Obesity has emerged as a significant independent predictor of severity in pandemic influenza A (H1N1)pdm09. The aim of this study was to investigate the association between body mass index (BMI) and the risk of hospitalization due to influenza.
MethodsHospitalized patients (n=755) with laboratory-confirmed influenza were individually matched by age, admission/visit date, and province with an outpatient (n=783) with laboratory-confirmed influenza and an outpatient control (n=950). We compared the BMI using conditional logistic regression adjusted for potential confounding factors (aOR). The population attributable fraction (PAF) was calculated.
ResultsA higher BMI was associated with an increased risk of hospitalization compared to both outpatient cases (aOR=1.11; 95% CI: 1.07–1.16) and outpatient controls (aOR=1.04; 95% CI: 1.01–1.07). Compared with normal weight, obesity type I, obesity type II and obesity type III was associated with a greater likelihood of hospitalization compared with outpatient cases (aOR=1.85, 95% CI: 1.05–3.26; aOR=5.24, 95% CI: 1.94–14.15 and aOR=44.38, 95% CI: 4.47–440.5). Compared with normal weight, obesity type II and obesity type III was associated with a greater likelihood of hospitalization compared with outpatient controls (aOR=4.37, 95% CI: 1.79–10.69 and aOR=4.95, 95% CI: 1.45–16.87). In persons without influenza vaccination, all categories of BMI≥30kg/m2 were associated with a greater likelihood of hospitalization compared with normal weight in both outpatient cases and outpatient controls. The PAF of hospitalization by influenza due to BMI ranged from 21.9% to 8.5%; in the case of unvaccinated against influenza between 20.5% and 16.9%.
ConclusionA high BMI is associated with an increased risk of hospitalization due to influenza. High percentage of hospital admissions are attributable to their BMI, especially in nonvaccinated.
Durante la pandemia de la gripe A (H1N1)pdm09 la obesidad emergió como un predictor signficativo de gravedad. El objetivo de este estudio fue investigar la asociación entre el índice de masa corporal (IMC) y el riesgo de hospitalización por gripe.
MétodosPacientes hospitalizados (n=755) con gripe confirmada por el laboratorio se emparejaron individualmente con pacientes ambulatorios (n=783) con gripe confirmada por el laboratorio y con controles ambulatorios (n=950) según edad, fecha de ingreso/visita y provincia. El IMC se comparó mediante una regresión logística condicional ajustada a los posibles factores de confusión (ORa). Fracción atribuible poblacional (FAP).
ResultadosLos valores elevados de IMC se asociaron a mayor riesgo de hospitalización, en comparación con los casos ambulatorios (ORa=1,11; IC 95%: 1,07–1,16) y con los controles ambulatorios (ORa=1,04; IC 95%: 1,01-1,07). En comparación con el peso normal, la obesidad tipo I, la obesidad tipo II y la obesidad tipo III se asociaron a mayor probabilidad de hospitalización, en comparación con los casos ambulatorios (ORa=1,85; IC 95%: 1,05-3,26; ORa=5,24; IC 95%: 1,94-14,15 y ORa=44,38; IC 95%: 4,47-440,5). En comparación con el peso normal, la obesidad tipo II y la obesidad tipo III se asociaron a mayor probabilidad de hospitalización, en comparación con los controles ambulatorios (ORa=4,37; IC 95%: 1,79-10,69 y ORa=4,95; IC 95%: 1,45-16,87). En los sujetos no vacunados de la gripe todas las categorías de IMC≥30kg/m2 se asociaron a mayor probabilidad de hospitalización, en comparación con el peso normal, tanto en los casos ambulatorios como en los controles ambulatorios. La FAP de hospitalización por gripe atribuible al IMC se situó entre el 21,9 y el 8,5%, y en los sujetos no vacunados de la gripe, entre el 20,5 y el 16,9%.
ConclusiónUn IMC elevado se asocia a mayor riesgo de hospitalización por gripe. Un alto porcentaje de los ingresos hospitalarios son atribuibles al IMC, especialmente en los sujetos no vacunados.
Obesity is a rising health threat in a growing number of countries and is currently viewed as an emerging global epidemic.1 The World Health Organization (WHO) estimates that 600 million adults, 18 years and older, were obese in 2014, and that worldwide obesity has more than doubled since 1980.2
In Spain, the prevalence of obesity has continued to grow in recent decades and today 1 in 4 people aged >18 years is obese.3 Obesity is associated with metabolic and cardiovascular problems and has a negative impact on the immune response and on susceptibility to infectious diseases.4 In the influenza A (H1N1)pdm09 pandemic, obesity emerged as a significant independent risk factor for hospitalization and death.5 Until then, the relationship between obesity and influenza had been established on the basis of obesity-related diseases that were recognized risk factors for influenza severity, such as diabetes, cardiovascular disease and others.
The WHO estimates that between 3 and 5 million cases of severe influenza and 250000 to 500000 influenza deaths occur annually.6
The combination of the two epidemics requires special attention due to their obvious impact on the health of the entire population.
In the United States, the Advisory Committee on Immunization Practices added “morbid obesity” to the list of conditions that increase the risk of influenza-related complications and for which prompt empiric influenza antiviral treatment is recommended during influenza seasons.7 They also recommended conducting further studies to determine whether obesity was a specific risk factor for the 2009–2010 pandemic only, or whether it also affects other seasonal influenza epidemics.8
The aim of this study was to investigate the association between body mass index (BMI) and the risk of hospitalization due to influenza in both the 2009–2010 and 2010–2011 influenza seasons.
Materials and MethodsStudy Population and DesignThis study forms part of the “Risk factors of hospitalization due to influenza A (H1N1) 2009 and effectiveness of pharmacological and non-pharmacological interventions in its prevention. Case–control study project”, led by the Centres for Biomedical Research in Epidemiology and Public Health (CIBERESP) and Respiratory Diseases (CIBERES).9 The study was conducted in 29 hospitals in 7 Spanish regions (Andalusia, the Basque Country, Castile and Leon, Catalonia, Madrid, Navarre and Valencia Community).
Cases and controls were recruited between July 2009 and April 2011. We selected cases among patients hospitalized for >24h with influenza-like illness, acute respiratory infection, septic shock or multiple organ failure in whom influenza virus A (H1N1) 2009 infection was confirmed by real-time reverse-transcription polymerase chain reaction (RT-PCR).10 Participating hospitals had protocols for systematic swabbing of patients admitted with influenza-like illness, defined as the sudden onset of any general symptom (fever or febrile symptoms, headache, myalgia), in addition to any respiratory symptom (cough, sore throat, shortness of breath).11 We excluded patients with nosocomial infection, defined as influenza appearing 48h or more after admission for another cause.
For each hospital case, we selected two matched controls: one patient consulting for influenza confirmed by RT-PCR (outpatient case) and another patient consulting for any reason other than influenza-like illness or acute respiratory infection (outpatient control).
Both outpatient cases and outpatient controls were recruited in primary care centers of the same geographical area as the hospitalized cases, from among the population of patients attending the primary care center for reasons other than acute respiratory infection or influenza-like illness. No cases were recruited from hospital-based emergency departments.
Controls were matched with each case according to age (±5 years), date of hospitalization (±10 days) and province of residence. Occasionally, more than one patient who met the criteria for pairing with the same case was recruited.
Patients were recruited prospectively and retrospectively. If no admissions were made in a hospital center after the beginning of the study, cases and controls were recruited retrospectively with the same criteria as for prospectively recruited patients.
Patients who did not give written consent were excluded and for this paper, we excluded patients <18 years old, BMI<18.5kg/m2, and pregnancy.
The study was approved by the Ethics Committee of the hospitals involved. Written informed consent was obtained from all patients included in this study.
Data CollectionSpecifically trained health professionals used a structured questionnaire to collect information on cases and controls by interview and review of clinical charts. This information included sociodemographic variables, current smoking habit, alcohol abuse (defined as consumption was greater than 4 standard units a day for women and 6 for men), pregnancy, major chronic conditions, unplanned hospitalization in the previous 12 months, confinement to bed in the 7 days before the hospitalization or visit, and other pre-existing risk factors for complicated influenza. The following major clinical conditions were recorded: chronic respiratory disease, asthma, cardiovascular disease, chronic renal disease, diabetes mellitus, immunodeficiency, neurological disease and disability, and cancer. Other risk factors for influenza complications previous to hospitalization or the medical visit were collected: chronic respiratory failure, chronic heart failure, pneumonia in the previous 2 years, systemic corticoids, and inhaled corticoid treatments. Information on the monovalent influenza A (H1N1)pdm09, 2010–2011 seasonal influenza and pneumococcal vaccination status was obtained from medical records or vaccination cards. Cases were considered vaccinated with the seasonal or pandemic influenza vaccines if they had received a dose of the vaccine at least 14 days before symptom onset. Controls were considered vaccinated if they had received the dose at least 14 days before symptom onset in the matched case.
BMI was obtained from direct or telephonic interview with the patients by healthcare workers. BMI was used as a continuous and categorical variable (normal weight: BMI 18.5–24.9kg/m2; overweight: 25.0–29.9kg/m2; obesity grade I: 30–34.9kg/m2; obesity grade II: 35–39.9kg/m2, and obesity grade III: BMI≥40kg/m2).1,12
Statistical AnalysisHospital cases were compared with outpatient cases and outpatient controls to estimate the risk of influenza-associated hospitalization. A bivariate comparison of demographic variables, medical conditions and BMI was made between cases and controls using the χ2 test for categorical variables and the Student's t test for continuous variables. The odds ratios (OR) for BMI, with 95% confidence intervals (CI), were calculated using conditional logistic regression models adjusted for potential confounders. The comparison was adjusted by sex, age (≥65 vs <65 years), ethnicity (Caucasian vs non-Caucasian), studies (primary education or less vs education level higher than primary), alcohol abuse (yes or no), smoking status (current vs not current smoker), history of pneumonia in the two previous years (yes or no), influenza vaccination, and risk factors (yes or no). One or more of the following problems were considered risk factors: lung diseases, cardiovascular diseases, kidney diseases, immunosuppressive diseases, neurological diseases, diabetes, immunosuppressive treatment or acetylsalicylic acid treatment.
We performed restriction analysis for the following subgroups: age (<65 years), influenza vaccination (unvaccinated subjects) and season (2009–2010 and 2010–2011). The odds ratios (OR) for BMI (continuous and categorical), with their 95% confidence intervals (CI), were calculated using conditional logistic regression, aOR were calculated using conditional logistic regression models adjusted for those all variables (Table 1).
Characteristics of Hospitalized Cases, Outpatient Cases and Outpatient Controls.
| Variable | Hospitalized Cases | Outpatient Cases | Outpatient Controls | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | n | % | N | n | % | N | n | % | |
| Male | 755 | 454 | 60.1 | 783 | 384 | 49.0 | 950 | 410 | 43.2 |
| 65 years or older | 755 | 166 | 22.0 | 783 | 62 | 7.9 | 950 | 175 | 18.4 |
| Caucasian | 747 | 682 | 91.3 | 779 | 738 | 94.7 | 945 | 898 | 95.0 |
| Primary education or less | 734 | 300 | 40.9 | 782 | 155 | 19.8 | 947 | 296 | 31.3 |
| Current smokers | 749 | 228 | 30.4 | 779 | 209 | 26.8 | 947 | 220 | 23.2 |
| Alcoholism | 741 | 95 | 12.8 | 782 | 36 | 4.6 | 948 | 46 | 4.9 |
| History of pneumonia | 755 | 80 | 10.6 | 783 | 44 | 5.6 | 950 | 27 | 2.8 |
| Risk factors | 755 | 522 | 69.1 | 783 | 219 | 28.0 | 950 | 301 | 31.7 |
| Vaccinated against influenza | 730 | 84 | 11.5 | 733 | 46 | 6.3 | 890 | 145 | 16.3 |
| Postpandemic season | 755 | 400 | 53.0 | 783 | 409 | 52.2 | 950 | 509 | 53.6 |
| BMI | |||||||||
| 18.5–24.9 | 755 | 280 | 37.1 | 783 | 405 | 51.7 | 950 | 423 | 44.5 |
| 25.0–29.9 | 755 | 266 | 35.2 | 783 | 266 | 34.0 | 950 | 358 | 37.7 |
| 30.0–34.9 | 755 | 120 | 15.9 | 783 | 94 | 12.0 | 950 | 126 | 13.3 |
| 35.0–39.9 | 755 | 54 | 7.2 | 783 | 14 | 1.8 | 950 | 34 | 3.6 |
| ≥40 | 755 | 35 | 4.6 | 783 | 4 | 0.5 | 950 | 9 | 0.9 |
| kg/m2; mean (SD) | 27.8 (6.4) | 25.4 (4.1) | 26.3 (4.8) | ||||||
N, total number of patients for whom this information is available; n, number of patients in this category.
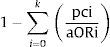
The population attributable fraction (PAF) was calculated using the formula:
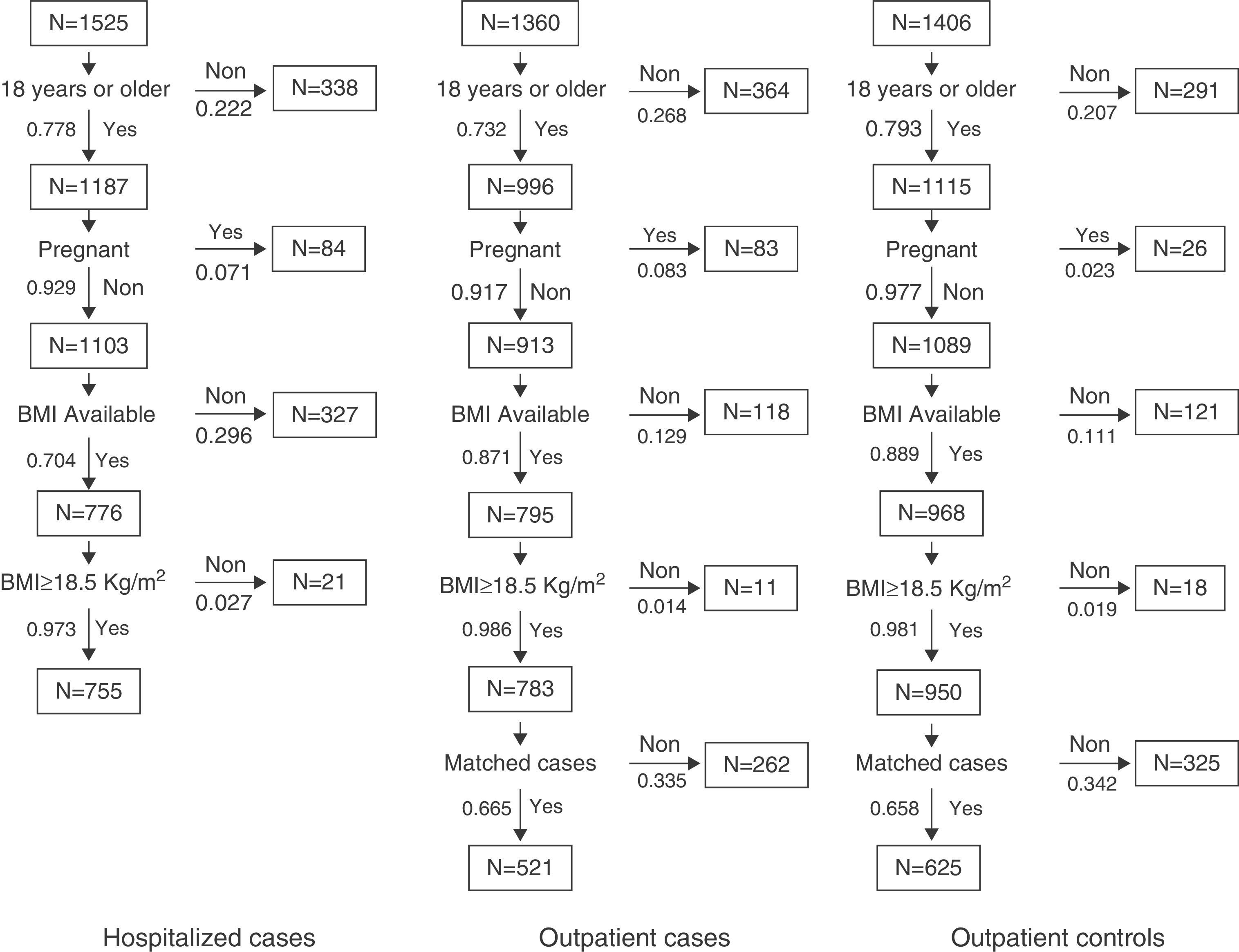
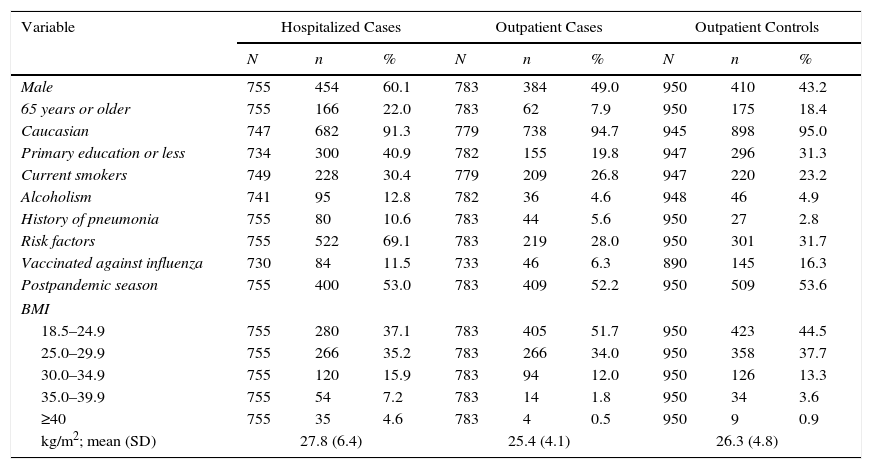
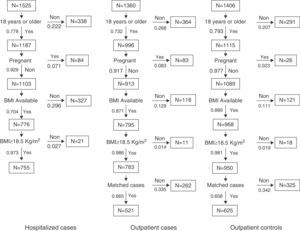
where pci is the proportion of patients in the exposure level and aORi is the odds ratio adjusted in the level of exposure.13RESULTSCharacteristics of Cases and ControlsFig. 1 shows the selection algorithm for cases and controls for this study, selected from the population which participated in the “Risk factors of hospitalization due to influenza A (H1N1) 2009 and effectiveness of pharmacological and non-pharmacological interventions in its prevention. Case–control study project”. According to the selection criteria of this study, 27.6% of hospitalized cases, 32.8% of outpatient cases, and 22.5% of outpatient controls were excluded. No information on height and weight was available for 29.6% of the hospitalized cases, 12.9% of the outpatient cases, and 11.1% of the outpatient controls. A total of 755 hospitalized patients, 783 outpatient cases, and 950 outpatient controls met the selection criteria and provided height and weight data. Finally, conditional logistic regression analyses were performed on 521 hospitalized cases, and 521 paired outpatient cases, and on 625 hospitalized cases and 625 paired outpatient controls. Table 1 shows the distribution of the study variables among the study subjects. Hospitalized cases were mainly men (60.1%), 22% were 65 years of age or older, 40.9% had primary level education or less, 30.4% were current smokers, 12.5% at risk drinkers, 10.6% had a history of pneumonia in the previous 2 years, 69% had some risk factor or risk treatment for developing influenza, and 11.5% had been vaccinated against influenza. Outpatient cases were 49% men, 7.9% aged 65 years or older, 19.8% had primary level education or less, 26.8% were current smokers, 4.6% at risk drinkers, 5.6% had a history of pneumonia in the previous 2 years, 28% had some risk factor or risk treatment for developing influenza, and 6.3% had been vaccinated against influenza. Outpatient controls were 43% men, 18.4% aged 65 years or older, 31.3% had primary level education or less, 23.2% were current smokers, 4.9% at risk drinkers, 2.8% had a history of pneumonia in the previous 2 years, 31.7% had some risk factor or risk treatment for developing influenza, and 16.3% had been vaccinated against influenza.
The prevalence of obesity and BMI values averages were 27.7% and 27.8kg/m2; 14.3% and 25.4kg/m2, and 17.8% and 26.3kg/m2 in hospitalized cases, outpatients cases and outpatients controls, respectively.
The causes of hospital admission were: pneumonia, 192 cases (25.4%); acute respiratory distress syndrome, 115 cases (15.2%); sepsis, 72 cases (9.5%); and influenza, 376 cases (49.8%).
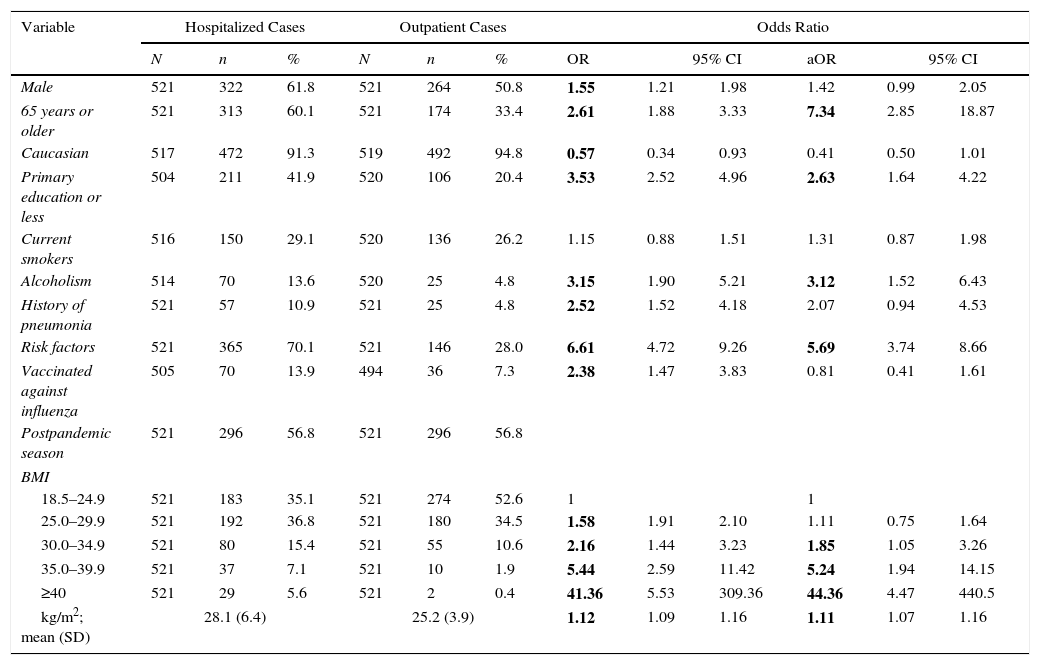
Risk of Hospitalization Due to InfluenzaHospital cases vs outpatient cases: There were significant differences in the BMI distribution between hospitalized and outpatient cases (28.1kg/m2 vs 25.2kg/m2; P<0.0001), with a higher prevalence of obesity in hospitalized cases (28.1% vs 12.9%; P<0.0001) (Table 2).
Effect of Study Variables on the Risk of Laboratory-Confirmed Influenza Hospitalization.
| Variable | Hospitalized Cases | Outpatient Cases | Odds Ratio | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | n | % | N | n | % | OR | 95% CI | aOR | 95% CI | |||
| Male | 521 | 322 | 61.8 | 521 | 264 | 50.8 | 1.55 | 1.21 | 1.98 | 1.42 | 0.99 | 2.05 |
| 65 years or older | 521 | 313 | 60.1 | 521 | 174 | 33.4 | 2.61 | 1.88 | 3.33 | 7.34 | 2.85 | 18.87 |
| Caucasian | 517 | 472 | 91.3 | 519 | 492 | 94.8 | 0.57 | 0.34 | 0.93 | 0.41 | 0.50 | 1.01 |
| Primary education or less | 504 | 211 | 41.9 | 520 | 106 | 20.4 | 3.53 | 2.52 | 4.96 | 2.63 | 1.64 | 4.22 |
| Current smokers | 516 | 150 | 29.1 | 520 | 136 | 26.2 | 1.15 | 0.88 | 1.51 | 1.31 | 0.87 | 1.98 |
| Alcoholism | 514 | 70 | 13.6 | 520 | 25 | 4.8 | 3.15 | 1.90 | 5.21 | 3.12 | 1.52 | 6.43 |
| History of pneumonia | 521 | 57 | 10.9 | 521 | 25 | 4.8 | 2.52 | 1.52 | 4.18 | 2.07 | 0.94 | 4.53 |
| Risk factors | 521 | 365 | 70.1 | 521 | 146 | 28.0 | 6.61 | 4.72 | 9.26 | 5.69 | 3.74 | 8.66 |
| Vaccinated against influenza | 505 | 70 | 13.9 | 494 | 36 | 7.3 | 2.38 | 1.47 | 3.83 | 0.81 | 0.41 | 1.61 |
| Postpandemic season | 521 | 296 | 56.8 | 521 | 296 | 56.8 | ||||||
| BMI | ||||||||||||
| 18.5–24.9 | 521 | 183 | 35.1 | 521 | 274 | 52.6 | 1 | 1 | ||||
| 25.0–29.9 | 521 | 192 | 36.8 | 521 | 180 | 34.5 | 1.58 | 1.91 | 2.10 | 1.11 | 0.75 | 1.64 |
| 30.0–34.9 | 521 | 80 | 15.4 | 521 | 55 | 10.6 | 2.16 | 1.44 | 3.23 | 1.85 | 1.05 | 3.26 |
| 35.0–39.9 | 521 | 37 | 7.1 | 521 | 10 | 1.9 | 5.44 | 2.59 | 11.42 | 5.24 | 1.94 | 14.15 |
| ≥40 | 521 | 29 | 5.6 | 521 | 2 | 0.4 | 41.36 | 5.53 | 309.36 | 44.36 | 4.47 | 440.5 |
| kg/m2; mean (SD) | 28.1 (6.4) | 25.2 (3.9) | 1.12 | 1.09 | 1.16 | 1.11 | 1.07 | 1.16 | ||||
BMI, body mass index; N, total number of patients for whom this information is available; n, number of patients in this category; OR, crude odds ratio; aOR, odds ratio adjusted for all variables included in the table.
The odds of hospitalization in patients diagnosed with influenza (comparison between hospitalized and outpatient cases) was significantly higher in patients with BMI 30–34.9kg/m2 (aOR=1.85), 35–39.9kg/m2 (aOR=5.24), and ≥40kg/m2 (aOR=44.36), compared with patients of normal weight (Table 2). In the case of BMI as a continuous variable, a greater risk of hospitalization was observed with a higher BMI (aOR=1.11; 95% CI=1.07–1.15) (Table 2).
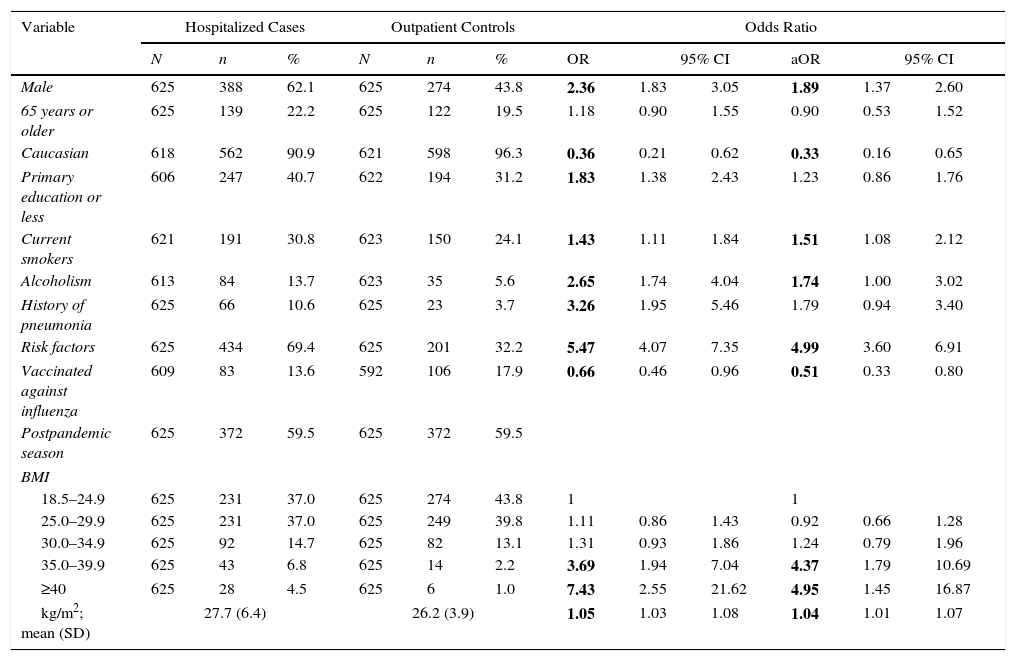
Hospitalized cases vs outpatient controls: There were significant differences in the BMI distribution between hospitalized cases and outpatient controls (27.7kg/m2 vs 26.2kg/m2; P<0.0001), with a higher prevalence of obesity in hospitalized cases (26.0% vs 16.3%; P<0.0001) (Table 3).
Effect of Study Variables on the Risk of Laboratory-Confirmed Influenza Hospitalization.
| Variable | Hospitalized Cases | Outpatient Controls | Odds Ratio | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | n | % | N | n | % | OR | 95% CI | aOR | 95% CI | |||
| Male | 625 | 388 | 62.1 | 625 | 274 | 43.8 | 2.36 | 1.83 | 3.05 | 1.89 | 1.37 | 2.60 |
| 65 years or older | 625 | 139 | 22.2 | 625 | 122 | 19.5 | 1.18 | 0.90 | 1.55 | 0.90 | 0.53 | 1.52 |
| Caucasian | 618 | 562 | 90.9 | 621 | 598 | 96.3 | 0.36 | 0.21 | 0.62 | 0.33 | 0.16 | 0.65 |
| Primary education or less | 606 | 247 | 40.7 | 622 | 194 | 31.2 | 1.83 | 1.38 | 2.43 | 1.23 | 0.86 | 1.76 |
| Current smokers | 621 | 191 | 30.8 | 623 | 150 | 24.1 | 1.43 | 1.11 | 1.84 | 1.51 | 1.08 | 2.12 |
| Alcoholism | 613 | 84 | 13.7 | 623 | 35 | 5.6 | 2.65 | 1.74 | 4.04 | 1.74 | 1.00 | 3.02 |
| History of pneumonia | 625 | 66 | 10.6 | 625 | 23 | 3.7 | 3.26 | 1.95 | 5.46 | 1.79 | 0.94 | 3.40 |
| Risk factors | 625 | 434 | 69.4 | 625 | 201 | 32.2 | 5.47 | 4.07 | 7.35 | 4.99 | 3.60 | 6.91 |
| Vaccinated against influenza | 609 | 83 | 13.6 | 592 | 106 | 17.9 | 0.66 | 0.46 | 0.96 | 0.51 | 0.33 | 0.80 |
| Postpandemic season | 625 | 372 | 59.5 | 625 | 372 | 59.5 | ||||||
| BMI | ||||||||||||
| 18.5–24.9 | 625 | 231 | 37.0 | 625 | 274 | 43.8 | 1 | 1 | ||||
| 25.0–29.9 | 625 | 231 | 37.0 | 625 | 249 | 39.8 | 1.11 | 0.86 | 1.43 | 0.92 | 0.66 | 1.28 |
| 30.0–34.9 | 625 | 92 | 14.7 | 625 | 82 | 13.1 | 1.31 | 0.93 | 1.86 | 1.24 | 0.79 | 1.96 |
| 35.0–39.9 | 625 | 43 | 6.8 | 625 | 14 | 2.2 | 3.69 | 1.94 | 7.04 | 4.37 | 1.79 | 10.69 |
| ≥40 | 625 | 28 | 4.5 | 625 | 6 | 1.0 | 7.43 | 2.55 | 21.62 | 4.95 | 1.45 | 16.87 |
| kg/m2; mean (SD) | 27.7 (6.4) | 26.2 (3.9) | 1.05 | 1.03 | 1.08 | 1.04 | 1.01 | 1.07 | ||||
BMI, body mass index; N, total number of patients for whom this information is available; n, number of patients in this category; OR, crude odds ratio; aOR, odds ratio adjusted for all variables included in the table.
The odds of being hospitalized was significantly higher in patients with BMI 35–39.9kg/m2 (aOR=4.37) and ≥40kg/m2 (aOR=4.95), compared with normal weight (Table 3). When BMI was taken as a continuous variable, a greater risk of hospitalization was observed with a higher BMI (aOR=1.04; 95% CI=1.01–1.07) (Table 3).
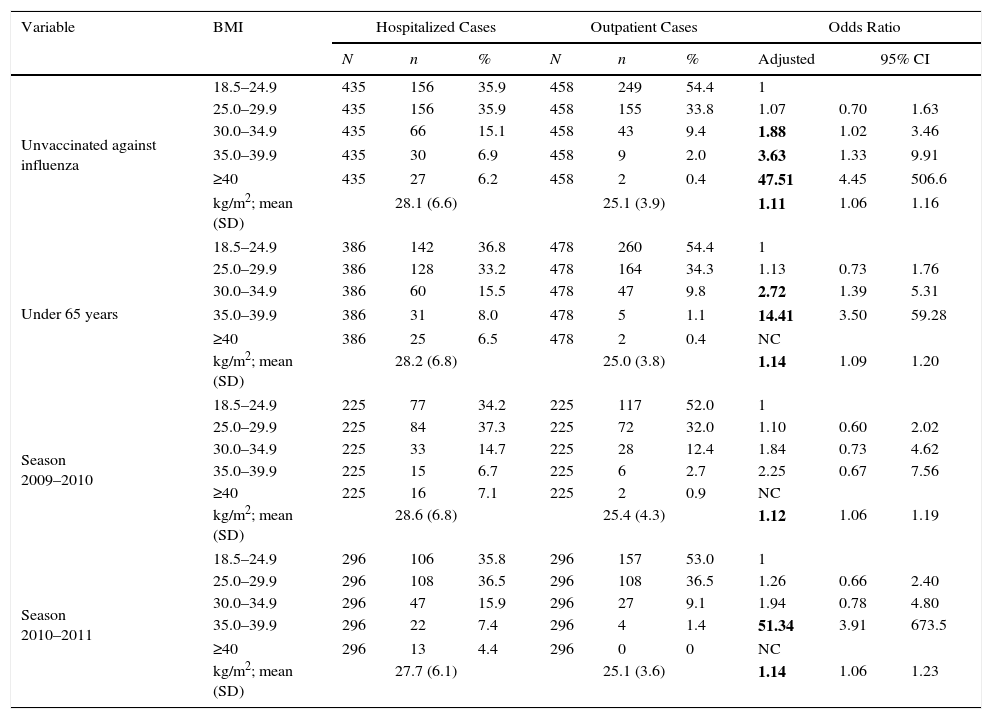
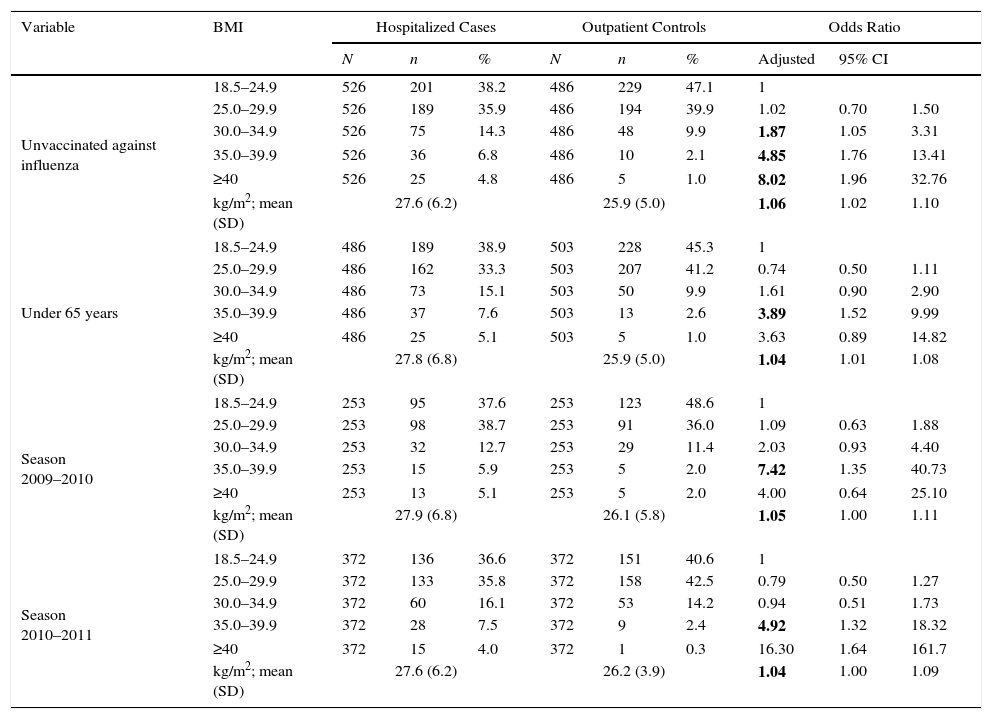
Restriction analysis: BMI was associated with an increased risk of hospitalization in patients not vaccinated against flu compared with both outpatient cases (aOR=1.11) and outpatient controls (aOR=1.06) (Tables 4 and 5). Compared with normal weight, the risk of hospitalization was increased with each BMI category from obesity grade I (BMI≥30kg/m2; aOR 1.87) to BMI≥40kg/m2 (aOR=47.51) in both comparison groups (Tables 4 and 5).
Effect of Study Variables on the Risk of Laboratory-Confirmed Influenza Hospitalization.
| Variable | BMI | Hospitalized Cases | Outpatient Cases | Odds Ratio | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | n | % | N | n | % | Adjusted | 95% CI | |||
| Unvaccinated against influenza | 18.5–24.9 | 435 | 156 | 35.9 | 458 | 249 | 54.4 | 1 | ||
| 25.0–29.9 | 435 | 156 | 35.9 | 458 | 155 | 33.8 | 1.07 | 0.70 | 1.63 | |
| 30.0–34.9 | 435 | 66 | 15.1 | 458 | 43 | 9.4 | 1.88 | 1.02 | 3.46 | |
| 35.0–39.9 | 435 | 30 | 6.9 | 458 | 9 | 2.0 | 3.63 | 1.33 | 9.91 | |
| ≥40 | 435 | 27 | 6.2 | 458 | 2 | 0.4 | 47.51 | 4.45 | 506.6 | |
| kg/m2; mean (SD) | 28.1 (6.6) | 25.1 (3.9) | 1.11 | 1.06 | 1.16 | |||||
| Under 65 years | 18.5–24.9 | 386 | 142 | 36.8 | 478 | 260 | 54.4 | 1 | ||
| 25.0–29.9 | 386 | 128 | 33.2 | 478 | 164 | 34.3 | 1.13 | 0.73 | 1.76 | |
| 30.0–34.9 | 386 | 60 | 15.5 | 478 | 47 | 9.8 | 2.72 | 1.39 | 5.31 | |
| 35.0–39.9 | 386 | 31 | 8.0 | 478 | 5 | 1.1 | 14.41 | 3.50 | 59.28 | |
| ≥40 | 386 | 25 | 6.5 | 478 | 2 | 0.4 | NC | |||
| kg/m2; mean (SD) | 28.2 (6.8) | 25.0 (3.8) | 1.14 | 1.09 | 1.20 | |||||
| Season 2009–2010 | 18.5–24.9 | 225 | 77 | 34.2 | 225 | 117 | 52.0 | 1 | ||
| 25.0–29.9 | 225 | 84 | 37.3 | 225 | 72 | 32.0 | 1.10 | 0.60 | 2.02 | |
| 30.0–34.9 | 225 | 33 | 14.7 | 225 | 28 | 12.4 | 1.84 | 0.73 | 4.62 | |
| 35.0–39.9 | 225 | 15 | 6.7 | 225 | 6 | 2.7 | 2.25 | 0.67 | 7.56 | |
| ≥40 | 225 | 16 | 7.1 | 225 | 2 | 0.9 | NC | |||
| kg/m2; mean (SD) | 28.6 (6.8) | 25.4 (4.3) | 1.12 | 1.06 | 1.19 | |||||
| Season 2010–2011 | 18.5–24.9 | 296 | 106 | 35.8 | 296 | 157 | 53.0 | 1 | ||
| 25.0–29.9 | 296 | 108 | 36.5 | 296 | 108 | 36.5 | 1.26 | 0.66 | 2.40 | |
| 30.0–34.9 | 296 | 47 | 15.9 | 296 | 27 | 9.1 | 1.94 | 0.78 | 4.80 | |
| 35.0–39.9 | 296 | 22 | 7.4 | 296 | 4 | 1.4 | 51.34 | 3.91 | 673.5 | |
| ≥40 | 296 | 13 | 4.4 | 296 | 0 | 0 | NC | |||
| kg/m2; mean (SD) | 27.7 (6.1) | 25.1 (3.6) | 1.14 | 1.06 | 1.23 | |||||
BMI, body mass index; N, total number of patients for whom this information is available; n, number of patients in this category; OR, crude odds ratio; aOR, odds ratio adjusted for all variables included in the table.
Effect of Study Variables on the Risk of Laboratory-Confirmed Influenza Hospitalization.
| Variable | BMI | Hospitalized Cases | Outpatient Controls | Odds Ratio | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | n | % | N | n | % | Adjusted | 95% CI | |||
| Unvaccinated against influenza | 18.5–24.9 | 526 | 201 | 38.2 | 486 | 229 | 47.1 | 1 | ||
| 25.0–29.9 | 526 | 189 | 35.9 | 486 | 194 | 39.9 | 1.02 | 0.70 | 1.50 | |
| 30.0–34.9 | 526 | 75 | 14.3 | 486 | 48 | 9.9 | 1.87 | 1.05 | 3.31 | |
| 35.0–39.9 | 526 | 36 | 6.8 | 486 | 10 | 2.1 | 4.85 | 1.76 | 13.41 | |
| ≥40 | 526 | 25 | 4.8 | 486 | 5 | 1.0 | 8.02 | 1.96 | 32.76 | |
| kg/m2; mean (SD) | 27.6 (6.2) | 25.9 (5.0) | 1.06 | 1.02 | 1.10 | |||||
| Under 65 years | 18.5–24.9 | 486 | 189 | 38.9 | 503 | 228 | 45.3 | 1 | ||
| 25.0–29.9 | 486 | 162 | 33.3 | 503 | 207 | 41.2 | 0.74 | 0.50 | 1.11 | |
| 30.0–34.9 | 486 | 73 | 15.1 | 503 | 50 | 9.9 | 1.61 | 0.90 | 2.90 | |
| 35.0–39.9 | 486 | 37 | 7.6 | 503 | 13 | 2.6 | 3.89 | 1.52 | 9.99 | |
| ≥40 | 486 | 25 | 5.1 | 503 | 5 | 1.0 | 3.63 | 0.89 | 14.82 | |
| kg/m2; mean (SD) | 27.8 (6.8) | 25.9 (5.0) | 1.04 | 1.01 | 1.08 | |||||
| Season 2009–2010 | 18.5–24.9 | 253 | 95 | 37.6 | 253 | 123 | 48.6 | 1 | ||
| 25.0–29.9 | 253 | 98 | 38.7 | 253 | 91 | 36.0 | 1.09 | 0.63 | 1.88 | |
| 30.0–34.9 | 253 | 32 | 12.7 | 253 | 29 | 11.4 | 2.03 | 0.93 | 4.40 | |
| 35.0–39.9 | 253 | 15 | 5.9 | 253 | 5 | 2.0 | 7.42 | 1.35 | 40.73 | |
| ≥40 | 253 | 13 | 5.1 | 253 | 5 | 2.0 | 4.00 | 0.64 | 25.10 | |
| kg/m2; mean (SD) | 27.9 (6.8) | 26.1 (5.8) | 1.05 | 1.00 | 1.11 | |||||
| Season 2010–2011 | 18.5–24.9 | 372 | 136 | 36.6 | 372 | 151 | 40.6 | 1 | ||
| 25.0–29.9 | 372 | 133 | 35.8 | 372 | 158 | 42.5 | 0.79 | 0.50 | 1.27 | |
| 30.0–34.9 | 372 | 60 | 16.1 | 372 | 53 | 14.2 | 0.94 | 0.51 | 1.73 | |
| 35.0–39.9 | 372 | 28 | 7.5 | 372 | 9 | 2.4 | 4.92 | 1.32 | 18.32 | |
| ≥40 | 372 | 15 | 4.0 | 372 | 1 | 0.3 | 16.30 | 1.64 | 161.7 | |
| kg/m2; mean (SD) | 27.6 (6.2) | 26.2 (3.9) | 1.04 | 1.00 | 1.09 | |||||
BMI, body mass index; N, total number of patients for whom this information is available; n, number of patients in this category; OR, crude odds ratio; OR, odds ratio adjusted for all variables included in the table.
BMI as a quantitative variable was associated with an increased risk of hospitalization in patients younger than 65 years in both comparison groups (aOR=1.14 and aOR=1.04) (Tables 4 and 5). Compared with normal weight, a risk of hospitalization was observed in obesity grade II (aOR=14.41; aOR=3.89) in both comparison groups, compared with outpatient cases also in the category of BMI 30–34 (aOR=2.72).
Similarly, in the two seasons studied, BMI was associated with a risk of hospitalization in both comparison groups (aOR=1.12 and aOR=1.14; aOR=1.05 and aOR=1.04). Compared with normal weight, BMI≥35kg/m2 was associated with an increased risk of hospitalization (Tables 4 and 5) in both seasons.
Fraction of hospitalized cases of influenza attributable to BMI: In patients infected by influenza, comparison of hospitalized cases and outpatient cases showed that the PAF of hospital admission for BMI was 21.9%. Comparison of hospitalized cases and outpatient controls showed a PAF of hospitalization for influenza for BMI of 8.5%. In patients unvaccinated against influenza, the contribution of BMI to hospitalization for influenza ranged between 20.5% and 16.9% depending on the type of comparison.
DiscussionObesity emerged as an independent risk factor for severity and death in the influenza A (H1N1)pdm09 pandemic, possibly due to factors associated with the influenza strain or because a certain prevalence of obesity that facilitated detection of the association was reached.14–18 Although it is not completely clear why obesity is associated with a higher frequency of infections, especially respiratory infections, some immunological and mechanical hypotheses have been put forward.18,19
One possible explanation is the association between obesity and the overexpression of adipokines, leading to a low-grade inflammatory state that impairs both the innate and adaptive immune responses.18,20,21 In addition, excess fat accumulated in the chest and abdomen reduces residual functional capacity and pulmonary compliance and impairs ventilation and perfusion. This mechanical dysfunction may also explain the increased risk of respiratory infections and the increased severity of influenza in obese subjects.18,22
This study, which compared patients hospitalized due to influenza with two types of outpatient controls, found that increases in BMI were associated with a greater risk of hospitalization, especially, and significantly, in patients with a BMI≥35kg/m2 and in those who were not vaccinated against influenza; therefore BMI plays a role in a significant proportion of patients hospitalized for influenza, especially in unvaccinated patients.
Several authors have already shown that a BMI≥40kg/m2 is an important risk factor for influenza severity and vaccination is recommended in these patients. In our series, we have seen how patients with BMI between 35 and 40kg/m2 presented a significant risk of hospitalization, around 5-fold that of normal weight, in all comparisons and subgroups studied. Several studies found no relationship between obesity and the risk of influenza infection, and the lack of relevant data in our study does not allow us to draw conclusions on this matter.23
The risk of hospitalization attributable to BMI was particularly high in patients who were not vaccinated against influenza. In these subjects, the risk of hospitalization was significant, even in patients with a BMI between 30 and 34.9kg/m2, and twice that of patients with normal weight in both comparisons. The higher prevalence of type I obesity than type II or higher calls for greater attention to this group of patients in view of its impact on PAF.
Our results are in agreement with those of Kwong et al.,24 who retrospectively studied 12 influenza seasons and found that a BMI≥30kg/m2 increased the risk of hospitalization for respiratory disease and a BMI≥35kg/m2 increased the risk of hospitalization in patients with or without comorbidities. In Brazil during the 2009–2010 pandemic, Lenzi et al.25 analyzed more than 4000 confirmed cases of influenza and found that the risk of hospitalization was 3-fold higher in subjects with BMI≥40kg/m2. Similarly, González-Candelas et al.26 compared hospital and outpatient cases during the 2009–2010 pandemic and found that the risk of hospitalization was 14-fold higher in subjects with BMI≥40kg/m2. A case-cohort study by Morgan et al.16 found that a BMI≥40kg/m2 was associated with an increased risk of hospitalization in subjects aged ≥20 years, both in cases with comorbidities recognized by the Advisory Committee on Immunization Practices and in patients without comorbidities (OR=4.9 and 4.7, respectively), but not in the case of BMI 30–39.9kg/m2.
In contrast, Gilca et al.27 compared hospitalized and outpatient cases of influenza in the 2009–2010 season and found that both BMI≥30kg/m2 and BMI≥40kg/m2 were associated, in the univariate analysis, with an increased risk of hospitalization (OR=2.2 and 3.1, respectively). However, the association was lost in the multivariate analysis, leading the authors to conclude that the independent role of obesity needs to be further defined. Other authors have not found this association.28,29
BMI correlates well with the percentage of body fat, especially when BMI≥35kg/m2.30 BMI is simple and inexpensive to obtain and there are well-established relationships with various causes of morbidity and mortality.31 For BMI<35kg/m2, the correlation with body fat is affected by gender, age and ethnicity, so the prevalence of overweight and obesity grade I is underestimated.30,32,33 Likewise, the role of body fat varies according to sex and age.34 These factors make it difficult to determine whether the different risk of hospitalization detected according to sex and age in people with a BMI 30–34.9kg/m2 is due to a classification problem or to the different role fat plays in these subjects. People aged <18 years and pregnant women were excluded from the study in order to avoid problems concerning the classification and validity of the BMI as an index for evaluating obesity. Cases of suspected nosocomial infection were also excluded, as main objective of the study was to investigate the prevention of influenza virus infection in the community.
The results of the analysis in specific subgroups of patients highlight two factors. First, unvaccinated patients with a BMI≥30kg/m2 are at risk for hospitalization while vaccinated patients are not. Evaluation of the effectiveness of the vaccine in people with a BMI≥30kg/m2 is beyond the scope of this study, but the results obtained suggest that the influenza vaccine protects obese individuals against hospitalization due to influenza, underlining the need for vaccination in these patients.8 Secondly, the risk of hospitalization in patients with a BMI≥30kg/m2 is particularly high in patients under 65 years, which also strengthens the recommendation of vaccination.8
In interpreting the results of this study, some possible limitations should be kept in mind. It is an established fact that case control studies do not provide a high level of evidence, due to the multiple biases that may be incurred, however, the aim of the research project was to rapidly detect risk factors and protective factors for influenza A (H1N1) 2009, and for this reason this design was selected. Another factor to take into account is that the study of obesity as a risk factor was not originally a study objective, but instead emerged as a secondary objective from the findings. This approach leads to a loss of power, because pairings were split when restriction criteria were used (adults, non-pregnant subject, etc.), so it seems very likely that the biases which were introduced tend towards nullity and do not invalidate the validity of the results.
The main limitation is that the study subjects were patients who sought medical help, so we do not know the real number of infected persons and their characteristics with respect to BMI. Outpatient cases were detected through the sentinel physicians who selected patients to take swabs according to a systematic approach, although patients who visit the physician more frequently may have been overrepresented. The cases and controls were included in the study when they requested medical attention, and this may have contributed to them being more alike in the use of health services. However, the care-seeking patterns could have had some influence on the comparisons between outpatients and inpatients.
The interviewers were aware of whether interviewees were cases or controls and this could have influenced information gathering. However, the same protocol was followed in cases and controls, and information was collected from clinical records, vaccination cards or registers recorded before the study began and referred to the date of hospitalization of the case, and therefore a significant information bias is unlikely.
Finally, the 2010–2011 season predominantly saw the circulation of influenza A (H1N1)pdm09, and the pattern of involvement may be somewhat different from other influenza viruses. It would be interesting to compare these findings in other seasons to determine whether the same results are obtained.34,35
ConclusionA higher BMI was associated with a worse outcome of influenza infection, with a higher risk of hospitalization, especially in patients with a BMI≥35kg/m2. A high percentage of hospitalizations for influenza in patients with a BMI≥35kg/m2 are due to this factor. This suggests that individuals aged >18 years with a BMI≥35kg/m2 should be considered a risk group for influenza infection. For people with a BMI between 30 and 34.9kg/m2, the risk of hospitalization is also higher in unvaccinated subjects and under 65 years, although this association is weaker.
Conflict of interestThe authors declare no conflicts of interest.
FundingThis study was supported by the Ministry of Science and Innovation, Institute of Health Carlos III, Programme of Research on Influenza A/H1N1 (Grant GR09/0030), and the Catalan Agency for the Management of Grants for University Research (AGAUR Grant number 2009/SGR 42).
We thank the physicians of the Sentinel Network of the participating Spanish regions and the study interviewers for their help and collaboration.
Thanks to Veronica Davila for her help in revising the manuscript.
Andalusia: E Azor, J Carrillo, R Moyano, JA Navarro, M Vázquez, F Zafra (Médico Centinela), MA Bueno, M Delgado, ML Gómez, M Mariscal, B Martínez, JP Quesada, M Sillero (Compl. Hosp. Jaén), M Carnero, J Fernández-Crehuet, J del Diego Salas (Hosp. Virgen de la Victoria), V Fuentes (Hosp. Costa del Sol), V Gallardo, E Pérez (Servicio de Epidemiología), R López (Hosp. Infanta Elena de Huelva), JR Maldonado (Hosp. Torrecárdenas), A Morillo (Hosp. Virgen del Rocío), I Pedrosa Corral, MF Bautista, JM Navarro, M Pérez (Lab. Referencia Gripe), S Oña (Hosp. Carlos Haya), MJ Pérez (Hosp. Virgen de Valme), MC Ubago (Hosp. Virgen de las Nieves), M Zarzuela (Hosp. Puerta del Mar), JM Mayoral (Servicio de Vigilancia de Andalucía).
Castile and Leon: T Fernandez, V Martín, A Molina, P Sanz (Universidad de León), D Carriedo, F Díez, I Fernández-Natal, S Fernández (Compl. Asist. Universitario, León), JJ Castrodeza, A Pérez, S Tamames (Dir. General de Salud Pública e Investigación, Desarrollo e Innovación), R Ortiz de Lejarazu (Centro Nacional de Gripe, Valladolid), J Ortiz de Saracho (Hosp. El Bierzo), A Pueyo, JL Viejo, (Compl. Asist. Burgos), P Redondo (Serv. Territorial de Sanidad y Bienestar Social, León).
Catalonia: A Domínguez (Universitat de Barcelona), A Agustí, A Torres, A Trilla, A Vilella (Hosp. Clínic); F Barbé (Hosp. Arnau de Vilanova); L Blanch, G Navarro (Hosp. Sabadell); X Bonfill, J López-Contreras, V Pomar, MT Puig (Hosp. Sant Pau); E Borràs, A Martínez, N Torner, P Godoy (Dir. General de Salud Pública); C Bravo, F Moraga (Hosp. Vall d’Hebrón); F Calafell (Universitat Pompeu Fabra); J Caylà, C Tortajada (Agencia de Salud Publica de Barcelona); I Garcia, J Ruiz (Hosp. Germans Trias i Pujol); JJ García (Hosp. Sant Joan de Deu); M Baricot, N Soldevila, O Garín (CIBERESP); J Alonso (IMIM- Hosp. del Mar), J Gea, JP Horcajada (Universitat Pompeu Fabra _CIBER Enfermedades Respiratorias); T Pumarola (Red Esp. Inv. en Patología Infecciosa); N Hayes (Hosp. Clínic_CRESIB); A Rosell, J Dorca (Hosp. de Bellvitge), Marc Saez (Universidad de Girona).
Madrid Community: A Castro (CIBER Enfermedades Respiratorias); C Álvarez, M Enríquez, A Hernández Voth, F Pozo (Hosp. 12 de Octubre), F Baquero, R Cantón, JC Galán, A Robustillo, M Valdeón (Hosp. Universitario Ramón y Cajal); J Astray, E Córdoba, F Domínguez, M García Barquero, J García, R Génova, E Gil, S Jiménez, MA Lopaz, J López, F Martín, ML Martínez, M Ordobás, E Rodriguez, S Sánchez, C Valdés (Área de Epidemiología, Comunidad de Madrid), JR Paño, M Romero (Hosp. Universitario La Paz).
Navarre: J Castilla, A Martínez, L Martínez (Inst. de Salud Pública), M Ruiz, P Fanlo, F Gil, V Martínez-Artola (Compl. Hosp. Navarra), ME Ursua, M Sota, MT Virto, J Gamboa, F Pérez-Afonso (Médicos Centinelas).
The Basque Country: U Aguirre, A Caspelastegui, PP España, S García, JM Quintana (Hosp. Galdakao), JM Antoñana, I Astigarraga, JI Pijoan, I Pocheville, M Santiago, JI Villate (Hosp. Cruces), J Arístegui, A Escobar, MI Garrote (Hosp. Basurto), A Bilbao, C Garaizar (Fundación Vasca de Innovación e Investigación Sanitarias), G Cilla, J Korta, E Pérez-Trallero, C Sarasqueta (Hosp. Donostia), F Aizpuru, JL Lobo, C Salado (Hosp. Txagorritxu), J Alustiza (Hosp. Mendaro), F J Troya (Hosp. de Santiago).
Valencia Community: F González (Universidad de Valencia), J Blanquer (Hosp. Clínico), M Morales (Hosp. Doctor Peset).
Please cite this article as: Martín V, Castilla J, Godoy P, Delgado-Rodríguez M, Soldevila N, Fernández-Villa T, et al. Índice de masa corporal alto como factor de riesgo de hospitalización por gripe: estudio de casos y controles. Arch Bronconeumol. 2016;52:299–307.