortness of breath | 253 (13.1) | 127 (11.2) | 71 (14)a,c | 54 (19.3)e |
| Has a sensation of breathlessness when walking on the flat or at rest, n (%) | 119 (6.2) | 69 (6) | 29 (5.7) | 20 (7.2) |
| Has seen the doctor, n (%) | 210 (10.9) | 107 (9) | 61 (12) | 42 (15) |
| Family doctor | 129/210 (61) | 69/107 (64.5) | 33/61 (54.1) | 27/42 (64.3) |
| Pulmonologist | 81/210 (38.6) | 38/107 (35.5) | 28/61 (45.9) | 15/41 (35.7) |
| Has performed spirometry at some time, n (%) | 139 (7.2) | 61 (5.4) | 48 (9.5)b | 30 (10.8) |
| Has gone to the emergency department for respiratory problems, n (%) | 45 (2.3) | 27 (2.4) | 13 (2.6) | 5 (1.8) |
| Perceived level of health, mean ± SD | 7.41 ± 1.88 | 8.53 ± 1.48 | 8.62 ± 1.30 | 8.63 ± 1.59 |
Data expressed as mean ± standard deviation or by absolute (relative) frequencies depending on the nature of the variable.
Analysis of the diagnostic circuit of respondents with respiratory symptoms shows little improvement over previous studies in 2005 and 2011 (Fig. 2).
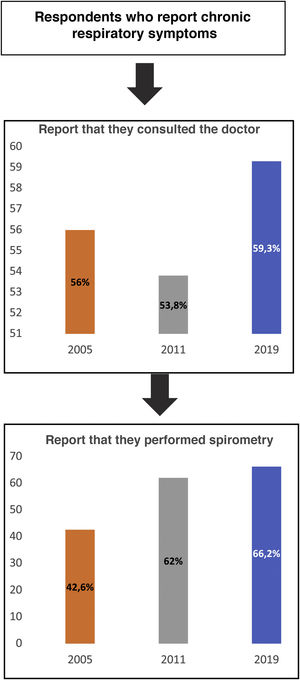
Use of spirometryThe use of spirometry differed significantly depending on sex and smoking history. Respondents who reported having performed a spirometry were more often men, had a history of smoking, and met criteria for a high risk of COPD than those who did not perform a spirometry (P < .001). There were also differences depending on the treating specialist: 79.1% of those treated by a pulmonologist reported having performed spirometry compared with 51.9% of those seen by a family doctor (P < .001) (Table 3) (Fig. 3).
Characteristics of patients who see the doctor for symptoms, by reported performance of spirometry.
| Total (n = 210) | Performed at least 1 spirometry (n = 139) | Never performed spirometry (n = 71) | P-valuea | |
|---|---|---|---|---|
| Sex (men), n (%) | 62 (29.5) | 48 (34.5) | 14 (19.7) | .018 |
| Age (years), mean ± SD | 62 ± 14 | 64.4 ± 13.6 | 67.7 ± 14.4 | .110 |
| Smoking history | .012 | |||
| Active smokers, n (%) | 42 (20) | 30 (21.6) | 12 (16.9) | |
| Former smokers, n (%) | 61 (9) | 48 (34.5) | 13 (18.3) | |
| Never smokers, n (%) | 107 (50.6) | 61 (43.9) | 46 (64.8) | |
| Meets criteria for high risk of COPDb, n (%) | 103 (49) | 78 (56.1) | 25 (35.2) | <.001 |
| Reports shortness of breath, n (%) | 156 (74.3) | 107 (77) | 49 (69) | .402 |
| Chronic cough | 75 (35.8) | 49 (35.3) | 26 (36.6) | .845 |
| Chronic expectoration | 66 (31.4) | 45 (32.4) | 21 (29.6) | .680 |
| Wheezing or noises in the chest | 71 (33.8) | 50 (36) | 21 (29.6) | .354 |
| Reports having some respiratory disease, n (%) | 140 (66.7) | 86 (61.9) | 17 (23.9) | <.001 |
| Have you ever attended the emergency department for worsening respiratory symptoms? n (%) | 41 (19.5) | 32 (23) | 9 (12.7) | .074 |
| Attending physician, n (%) | <.001 | |||
| Family doctor | 129 (61.4) | 67 (48.2) | 62 (87.3) | |
| Pulmonologist | 91 (38.6) | 72 (51.8) | 9 (12.7) | |
| Perceived level of health, mean ± SD | 8.7 (1.4) | 6.0 (2.0) | 6.2 (2.2) | .546 |
Data expressed as mean ± standard deviation or by absolute (relative) frequencies depending on the nature of the variable.
Ninety-six (5%) respondents reported having COPD. Of these, 20% did not report spirometry testing, although 34.4% had attended the emergency department for respiratory problems; 245 (13.4%) participants met criteria for a high risk of COPD, but did not report having COPD. These individuals were younger (63.4 ± 12.9 vs. 67.4 ± 8.4), had a higher smoking exposure measured in pack-years (43.1 ± 24.9 vs. 25.9 ± 25.2), and were more frequently active smokers (26% vs. 17.7%). Just over half (51.4%) of respondents had consulted a doctor, most often the family doctor (70.6%), but only 9.8% reported having performed spirometry, although 7.8% had attended the emergency department for respiratory problems (Table 4).
Characteristics of respondents who report having COPD and of respondents with high-risk criteria and who report not having COPD.
| Respondents reporting COPD (n = 95) | Respondents with criteria for high risk of COPDb who do not report COPD (n = 245) | P-valuea | |
|---|---|---|---|
| Sex, men, n (%) | 29 (30.2) | 126 (55.5) | <.001 |
| Age, years, mean ± SD | 67.4 ± 8.4 | 63.4 ± 12.9 | .007 |
| Smoking history | |||
| Pack-years, mean ± SD | 25.9 ± 25.2 | 43.1 ± 24.9 | |
| Never smokers (%) | 3.1 | 0 | |
| Former smokers (%) | 79.2 | 74 | |
| Active smokers (%) | 17.7 | 26 | |
| Attempted smoking cessation, n (%) | 16 (94.1) | 30 (47.5) | .001 |
| No. of attempts, mean ± SD | 2.6 ± 1.5 | 2.6 ± 1.3 | .812 |
| Have you ever tried other forms of smoking, n (%) | 7 (7.3) | 20 (8.2) | .826 |
| Do you think they can help to quit smoking (%) | 17.4 | 15 | |
| Do you think they have health risks (%) | 85.5 | 91 | |
| ≥ 2 chronic respiratory symptoms, n (%) | 43 (44.8) | 66 (27) | .001 |
| Reports a sensation of breathlessness, n (%) | 32 (33.3) | 46 (18.8) | .005 |
| Has seen the doctor, n (%) | 84 (87.5) | 126 (51.4) | .001 |
| Family doctor (%) | 36.1 | 70.6 | .005 |
| Pulmonologists (%) | 63.9 | 29.4 | |
| Has gone to the emergency department for respiratory problems, n (%) | 33 (34.4) | 19 (7.8) | <.001 |
| Has performed spirometry at some time, n (%) | 80 (83.3) | 24 (9.8) | <.001 |
| Receives treatment for respiratory symptoms, n (%) | 76 (79.2) | ||
| Inhalers | 74 (97.4) | ||
| Oral | 2 (2.6) | ||
| Oxygen therapy | 15 (19.7) | ||
| Perceived level of health, mean ± SD | 6.8 (2.0) | 6.9 (2.1) | .687 |
Data expressed as mean ± standard deviation or by absolute (relative) frequencies, by nature of the variable.
Over a quarter (27.9%) of the surveyed population had a spontaneous knowledge of COPD, the most well-known symptom being breathlessness (72.5%), while 34.9% of the respondents had suggested knowledge. Among individuals with spontaneous or suggested knowledge, the most frequent sources of information were the media (35.5%), family and acquaintances (27.7%), and social media and the Internet (25.7%). The perception of COPD severity was very high, 8.5 ± 1.4, and only surpassed by angina. Some results showed a slight improvement in spontaneous knowledge compared to the results of 2011 and 2005 (Table 5).
Changes in the level of knowledge of COPD.
| 2005 (n = 6758) | 2011 (n = 6528) | 2019 (n = 1920) | |
|---|---|---|---|
| Spontaneous knowledge, n (%) | 574 (8.6) | 1111 (17) | 535 (27.9) |
| Known symptoms of COPD, n (%) | |||
| Shortness of breath | 264 (45.9) | 900 (81.1) | 388 (72.5) |
| Morning cough | 103 (17.9) | 322 (29) | 133 (24.8) |
| Expectoration/sputum/phlegm | 74 (12.9) | 118 (10.6) | 74 (1.8) |
| Wheezing when breathing | – | 191 (17.2) | 104 (19.4) |
| Suggested knowledge of COPD, n (%) | 5295 (78.3) | 2738 (41.9) | 671 (34.9) |
| Knowledge source, n (%) | |||
| Communication | 245 (42.7) | 442 (39.8) | 410 (35.5) |
| Social media or the Internet | – | – | 297 (25.7) |
| Doctor | 139 (24.2) | 262 (23.6) | 115 (9.9) |
| Pharmacist | 22 (3.8) | 19 (1.7) | 14 (1.2) |
| Family/acquaintances | 191 (33.3) | 347 (31.3) | 320 (27.7) |
| Perception of COPD severity, mean ± SD | 8.3 ± 1.6 | 8.3 ± 1.5 | 8.5 ± 1.4 |
| Perception of severity, mean ± SD | |||
| Diabetes | 7.7 ± 1.8 | 7.6 ± 1.5 | 7.7 ± 1.5 |
| AHT | 7.6 ± 1.7 | 7.5 ± 1.5 | 7.6 ± 1.5 |
| AMI | 8.7 ± 1.6 | 8.8 ± 1.2 | 8.7 ± 1.3 |
| Gastric ulcer | 7.0 ± 1.7 | 6.9 ± 1.5 | 7.0 ± 1.5 |
| Osteoarthritis | 7.8 ± 1.7 | 7.5 ± 1.5 | 7.5 ± 1.5 |
Data expressed as mean ± standard deviation or by absolute (relative) frequencies depending on the nature of the variable.
With regard to knowledge of COPD (Table 6), statistically significant differences were observed in age, place of residence, and smoking history. In the multivariate analysis, respiratory symptoms and spirometry were associated with spontaneous knowledge of COPD (P < .05) (Table 6).
Characteristics by level of knowledge of COPD.
| Total (n = 1920) | Spontaneous knowledge (n = 535) | Suggested knowledge (n = 671) | No knowledge (n = 714) | Pa |
|---|---|---|---|---|
| Sex, men, n (%) | 158 (29.5) | 224 (33.4) | 225 (31.5) | .359 |
| Age, n (%) | .003 | |||
| 40−50 years | 142 (26.5) | 173 (25.8) | 165 (23.1) | |
| 51−60 years | 145 (27.1) | 159 (23.7) | 176 (24.6) | |
| 61−70 years | 150 (28.0) | 152 (22.7) | 178 (24.9) | |
| >70 years | 98 (18.3) | 187 (27.9) | 195 (27.3) | |
| Setting < 10,000 inhabitants, n (%) | 164 (30.6) | 263 (39.2) | 322 (45.1) | <.001 |
| Smoking history, n (%) | <.001 | |||
| Never smoker | 258 (48.2) | 415 (61.8) | 463 (64.8) | |
| Former smoker | 184 (34.4) | 156 (23.2) | 165 (23.1) | |
| Active smokers | 93 (17.4) | 100 (14.9) | 86 (12.0) | |
| History of smoking (ex-smoker or active smoker), n (%) | 277 (51.8) | 256 (38.2) | 251 (35.2) | <.001 |
| Criteria for high risk of COPDb, n (%) | 85 (30.7) | 71 (27.7) | 89 (35.5) | .167 |
| Perceived level of health, mean ± SD | 7.5 ± 1.7 | 7.3 ± 1.9 | 7.4 ± 1.9 | .382 |
| Reports respiratory symptoms, n (%) | 127 (23.7)c | 111 (16.5) | 116 (16.3) | .001 |
| Reports shortness of breath, n (%) | 103 (19.3) | 67 (10) | 82 (11.5) | <.001 |
| Has performed spirometry, n (%) | 68 (12.7)c | 42 (6.3) | 29 (4) | .001 |
Data expressed as mean (standard deviation) or absolute (relative) frequencies depending on the nature of the variable.
The main outcome of this survey is that 27.9% of the Spanish adult population spontaneously know about COPD, a small increase from the 17% observed in 20117. Nevertheless, this improved knowledge does not appear to be reflected in a change in the procedures performed for the diagnosis of this disease, as only two thirds of respondents with respiratory symptoms consulted the doctor, despite COPD being perceived as a serious disease. Furthermore, the use of spirometry is limited, since only two thirds of the respondents who consulted the doctor for symptoms reported ever having performed spirometry, while respondents who reported having a diagnosis of COPD stated that they had not undergone spirometry testing, as recommended in the current guidelines10. Some authors suggest that there is still a wide gap between the public’s perception of COPD and the significant health and social welfare impact of the disease, as reflected in the latest data which show an increase in prevalence and mortality in Spain1,11,12.
A lack of knowledge of COPD is also observed in other countries. A survey conducted in Poland13 showed that only 14% of the general population had some superficial knowledge of COPD. Other studies have also shown that other collectives, such as medical students14, healthcare personnel15,16, and COPD patients themselves16,17 have very limited knowledge of the disease. These data underline the urgent need for better educational, outreach and awareness interventions. One interesting finding from our study is that more than 25% of respondents have learnt about the disease from the Internet and social networks. This channel is growing considerably as a source of awareness and scientific information, and up to 55% of Spaniards browse the Internet to search for health information, with women showing a greater preference for seeking information on health issues (11.8% more than men)18. However, the challenge is to provide valuable, reliable, and validated information. In our study, lack of knowledge was greatest in rural areas and in respondents over 70 years of age. This population may have more limited access to information sources, and is therefore a potential target of educational initiatives delivered by health professionals. It is important that health professionals, especially in primary care, use the term COPD and explain its meaning, as the expression is still unfamiliar19. This health education should be offered not only to individuals with respiratory symptoms and to patients undergoing spirometry, but also to smokers and at-risk populations. Only 9.9% of the respondents in our study reported that they had learnt about the disease from their doctors.
We also found that the importance of seeking medical attention for respiratory symptoms is underestimated and the use of spirometry is still limited, despite the fact that it should be a key tool in the diagnostic process. In our analysis, the frequency of chronic respiratory symptoms was 18.4%, somewhat lower than reported in previous studies in Spain conducted in 1999 (IBERPOC, 48%)20, 2005 (telephone survey, 24%)6, and 2011 (CONOCEPOC, 28.8%)7. This difference could be related to the lower number of current smokers (14.5%) and a higher proportion of women in our survey (68%). According to data from the 2017 National Health Survey, the smoking rate among people over 45 years of age is 20.8% (17.7% in women and 24.5% in men)21. Other factors known to influence the frequency of respiratory symptoms are educational level, place of residence, and pollution levels22,23, although these were not evaluated in our study. Another determinant for the presence of chronic respiratory symptoms may be the use of new forms of tobacco consumption. The market for these devices is growing rapidly, especially among young people and smokers who believe that they reduce the risks associated with smoking and are an aid to quitting smoking. In Spain, 9% of the population between the ages of 15 and 64 have tried them on at least 1 occasion24. In our survey, 19.7% of active smokers and 5% of former smokers used these devices: 20.4% of active smokers believe them to be an aid to smoking cessation, although 71.7% understand that they entail health risks.
Five percent of respondents reported a diagnosis of COPD, similar to the 4.8% reported 20 years ago in the IBERPOC study6, and the 5.3% reported 10 years ago in EPISCAN I7. These data show that underdiagnosis persists and is driven by many factors. Some of these are patient-related, as only 59.3% of individuals with respiratory symptoms sought medical attention, 74% of whom reported breathlessness. We found no differences according to smoking habit, although only 52.5% of active smokers with symptoms reported having seen a doctor, while almost half of the individuals at high risk for COPD had not seen a doctor.
However, underdiagnosis is also associated with the underuse of spirometry, something that occurs even in a population at high risk of COPD. Although half of these individuals had sought medical attention for respiratory symptoms, only 75% of them underwent spirometry. This is significant because COPD is highly prevalent among this group, and up to 25% may have undiagnosed COPD25. It should be noted that our sample comprises a higher percentage of women. Doctors’ level of suspicion for COPD in women has been documented to be lower, so they request fewer spirometries for this group26, contributing to a higher rate of underdiagnosis in women4.
The use of spirometry, particularly by family doctors, must increase, given the preliminary data from the EPI-SCAN II epidemiological study4, which show a prevalence of COPD of 12.4% in the population over 40 years of age and rising trends due to the gradual aging of the population and tobacco exposure.
The 3E study reported that use of spirometry was still limited27, despite a slight improvement in figures compared with studies performed more than 20 years ago28. Promoting the routine use of quality spirometry in primary care is a priority for achieving earlier diagnosis and changing the natural history of this disease, as this is the care level where the individual with risk factors or respiratory symptoms first comes into contact with the system.
Calling landline numbers at random is a methodology similar to that used in the 2005 and 2011 surveys. It is also representative of the Spanish population, which is important given the objective of analyzing changes in the knowledge of COPD among that population. However, it should be borne in mind that according to data from the 2019 survey of the National Institute of Statistics, 77% of households in Spain have a landline telephone18. Some limitations should also be considered, such as the lack of stratification by sex in the sampling process (resulting in a higher percentage of women in the sample evaluated) and a smaller sample size that, in contrast to the 2011 survey, did not take into account representativeness among the autonomous communities, thus limiting the analysis of regional variability and resulting in some small samples close to an estimated prevalence of less than 5%. We must also point out that the study evaluates self-reported, unvalidated responses, although it does provide true estimates of respiratory symptoms and diagnostic interventions reported anonymously in a large population with national representation with a response rate of 21.8%, higher than the 13.1% rate reported in the previous 2011 survey.
ConclusionsKnowledge of COPD among the Spanish population and the use of spirometry, even in high-risk subjects, is still limited, and strategies are needed to increase awareness of the disease, to emphasize the importance of assessing respiratory symptoms, and to promote the use of spirometry in primary care.
Conflict of interestsMCR has received honoraria in the past 3 years for lectures, scientific consultancy, and clinical trial participation from: Boehringer Ingelheim, Bial, Chiesi, Ferrer, Gebro, GlaxoSmithKline, Grifols, Menarini, and Novartis.
JLRH has received honoraria in the past 3 years for lectures, scientific consultancy, and clinical trial participation from: Boehringer Ingelheim, Bial, Chiesi, GlaxoSmithKline, Grifols, Menarini and Novartis.
MM has received honoraria for speaking engagements from AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, Menarini, Rovi, Bial, Sandoz, Zambon, CSL Behring, Grifols y Novartis; consultancy fees from AstraZeneca, Boehringer Ingelheim, Chiesi, Ferrer, GlaxoSmithKline, Bial, Gebro Pharma, Kamada, CSL Behring, Laboratorios Esteve, Ferrer, Mereo Biopharma, Verona Pharma, TEVA, Spin Therapeutics, pH Pharma, Novartis, Sanofi and Grifols, and research grants from GlaxoSmithKline and Grifols.
JLLC has received honoraria in the past 3 years for lectures, scientific consultancy, clinical trial participation, and writing of papers from (in alphabetical order): AstraZeneca, Boehringer Ingelheim, Chiesi, CSL Behring, Esteve, Ferrer, Gebro, GlaxoSmithKline, Grifols, Menarini, Novartis, Rovi and Teva.
Please cite this article as: Calle Rubio M, Rodríguez Hermosa JL, Miravitlles M, López-Campos JL. Conocimiento de la enfermedad pulmonar obstructiva crónica, presencia de síntomas respiratorios crónicos y uso de la espirometría en la población española: estudio CONOCEPOC 2019. Arch Bronconeumol. 2021;57:741–749.