To the Editor:
Idiopathic pulmonary haemosiderosis (IPH) is an extremely rare condition of unknown cause, which usually affects young children, and occasionally young adults, and is more common in males. This primary lung disease is mainly characterised by episodes of chronic or recurrent pulmonary haemorrhage and accumulation of haemosiderin in the lungs.1 To our knowledge there are few reports on post-mortem studies of this disease; therefore we believe that this case may be of great interest, particularly as it about a young adult patient (the majority of cases being reported in children), and because the clinical characteristics were rather unusual, with a fatal outcome.
This disease was described for the first time by Rudolf Virchow in 1864. The incidence is estimated to 1.23 cases per million inhabitants.2 The aetiology is still unknown, but it seems that immunological phenomena are involved; therefore treatment is mainly based on corticosteroids, but some studies doubt their effectiveness. Although its aetiology is unknown, it has been attributed to changes in the pulmonary microvasculature triggered by environmental factors.3,4 The clinical picture is characterised by episodes of haemoptysis, which can be more or less severe, accompanied by a cough, dyspnoea and pain in the sternum. Occasionally, the haemoptysis can be minimal and go unnoticed. Laboratory tests generally report a normocytic anaemia. The X-rays show irregular radio-opaque areas throughout the lungs. The diagnosis can be established from the clinical picture, the radiological characteristics, histopathological findings, and eliminating diseases that are clinically and radiologically similar.1 As diagnosis is established by exclusion of other diseases, it is essential to demonstrate the absence of a renal lesion, a deposit of immune complexes, anti-neutrophil cytoplasmic antibodies (ANCA) and anti-glomerular basement membrane antibodies (anti-GBM).
In 2003, an 18 year-old male was seen in the Emergency Department of the Mexico General Hospital with an uncontrollable haemoptysis. As history of relevance, 8 months before his death he suffered an anaemia syndrome, and during this period he had several episodes of associated haemoptysis. Two days before his admission to the Emergency Department he had a cough and an unquantified fever, being complicated with significant signs of haemoptysis. For this reason he was seen in the Emergency Department, where, despite the measures implemented and due to the massive haemoptysis, he had a hypovolemic shock and died. No imaging studies were performed as the patient died before these could be done. The immunofluorescence results were negative for IgC, IgM, C3 and C1 in the lungs and kidneys. The laboratory tests reported, red cells 4.02, Hb 8.5g/dl, Hct 28.2, MCV 70, MCH 21.5, MCHC 30.8, RDW 18.8%, platelets 381,000, MPV 9.7 fl, and white cells 22.1. Differential: lymphocytes 6.9%, eosinophils 0.6%, basophils 0.4%, lymphocytes 1,530, eosinophils 130, basophils 90, neutrophils 86, band cells 3, lymphocytes 8, and monocytes 3. The arterial blood gases were: pH 7.282, pCO2 22 mm Hg, pO2 92.4 mm Hg, HCO3 10.5 mmol/l.
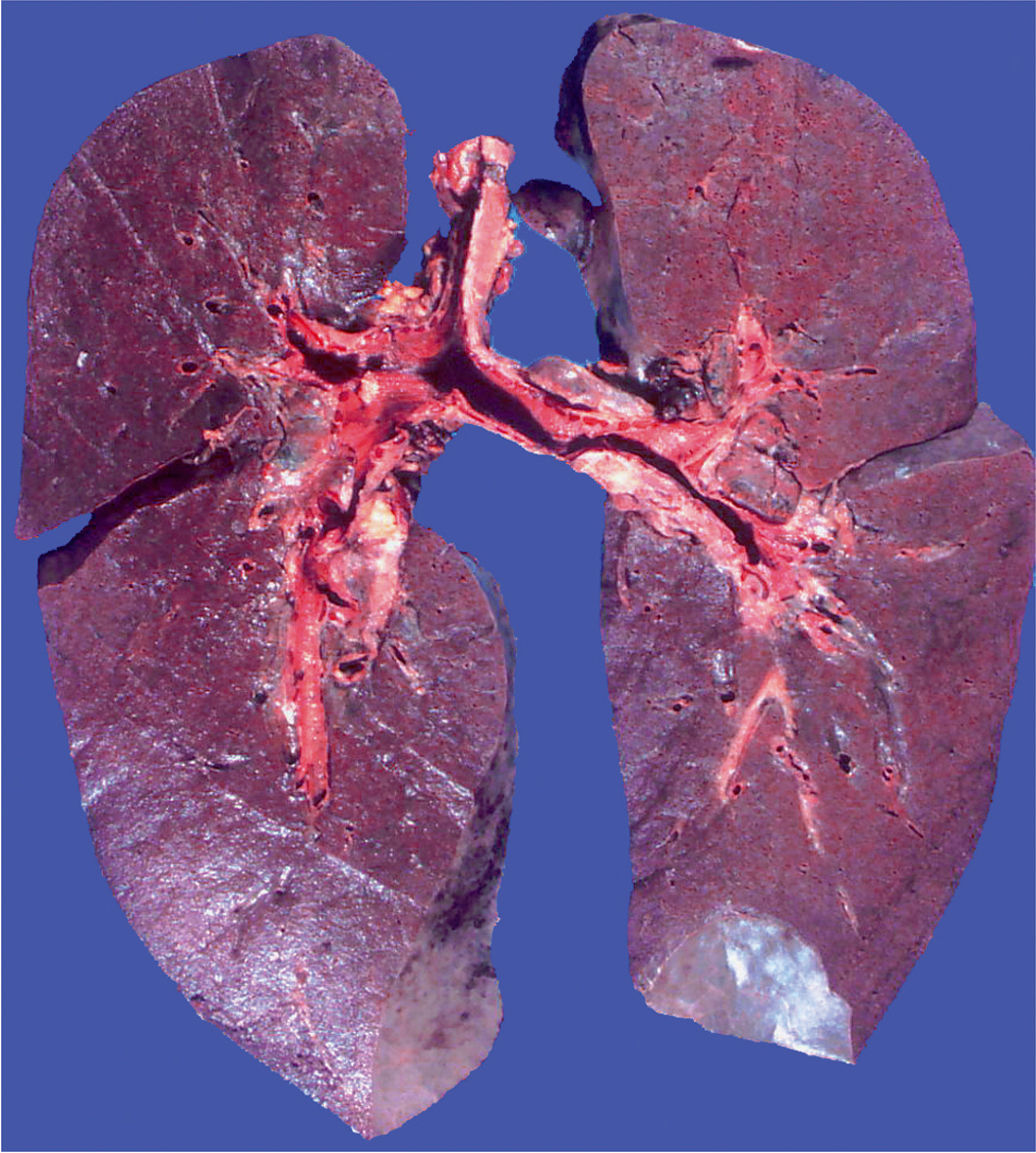
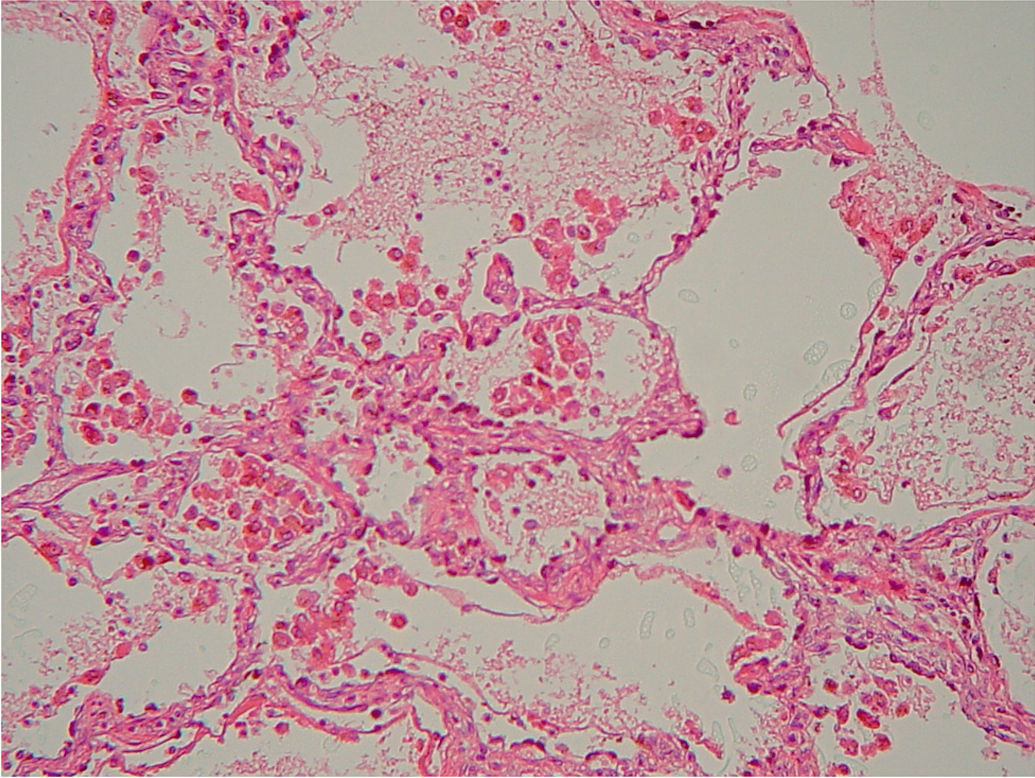
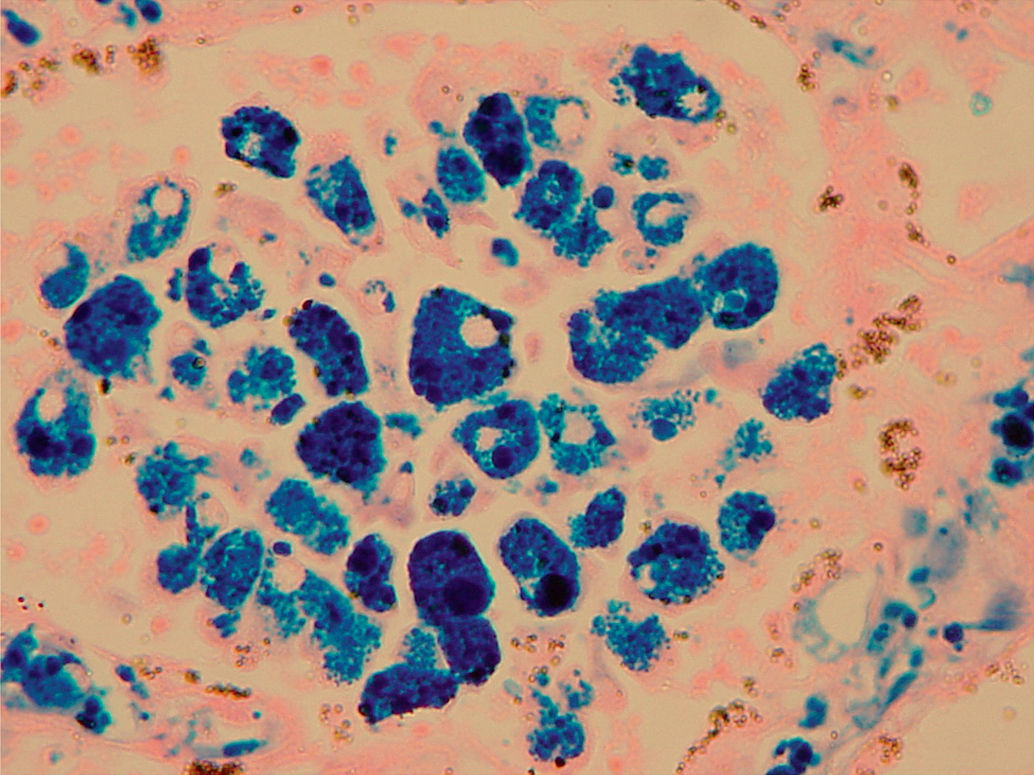
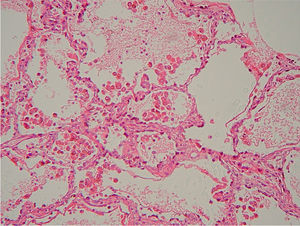
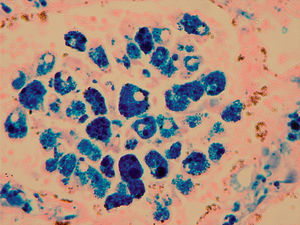
The post-mortem was performed on a young male, with generalised skin and conjunctival pallor; the lungs were increased in weight and the section showed an increase in consistency and a diffuse haemorrhagic appearance (Figure 1). The heart had no changes. The kidneys were of normal characteristics. In the microscopic study of the lungs a large quantity of erythrocytes and numerous macrophages were observed in the alveoli, with a dark coffee coloured material in their cytoplasm (haemosiderin granules, a product of haemoglobin breakdown of the red cells within the alveoli) (Figure 2). Iron was shown to be positive with Perl's stain in the previously described granules inside the macrophages (Figure 3). The alveolar walls were swollen to different degrees. A slight fibrosis was identified with Masson stain. The blood vessels did not have any apparent changes. The kidneys were of normal characteristics. The liver showed incipient centro-lobular necrosis. Immunofluorescence was performed on the kidney (with no signs of immune complex deposits), as well as carrying out immunohistochemical reactions for: IgC, IgM, C3 and C4 in the lungs, with no immunoreactivity demonstrated. With these studies, a possible Goodpasture syndrome, a well known cause of pulmonary bleeding, was ruled out. Therefore, by excluding this and other diseases, and in the absence of other associated histopathological data of relevance, the diagnosis was established as idiopathic pulmonary haemosiderosis. It was later found out that a sister of the deceased had the same symptoms of recurrent haemoptysis episodes. This post-mortem case is the second in this hospital within a period of 15 years. Although this condition is rare it is important to be familiar with it, since it is included among the diseases that present with pulmonary haemorrhage, mainly showing as a pulmonary haemosiderosis. The treatments with corticosteroids generally give good results, although other centres have used alternative drugs, such as, hydroxychloroquine, azathioprine and cyclophosphamide.1
Idiopathic pulmonary haemosiderosis demands a thorough clinical investigation. For this reason it is important to carry out peripheral blood tests, renal function and immunology tests and to assess cardiac function. Some authors have proposed performing lung biopsies and immunofluorescence, and electron microscopy. The immunofluorescence is generally negative and the electron microscopy shows non-specific data, such as endothelial cell oedema and irregular thickening of the alveolar basal membranes.6 The clinical course is unpredictable, since some cases that remain stable can suffer acute episodes of pulmonary haemorrhage 1. Pulmonary haemosiderosis may be primary or secondary; IPH is among those initially of lung origin, that associated with cow milk protein antibodies, known as Heiner syndrome, and have also been associated with some toxins produced by the stachybotrys fungus.1,4,5 There are other primary diseases with kidney-lung syndromes, such as Goodpasture and Wegener granulomatosis.4,5 Other causes of pulmonary origin are, foreign body aspiration and chronic infectious diseases. The causes of secondary pulmonary haemosiderosis include conditions such as pulmonary hypertension, vascular malformations, cardiac diseases, and haematological conditions, such as coagulation diseases, purpuras, etc.
This is a case with a fatal outcome and with very distinctive clinical characteristics, which we show although this disease is chronic it can have acute bleeding episodes, so intense that it could cause the death of the patient.