Radon has been a declared lung carcinogen since 1988.1 The seminal paper by Darby et al. showed a dose–response effect between indoor radon and lung cancer (LC) risk, where each 100Bq/m3 increase of radon concentration at home increased LC risk by 16%.2 This dose–response effect is present both in ever-smokers and in never smokers.3 Following Darby et al. study, the WHO recommended a target reference level of 100Bq/m3 with a threshold of 300Bq/m3.4 This recommendation was implemented by the European Union (EU) Directive published in 2014, establishing a maximum reference level of 300Bq/m3 for dwellings and workplaces, to be applied by member states before February 2018.5
In December 2022, Spain fully applied this EU directive to its national by-laws on ionizing radiation protection,6 and it shall be enforced as of June 2024, when all underground and ground floor workplaces located in designated radon-priority municipalities7 have to be measured. If radon concentration exceeds 300Bq/m3 these workplaces will have to be duly remediated. These workplaces include many belonging to the health sector, e.g. hospitals or primary care facilities.
To date, thousands of workers in Spain have been exposed to excessive radon concentrations in their workplace,8 but the impact of such exposure on the excess mortality of LC is unknown. The International Commission of Radiological Protection (ICRP) considers that 300Bq/m3 of radon concentration at home leads to an annual effective dose of 14mSv, whereas the same concentration at work leads to an annual effective dose of 4mSv.9
Complying with the current regulation is the starting point for health surveillance of radon exposed workers. If workers reach 6mSv or more annually, they have to be classified as exposed workers and employers are obliged to perform active dose surveillance.6
Apart from LC, there is no other disease causally linked to radon.10 The existing health surveillance protocol for ionizing radiation has a broad scope covering an extensive number of organs, and its section on the respiratory tract is insufficient for LC prevention or early diagnosis.11 According to the Spanish regulation,6 medical surveillance should be applicable to radon exposed workers when indicated by a health professional. Nevertheless, there is no specific surveillance protocol applicable to radon exposed workers. Therefore, the questions are: what kind of medical surveillance should be performed and what should be the eligibility criteria for it?
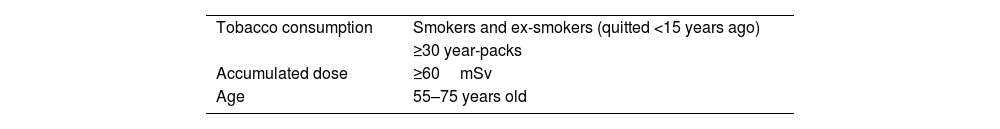
Currently, there is no specific protocol for the health surveillance of workers exposed to radon in any European country.12 In France, a pilot study is evaluating the applicability of an occupational LC screening with low dose computed tomography (LDCT) in which radon exposed workers are eligible.13 Should we use lung cancer screening with LDCT? Should we add more ionizing radiation to an individual already exposed to a high amount of such radiation at work? LDCT might be considered only in those cases where the risk–benefit balance is both reasonable and acceptable. We cannot forget that currently proposed screening recommendations only refer to ever-smokers and that there is no evidence on the use of such screening on radon-exposed individuals. Alternatively, the use of a chest X-ray might be a good alternative in these cases. This surveillance should also include an assessment of LC symptoms and tobacco cessation counseling in the case of current smokers. Table 1 proposes some eligibility criteria for medical surveillance.
Some Eligibility Criteria for Medical Surveillance Among Radon Exposed Workers.
| Tobacco consumption | Smokers and ex-smokers (quitted <15 years ago) |
| ≥30 year-packs | |
| Accumulated dose | ≥60mSv |
| Age | 55–75 years old |
Lung cancer is a multifactorial disease, with smoking as the main risk factor. Tobacco exposure and indoor radon present a sub multiplicative interaction for LC risk, and most LC cases due to radon exposure occur in ever-smokers.14 Therefore, at a given radon exposure in the workplace, LC risk may be different depending on the smoking history of the worker. Thus, smoking habit is key to determine LC risk, and should be a key element of the eligibility criteria (see Table 1).
Regarding radon exposure, we probably need to consider a minimum exposure time of 10 years, as proposed by the French National Authority for Health (HAS).15 This means that the inclusion would start at 60mSv (6mSv/year in 10 years) (see Table 1). Finally, eligibility criteria must consider age. We propose inclusion of those between 55 and 75 years old as usual in LC screening, as in Spain most LC cases are diagnosed within that age frame.
Furthermore, additional LC risk factors should be considered, namely radon exposure at home, other occupational exposures to carcinogenic agents, and pulmonary conditions such as COPD. Of note, multiple occupational exposures to carcinogens are possibly present in certain occupations, e.g. miners (exposed to silica dust or gamma radiation); metro workers (exposed to asbestos) or carpenters (exposed to wood dust, paint or varnishes).
Medical surveillance should start when the worker fulfills the inclusion criteria commented above and, for workers at the retirement age, it should last for at least five years providing evidence that radon exposure has been reduced after the first measurement. Annual health surveillance should be done during this period.
We consider essential to have a specific protocol in place for radon exposed workers. Such protocol should define the inclusion criteria, medical imaging tests along with a checklist of symptoms and signs of lung cancer and define a periodicity and length of surveillance. Some of these points might be applied using shared decision making with the worker and pneumologists have a role here. This protocol should consider and quantify the risk derived from smoking, exposure to radon at work and at home, exposures to other occupational carcinogens, age, the presence of a COPD diagnosis and, finally, it should consider the potential risks from any imaging test entailing exposure to ionizing radiation. To our knowledge, such protocol would be the first to be applied in the EU to radon exposed workers.12
FundingThis editorial has no external funding.
Conflict of InterestsThe authors do not have any conflict of interest related to the content of this manuscript.