Laryngeal tuberculosis (TB) is the most common manifestation of ear–nose–throat tuberculosis1 and the most common granulomatous disease of the larynx.2 However, it is an uncommon site of TB, and represents about 1% of all cases of extra pulmonary TB.2,3
In the beginning of the last century, about half of all patients with advanced pulmonary TB presented concomitant laryngeal TB due to direct spread of the infection from the lung.4
Currently, due to earlier and more appropriate treatment of pulmonary TB, the incidence of laryngeal TB has steadily decreased in developed countries. However, it still is on the rise in developing countries, in association with the Acquired Immune Deficiency Syndrome (AIDS) epidemic, low socioeconomic conditions and lack of adequate TB chemotherapy, among other factors.5–7
We report the case of a 57-year-old man, smoker of 30 pack-years, presenting with a two-year history of hoarseness, weight loss of 20kg, with no anorexia. He had no dysphagia, odynophagia, cough, fever or night sweats. The patient worked as a carpenter, and had had a history of heavy alcohol consumption until ten years previously. He reported a history of recurrent otitis and had undergone bilateral ear surgery about 10 years previously. He had facial palsy of unknown cause since he was13 years old, and had no personal history of TB or contact with patients with TB. Physical examination, apart from left hemifacial palsy, was unremarkable.
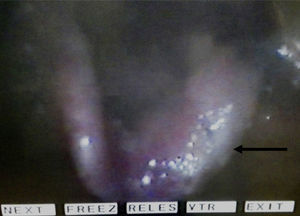
The patient was evaluated by the otorhinolaryngologist and underwent laryngoscopy (Fig. 1) that revealed mucosal thickening, irregularities and leukoplasia lesions of the left side of the epiglottis and of the left vestibular fold. Vocal cords were normal. Laryngeal CT showed no lymphadenopathies or other abnormalities.
The patient then underwent a suspension microlaryngoscopy during which the epiglottic lesion was biopsied and sent for histological and mycobacterial direct stain and culture study. Anatomopathological study showed no signs of malignancy or granulomas. Mycobacterial cultural exam was positive for Mycobacterium Tuberculosis Complex, susceptible to all first line anti-TB drugs.
The patient was then referred to the tuberculosis outpatient clinic. Occupational health services were immediately activated in order to initiate screening of exposed health professionals. HIV infection was excluded and a chest X-ray (CXR) was performed, showing a cavitary lesion at the left lung apex and an infiltrate on the left lower lobe. Sputum samples were collected and anti-TB medication with isoniazid, rifampin, pirazinamid and ethambutol was started. Mycobacterium direct test of sputum was negative and culture was positive for Mycobacterium tuberculosis complex.
The patient's symptoms improved and videolaringoscopy performed after 6 months of treatment showed resolution of the epiglotic lesions.
In the last three decades, a change in the pathophysiology of laryngeal TB has been observed. Although concomitant pulmonary involvement is common, more cases of primary laryngeal TB, without pulmonary involvement, have been described.6,8–11
Clinical presentation has also changed. Ling et al.8 compared a group of patients diagnosed with laryngeal tuberculosis before 1990 and another after 1998 and found that odynophagia was the most frequent symptom among the former group and hoarseness among the latter. Moreover, in the group of patients from before 1990, constitutional symptoms were more frequently reported.
We believe that, in our case, epiglottic TB originated from dissemination of lung infection. This was subsequently demonstrated by the presence of cavitary lung disease and positive mycobacterial culture of the sputum. However, the patient had no pulmonary symptoms suggestive of TB, so lung infection was not suspected. As illustrated by the present case, despite advanced pulmonary involvement, chest symptoms might not be prominent.5,12 Nevertheless, direct spread of bacilli from the lung is still the most common mechanism of laryngeal tuberculosis, especially in countries where TB burden is still a considerable burden. Portugal has only recently reached the cut-off of low incidence, with 20 new cases of tuberculosis per 100000 inhabitants in 2015. A few Portuguese districts still report an intermediate TB incidence rate.13
Hoarseness and weight loss are also features of laryngeal carcinoma. Symptoms of laryngeal TB are unspecific and differentiation from cancer is difficult, as the two diagnoses may even coexist.10
A shift to older ages and male predominance has also been observed. In earlier series, patients were 20–40 years old, but more recent studies report an age range of 17–71 years old, predominantly male.6,8 Our case is consistent with this trend, and also includes the risk factors most usually associated with laryngeal TB: tobacco and alcohol consumption.8,12
Some changes in the macroscopic appearance of laryngeal TB have also been described. TB lesions have so far been mostly ulcerated and located in the posterior part of the larynx. Nowadays, the majority of cases show no ulceration and no predilection is observed for any part of the larynx.8 The case described manifested with mucosal thickening and irregularities of the left side of the epiglottis and of the left vestibular fold. Hypertrophic or exophytic lesions are the most common findings nowadays, which makes the differential diagnosis with malignancy even more complicated.2,6,8
Misdiagnosis of laryngeal TB poses a serious risk for the community, as it is highly contagious. That is why otorhinolaryngologists, pulmonologists and the medical community in general must be aware of the symptoms and remember to investigate the possibility of TB. An important consideration is screening, not only of the patient's contacts but also of health care professionals, as some invasive airway procedures were performed, with an important risk of infection.
When the hypothesis of laryngeal TB is considered, a CXR is compulsory. If there are pulmonary lesions suggestive of TB, it is more likely that the laryngeal lesions have the same etiology, even though biopsy is still required to establish the diagnosis.
Please cite this article as: Dias A, Monteiro F, Silva J, Duarte R. Caso clínico de ronquera de dos años de duración: ¿comenzó en el pulmón?. Arch Bronconeumol. 2017;53:457–458.