We report the case of patient diagnosed with intrathoracic vagus nerve schwannoma. Vagus nerve schwannomas are highly unusual. In the last 40 years, 30 cases at most have been reported, of which only 2 have been published in Spanish.1,2
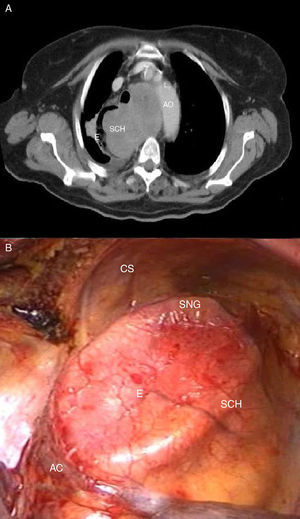
A 74-year-old woman, with no significant clinical history, presented with clinical symptoms of dry cough, asthenia and dyspnea on minimal exertion. Standard chest X-ray showed mediastinal widening, so a computed tomography (CT) was performed, revealing a posterior, retrovascular, paratracheal mass in the mediastinum measuring 9.3cm×4.3cm (Fig. 1A) extending to the carina, causing substantial dilation and right shift of the esophagus, but with no evidence of stenosis. The mediastinal mass showed pathological uptake on positron emission tomography (SUV 7.57). Endoscopic ultrasound revealed a well-defined hypoechogenic lesion, containing heterogeneous areas, 30cm from the dental arch, protruding into the submucosa. Fine needle aspiration was performed, but the specimen was insufficient for diagnosis.
Fiberoptic bronchoscopy/endobronchial ultrasound showed extrinsic posterior compression of the trachea and carina, with no infiltration. Results from ultrasound-assisted biopsy confirmed fusocellular tumor, with low-grade malignant cytology, immunohistochemical study positive for S100, and negative CD34 and CD117.
A right posterolateral thoracotomy was performed, and a 10-cm tumor was found in the posterior mediastinum, adhering closely to the supracarinal esophagus, which was severely dilated (Fig. 1B). During resection of the tumor, the tracheal membrane was torn and repaired by suturing. In view of the close adhesion of the tumor to the esophagus, the mucosa was left exposed, so a 9cm×4cm portion of the esophagus had to be resected en bloque with the tumor. The esophageal defect was repaired with separate sutures in the mucous membrane and the muscle layer. The vagus nerve could be preserved, although this was not a significant consideration in our surgical strategy. An esophageal transit study did not reveal any extravasation of contrast medium or difficulty in passage.
Diagnosis from the pathology laboratory was schwannoma extending to the tunica adventitia of the esophagus with no infiltration of the muscle layer. Surgical borders were completely free of disease.
Schwannoma is a tumor originating in the Schwann cells1 that surround the peripheral nerve fibers of the nerve roots or peripheral nerves. It accounts for 20% of mediastinal cancers in adults, but 85%–90% of all tumors of the posterior mediastinum are schwannomas. Up to 80% of cases are asymptomatic, and diagnosis in young and middle-aged adults is generally fortuitous. Symptoms, when they occur, are due to local compression of the affected nerve or adjacent structures. Schwannomas are benign, encapsulated and well-delimited 98% of the time, but cases of very aggressive, locally invasive, malignant schwannomas that tend to relapse and metastasize have been described.3 CT is useful for planning the surgical approach and a definitive diagnosis can be reached using immunohistochemical techniques.4 Surgical resection via thoracotomy or video-assisted thoracoscopy is the treatment of choice in these neurogenic tumors, and can be considered curative, in view of the low relapse rate.
Conflict of InterestsThe authors state that they have no conflict of interests. All the authors have read and approved the final manuscript.
Please cite this article as: Rodríguez CM, Naranjo S, Carbajo M. Schwannoma intratorácico del nervio vago. Arch Bronconeumol. 2015;51:255–256.