IgG4-related disease is a fibroinflammatory disease in which the organs involved share similar pathological findings. Chest disease has been recently clinically and radiologically characterized. Most reports advocate prompt immunosuppressive therapy and describe a fast and good response. We report 3 cases of untreated IgG4-related lung disease that on follow-up have been clinically asymptomatic and radiologically stable or improved. In some cases of IgG4-related lung disease immunosuppressive therapy may not be warranted.
La enfermedad relacionada con IgG4 es una condición fibroinflamatoria en la cual los distintos órganos afectados comparten similitudes patológicas. Recientemente se ha caracterizado clínica y radiológicamente esta enfermedad en órganos torácicos. La mayoría de los casos descritos abogan por un tratamiento precoz con terapia inmunosupresora y observan una respuesta rápida y favorable. Describimos 3 casos de enfermedad pulmonar relacionada con IgG4 que no recibieron tratamiento farmacológico y que tuvieron una respuesta clínica y radiológica favorable o estable durante el seguimiento. La terapia inmunosupresora puede no ser necesaria en algunos casos de enfermedad pulmonar relacionada con IgG4.
IgG4-related lung disease (IgG4-RLD) is part of a spectrum of inflammatory diseases that share similar pathological features and elevated serum IgG4.1 Pathological findings include dense lymphoplasmacytic infiltrates, storiform-type fibrosis and obliterative phlebitis.1
Chest involvement in IgG4-disease may involve the lung parenchyma, airways, mediastinum and pleura.2 Most reports advocate immunosuppressive therapy and describe a rapid and satisfactory response. Some patients have been reported with poor or partial response to therapy.3 We report 3 cases of untreated IgG4-RLD that on follow-up have been clinically asymptomatic and radiologically stable or improved.
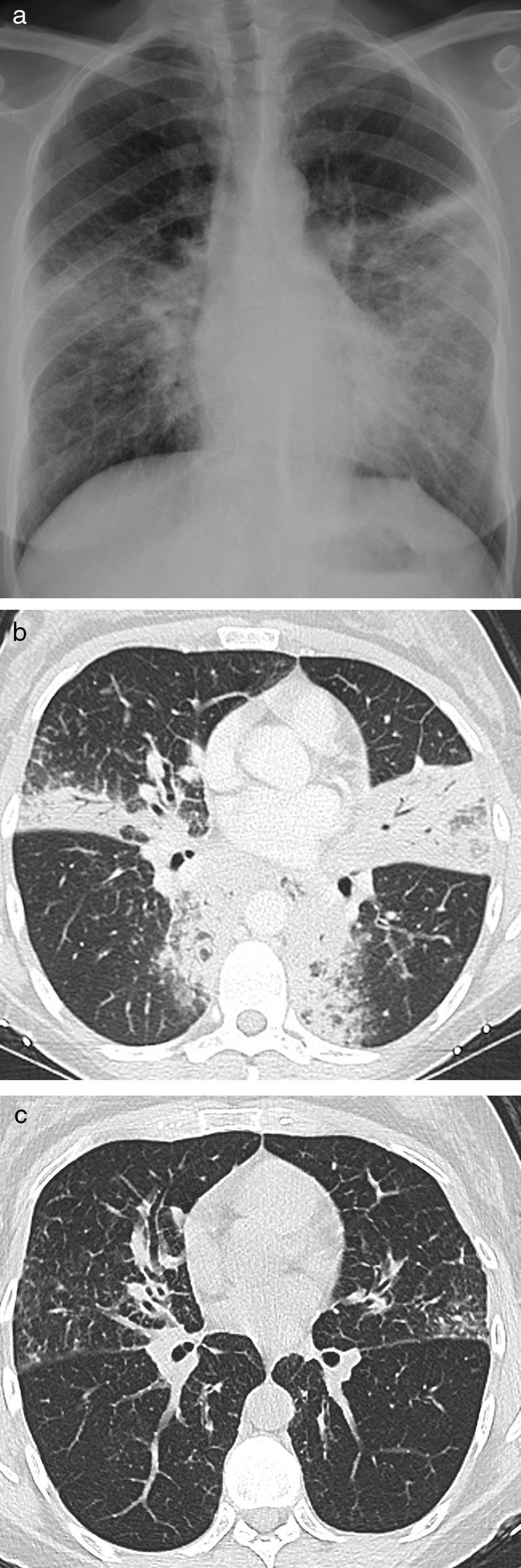
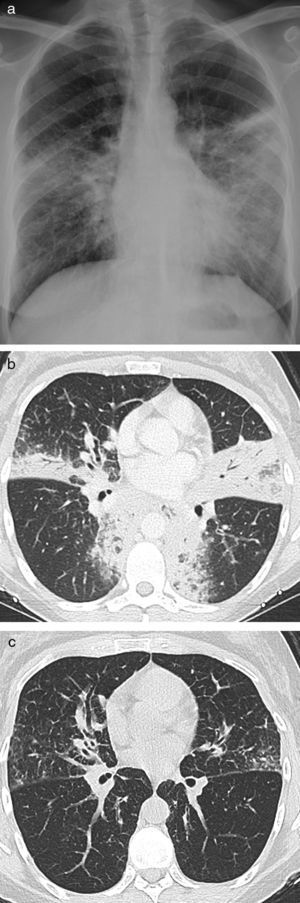
Case PresentationsCase 1A 44-year old female non-smoker presented with cough and dyspnea. She was afebrile, and physical examination was unremarkable. Her lab tests showed elevated CRP (122mg/L). Pulmonary function tests showed normal spirometry (FEV1 94%, FVC 96% predicted), normal lung volumes (TLC 102%, FRC 119% predicted) and reduced DLCO (68% predicted). Chest imaging showed bilateral air space disease and peribronchovascular nodules (Fig. 1a,b). Core needle biopsy showed thickened lung interstitium, dense lymphoplasmocytic infiltrate, fibrotic blood vessels and 30–40 IgG4+ plasma cells per high power field (hpf). Serum IgG4 was 573mg/dl (normal range: 3–201mg/dl). On follow-up (18 months from diagnosis), pulmonary symptoms resolved spontaneously and radiological findings had partially regressed (Fig. 1c). Spirometry, lung volumes and DLCO did not change. Several months after discharge, a diagnosis of dacryoadenitis was made following a complaint of dry eyes.
Case 2A 21-year old male, non-smoker, presented with productive cough and pleuritic chest pain. The physical examination was unremarkable, and lab tests showed mild leukocytosis (12570/μL). Spirometry showed moderate reversible airway obstruction (FEV1 68%, FVC 81% predicted; FEV1 post bronchodilator 85%). Lung volumes and DLCO were not available. Chest CT showed a 3cm spiculated mass in the right upper lobe. Fine needle aspiration suggested an inflammatory pseudotumor, therefore lobectomy was performed. Pathology showed a fibrotic mass with lymphoplasmacytic infiltration without obliterative phlebitis, and up to 40 IgG4+ plasma cells/hpf. Serum IgG4 was 416mg/dl. On follow-up (11 months from diagnosis) the patient was asymptomatic, and with no significant changes in spirometry. Chest CT 1 year after lobectomy did not show any new lesions.
Case 3A 58-year old male, non-smoker, presented with pleural thickening (incidental finding on chest CT). PET–CT showed retroperitoneal fibrosis, mesenteric panniculitis and aortitis. FEV1 was 85% and FVC 82% predicted. Lung volumes showed TLC 79% and FRC 84% predicted. DLCO was 75% predicted. Core needle biopsy showed densely fibrotic paucicellular pleura and a small fragment of adjacent lung parenchyma with lymphoplasmacytic infiltrate. No IgG4+ cells were identified. No asbestos bodies or silica particles were identified. Serum IgG4 was 177mg/dl. Two years after diagnosis the patient remained asymptomatic and chest CT did not show any changes.
DiscussionWe present 3 cases of IgG4-RLD that did not receive immunosuppressive therapy, followed for 11–24 months from diagnosis. Two cases (1 and 2) had respiratory symptoms at presentation that subsequently resolved. One (case 1) showed spontaneous radiological improvement while the other two cases were radiologically stable. To the best of our knowledge these are the first reported cases of IgG4-RLD with regression or stable disease without treatment.
Sarcoidosis is an important differential diagnosis. Both diseases are systemic in nature and the clinical presentation varies according to the organ(s) involved. The histological presence of epithelioid cell granulomas rules out the diagnosis of IgG4-RLD.1 None of our patients had this histological feature on pathology studies.
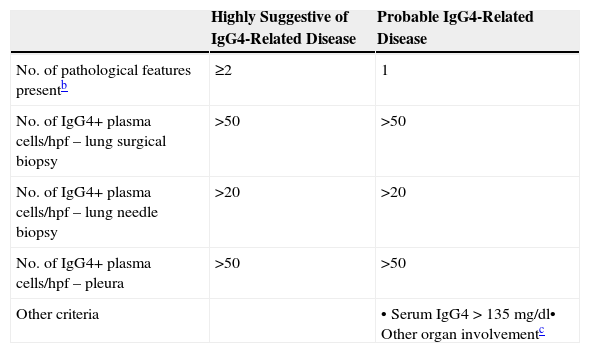
Our first case can be classified as highly suggestive of disease (Table 1).1 It showed the most striking clinical and radiological improvement. The third case, classifiable as probable disease,1 is also remarkable due to its extent and mostly fibrotic changes.
Diagnostic Criteria for IgG4-Related Lung Disease.a
| Highly Suggestive of IgG4-Related Disease | Probable IgG4-Related Disease | |
|---|---|---|
| No. of pathological features presentb | ≥2 | 1 |
| No. of IgG4+ plasma cells/hpf – lung surgical biopsy | >50 | >50 |
| No. of IgG4+ plasma cells/hpf – lung needle biopsy | >20 | >20 |
| No. of IgG4+ plasma cells/hpf – pleura | >50 | >50 |
| Other criteria | •Serum IgG4>135mg/dl•Other organ involvementc |
In contrast, three Chinese patients were reported as having severe disease with poor response to usual prednisone doses.3 A correlation between the large mass lesions and the severity of the disease was proposed. We did not see such a relationship, even though the radiological findings in our patients were of considerable extent. As discussed by Raj,4 no association has been made between disease severity and type or size of the pulmonary lesions.
HLA serotypes DRB1*0405 and DQB1*0401 have been associated with increased susceptibility and disease relapse in Far East populations with autoimmune pancreatitis. These serotypes are not prevalent in Middle-Eastern and European populations.5 We speculate that genetic differences might explain the different natural history of the disease.
In conclusion, we propose that each individual case should be carefully evaluated before a decision is made regarding the need for systemic immunosuppression. In some cases watchful waiting may be justified. Further genetic studies are warranted in order to clarify possible susceptibility to a more aggressive disease
Please cite this article as: Baltaxe E, Shulimzon T, Lieberman S, Rozenman J, Perelman M, Segel MJ. Enfermedad pulmonar relacionada con IgG4 – Tres casos no tratados con resultado benigno. Arch Bronconeumol. 2016;52:e1–e3.