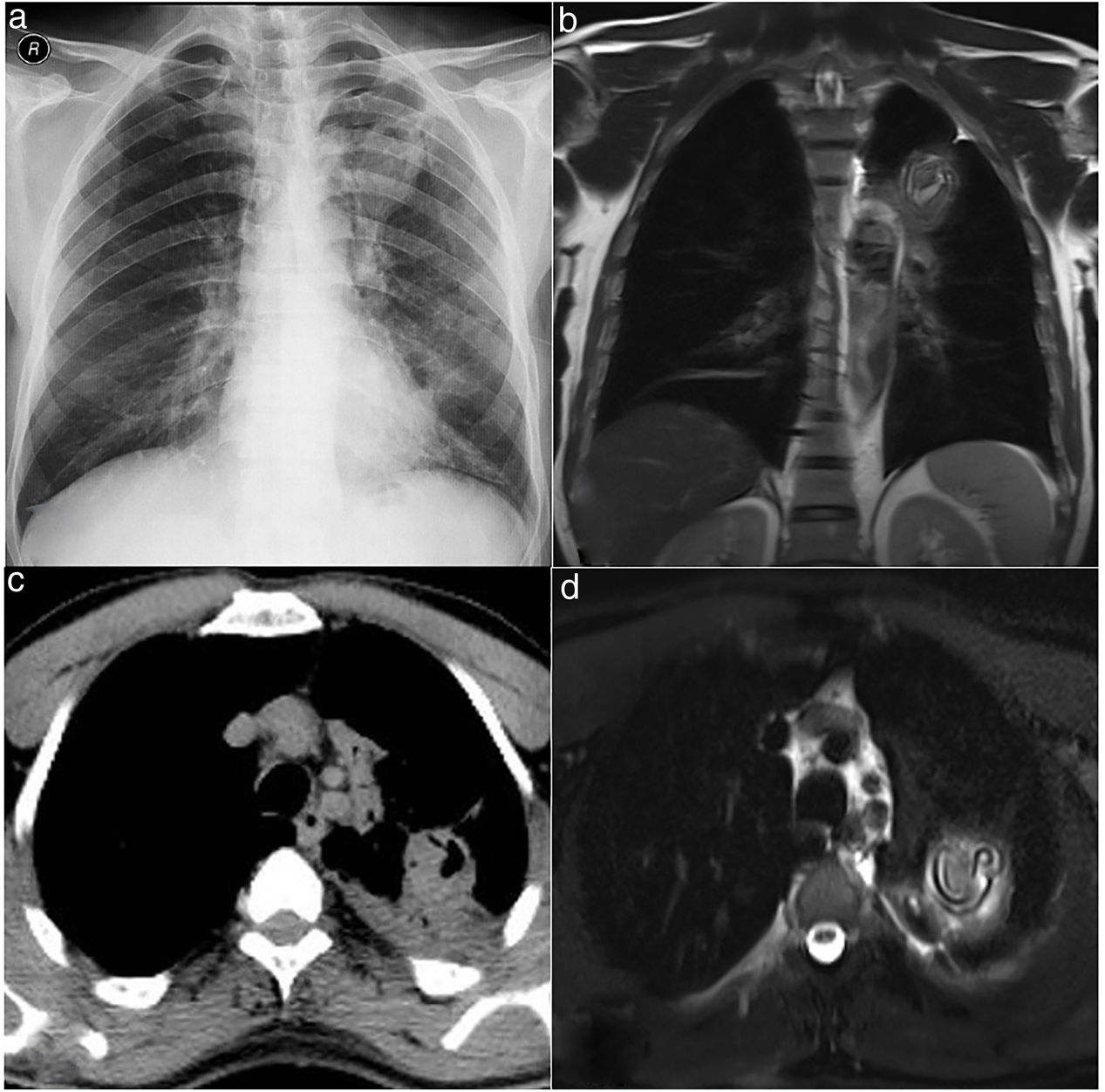
A 59-year-old male patient was admitted to the chest diseases clinic with complaints of sweating, fever and cough. The chest X-ray showed a uniform limited radiopaque area in the upper zone of the left lung. Then, the patient underwent positron emission tomography (PET)/computed tomography (CT) (PET-CT) imaging. In PET-CT, 4×5mm sized hypometabolic cavitary lesion was observed in the left lung upper lobe. Then the patient was asked for thorax tru-cut biopsy due to suspicion of malignancy. We thought that this lesion may be hydatid cyst. Because our city is one of the endemic regions. The patient was taken a contrast thoracic magnetic resonance imaging (MRI). In thoracic MRI, a 45×40×40mm sized T1 weighted imagines hypointense, T2 weighted imagines hyperintense lesion was observed (Fig. 1). There was band formation compatible with germinative membrane in the lesion. Based on these findings, we diagnosed the patient with perforated cyst hydatid. The biopsy was not taken.
(a) Chest X ray PA view showing an ill-defined radiopacity in left upper lung field. (b) T2 weighted imagines haste coronal view hyperintense lesion was observed. There was band formation compatible with germinative membrane in the lesion. (c) Positron emission tomography (PET)/computed tomography (CT) showed hypometabolic cavitary lesion was observed in the left lung upper lobe. (d) T2 weighted imagines haste axial view hyperintense lesion was observed. There was band formation compatible with germinative membrane in the lesion.
It is difficult to differentiate complicated cysts from tumor, hematoma, congenital cysts, or pneumothorax.1 Thoracic MRI may be more sensitive than CT especially malign-benign differentiation of lesions.2,3 It can be a guide before the interventional procedure.
FundingThe authors received no financial support for the research and/or authorship of this article.
Conflict of interestThe authors declare that they have no conflict of interest to the publication of this article.