Light-chain deposition disease (LCDD) is a rare systemic disorder characterized by the accumulation of immunoglobulin light chains in multiple organs, and is associated, in most cases, with multiple myeloma or lymphoproliferative disorders. Unlike amyloidosis, the non-fibrillar deposits are negative on Congo Red staining.1 The organs most often affected are the kidney, the heart, the liver, and the nervous system. LCDD lung involvement is very uncommon. Presentation is generally in the form of converging pulmonary cysts, although some atypical forms occurs, such as nodules or bronchiectasis.2
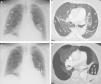
We report a case of pulmonary intracystic hemorrhage caused by anticoagulation in a 59-year-old woman, non-smoker, with severe pulmonary cystic involvement related with LCDD. The patient consulted due to progressive dyspnea and chest pain. In addition to her LCDD-related pulmonary cystic disease (she is on the waiting list for a lung transplant), her personal history included a diagnosis 8 years previously of multiple myeloma, and a nephrotic syndrome resistant to steroid treatment related with her LCDD. Chest radiograph (Fig. 1A) showed multiple cystic images in both lungs, predominantly in the subpleural regions (already known). Computed tomography (CT) angiogram of the chest detected pulmonary thromboembolism (PTE), and large subpleural thin-walled cystic lesions in all lobes (described in previous studies), traversed by pulmonary vessels (Fig. 1B). Four weeks after beginning anticoagulation, the patient had an episode of left chest pain and bloody sputum. A chest radiograph revealed an air-fluid level in the left lung base (Fig. 1C). The presence of air-fluid level in the interior of a cystic lesion of the left lower lobe was confirmed on chest CT (Fig. 1D). The high density of the intracavitary fluid component suggested recent bleeding. The pulmonary artery branches that surrounded the bleeding cystic formation was then embolized with gelfoam particles, and the patient's symptoms improved.
(A) Chest radiograph, showing multiple subpleural cystic formations (asterisks) in both lungs. (B) Axial image of chest CT (lung window), showing multiple converging cystic lesions in the periphery of both lungs. Note the presence of small pulmonary vessels (arrows) traversing the cystic formations. (C) Chest radiograph identifying an air-fluid level (arrows) in a cystic lesion in the left lung base (asterisk). (D) Minimum intensity projection (miniIP) axial reconstruction, showing the air-fluid level (arrows) corresponding to bleeding in the interior of a cystic lesion (asterisk) in the left lower lobe.
LCDD is a rare systemic disease, generally associated with plasma cell dyscrasias or lymphoproliferative syndrome, in which light chains of immunoglobulins are deposited in multiple tissues (particularly the kidney, liver and heart).1 When the lung is involved, diffuse cystic disease, nodules or bronchiectasis may develop.2,3 The pulmonary cystic form is the most common type of involvement, featuring diffusely distributed, thin-walled cysts of varying sizes (that tend to converge), with walls lined with pulmonary vessels, and, characteristically, pulmonary vessels traversing the cystic formations4,5 We found no references in the literature to intracystic hemorrhage as a complication of diffuse pulmonary cystic disorder related with LCDD. Nephrotic syndrome is a common occurrence in LCDD (resulting from renal involvement) and increases the risk of thromboembolic disease in these patients, but anticoagulation of thromboembolic events can increase the risk of intracavitary bleeding. In our opinion, it is important to remember in LCDD-related pulmonary cystic disorders that the vessels that characteristically penetrate the cysts are pulmonary vessels (rather than bronchial or other systemic arteries), so if intracystic hemorrhage does occur, embolization of the pulmonary arteries must be considered.
Please cite this article as: Sarasúa LG, Pacios-Blanco R-E, Arrieta P, Chinea-Rodríguez A. Hemorragia intraquística en paciente con afectación pulmonar quística secundaria a enfermedad por depósito de cadenas ligeras. Arch Bronconeumol. 2017;53:285–287.