The present guidelines have been prepared with the consensus of at least one representative of each of the hospitals with lung transplantation programs in Spain. In addition, prior to their publication, these guidelines have been reviewed by a group of prominent reviewers who are recognized for their professional experience in the field of lung transplantation. Within the following pages, the reader will find the selection criteria for lung transplantation candidates, when and how to remit a patient to a transplantation center and, lastly, when to add the patient to the waiting list. A level of evidence has been identified for the most relevant questions. Our intention is for this document to be a practical guide for pulmonologists who do not directly participate in lung transplantations but who should consider this treatment for their patients. Finally, these guidelines also propose an information form in order to compile in an organized manner the patient data of the potential candidate for lung transplantation, which are relevant in order to be able to make the best decisions possible.
La presente normativa ha sido elaborada con el consenso de, al menos, un representante de cada uno de los hospitales con programa de trasplante pulmonar en España. Además, previamente a su publicación, ha sido revisada por un grupo de revisores destacados por su reconocida trayectoria en el campo del trasplante pulmonar. En las siguientes páginas, el lector encontrará los criterios de selección de pacientes candidatos a trasplante pulmonar, cuándo y cómo remitir un paciente a un centro trasplantador y, finalmente, cuándo incluir al paciente en lista de espera. Se ha atribuido un nivel de evidencia a las cuestiones más relevantes. Este documento pretende ser una guía práctica para los neumólogos que no participan directamente en el trasplante pulmonar pero que deben considerar este tratamiento para sus pacientes. Finalmente, se ha propuesto de una forma consensuada un documento que recoge de forma estructurada los datos del paciente potencial candidato a trasplante pulmonar que son relevantes para poder tomar la mejor decisión.
Lung transplantation (LT) is a well-consolidated treatment option in patients with advanced chronic respiratory diseases. LT has been implemented in the majority of developed countries for more than 15 years and many developing countries are initiating their own programs. The data indicate that it is a growing activity.1 An approximate calculation situates the world-wide activity in around 2900-3000 LT per year. In Spain, leader in the generation of organs thanks to a conscientious society and a genuinely coordinated system, LT has likewise undergone development. Our country, which represents approximately 0.8% of the world-wide population, performs about 6% of the LT that are done annually the world over. This amount, close to 200 annual LT, has all the signs of being surpassed in the near future, offering patients in chronic respiratory failure the possibility of benefitting from LT.
Which patients are adequate candidates and which are not, when and how they should be referred to an LT center in order to have real possibilities of benefiting from this treatment are all questions that have evolved over time. For the last 11 years, there have been international guidelines in place for the selection and study of potential LT candidates, the last of these published in 2006.2 This document has been conceived in order to be a practical guide for the pulmonologists who treat adult patients in chronic respiratory failure, regardless of whether they are involved or not in LT.
It is important to admit that there are no data from controlled clinical assays in order to establish the recommendations on the selection of candidates for LT. In fact, the majority of the recommendations of this document are based on expert opinions, retrospective studies of a center or multiple centers and national and international registers. These recommendations are naturally influenced by our experience in Spain and are also dependent upon the availability of organs.
The responsibility placed by the community on the transplant groups includes putting the candidates on the recipient list at the proper time and, possibly, withdrawing them if it is predictable that the patient will not benefit from LT. Thus, taking into account the limitations inherent of organ availability, LT should be indicated only in patients capable of bearing it, and should be avoided in the patients with few possibilities of surviving the procedure.
From a methodological viewpoint, these guidelines have been drawn up in the following manner: (1) initial manuscript evaluated individually by the authors; (2) meeting of the authors in order to discuss the document; (3) second version incorporating the modifications agreed upon in the meeting; (4) review by external experts; and, finally, (5) acceptance of the final document by the authors.
Patient SelectionIndicationsLT is indicated in patients with advanced respiratory diseases that progress despite the maximum pharmacological treatment possible. The potential candidates must be capable of comprehending the procedure, undergoing the selection process and waiting the time necessary on the waiting list while being in a physical condition that allows specialists to predict a potential benefit from LT.
The main objective is to improve the survival of the patients and this has been documented in patients with cystic fibrosis (CF), pulmonary fibrosis (PF) and pulmonary arterial hypertension (PAH).3 This improvement in survival does not seem to be as clear in patients with emphysema.4,6
How to achieve a balance between the improvement in survival and greater quality of life is a question that has not been totally resolved. In these guidelines, we consider that LT should improve both.5 Except in exceptional cases, adding patients to waiting lists merely due to criteria based on quality of life does not seem to be adequate.2
Absolute Contraindications for Lung TransplantationThe following conditions are considered absolute contraindications, as they make it quite improbable for the patient have a greater life expectancy with LT.
- 1.
Neoplasm in the previous 2 years, with the exception of basocellular and spinocellular carcinoma.
- 2.
A disease-free period of 3-5 years is recommended. Lung neoplasm contraindicates LT. However, its indication in bronchioloalveolar carcinoma is controversial and needs to be evaluated individually.
- 3.
Advanced and irreversible cardiac, hepatic and renal deterioration. In these cases, the possibility of a combined transplantation could be considered.
- 4.
Ischemic heart disease with poor ventricular function. Treatable coronary lesions are permitted as long as they resolve the problem, do not present complications and the ventricular function is not affected.
- 5.
Incurable extrapulmonary infection that includes infection by the human immunodeficiency virus and some cases of hepatitis B and C.
- 6.
Important ribcage deformities progressive neuromuscular disease.
- 7.
Patients with demonstrated and reiterated poor therapeutic compliance, which predict the persistence in this conduct after LT.
- 8.
Major psychiatric disorder or absence of social support that foresee difficulties in the follow-up and treatment.
- 9.
Addiction to toxic substances (alcohol, tobacco or others). The patients can be accepted as long a sufficient period of abstinence has passed and the possibilities for relapse are slim.
These conditions can mean an increase in risk for LT, and therefore each transplant group, depending on experience, will make their own decisions.
- 1.
Age over 65 for the unilateral lung transplantation, over 60 for bilateral lung and over 55 for cardiopulmonary transplantation. The last international consensus advocates that age not be an absolute contraindication for LT2 while advocating individualized evaluations, keeping in mind that, in patients with no comorbidity and with good physical condition, age may not be a strong enough argument against LT, despite the fact that older patients have poorer post-op survival than younger ones.
- 2.
Clinical state at the moment of notification or referral: hemodynamic instability, invasive mechanical ventilation or membrane oxygenator support, in a patient that previously has not been evaluated for LT. The contraindication due to invasive mechanical ventilation in a previously evaluated patient will be the decision of each team according to the characteristics of the patient. Non-invasive home mechanical ventilation is not considered a contraindication for LT.
- 3.
Excessive physical deterioration that impedes performing outpatient rehabilitation or severe muscle atrophy, which predicts the failure of the extubation after LT.
- 4.
Colonization by multi-resistant or pan-resistant bacteria a, fungus or mycobacteria.
- 5.
Obesity defined as a body mass index higher than 30kg/m.2
- 6.
Other medical conditions such as diabetes mellitus, high blood pressure, peptic ulcer, gastroesophageal reflux or symptomatic osteoporosis should be properly treated before LT.
When a patient with severe chronic respiratory disease presents an important functional deterioration and is predicted to have a possibility of surviving of 50% or less in the next 2-3 years, this is the moment to contact an LT center. The real possibilities for survival on the waiting list depend on data that are well-known by transplantation teams, but not necessarily by the pulmonologists who make the referrals. Among other factors, it depends on the transplant activity of each center, the availability of donors, the baseline disease of the patient, the type of transplantation and some personal characteristics, such as AB0 group and size.
In Spain, generally the patients who have a longer wait are those who are candidates for bilateral lung transplantation, those who are short in stature and those of blood group 0. Therefore, it is better to consider LT sooner than later as it avoids hasty decisions by the patient or the transplantation team. In fact, the evaluation of the possible LT candidate includes an overall study of the patient by a multidisciplinary team that analyzes the details of the respiratory disease and the comorbidities of the patient and, in addition, a process of education that is extremely important and should be done with plenty of time.
The decision to remit a patient for LT cannot be based on a single factor. We must always take into account certain factors, such as frequency of infections, number of hospitalizations and severity, the need for oxygen, weight loss, the presence or not of hypercapnia, lung function data, exercise capacity and the opinion of the patient. Thus, we consider it to be especially useful to differentiate some defined referral criteria, such as those that recommend sending the patient information to a transplant team in order to adequately initiate the evaluation, and some transplantation criteria that identify the ideal moment in which the patient should be included on a waiting list by the corresponding transplant team.
Specific Considerations of Each DiseaseThe available evidence for making recommendations of when to remit a patient for LT does not include high-quality studies or clinical assays. Therefore, all the recommendations of the present consensus are based on studies of registers, patient cohorts and expert opinions and have a moderate quality of evidence.
Chronic Obstructive Pulmonary DiseaseChronic obstructive pulmonary disease (COPD) is the most frequent indication for LT worldwide.1 LT in a patient with COPD should be considered when, despite the maximum pharmacological treatment possible, the patient continues to deteriorate. In this disease, to define the adequate time for LT is difficult because some very symptomatic patients may have a good prognosis, while others, despite very altered spirometric values, can present a very acceptable quality of life.
After hospitalization due to an acute hypercapnic exacerbation, a 2-year survival has been described of 49%.7 The American clinical assay on lung volume reduction surgery demonstrated that the patients with forced expiratory volume in one second (FEV1) less than 20% and carbon monoxide diffusing capacity (DLCO) less than 20% or homogeneous emphysema had a mean survival of 3 years.8 It is demonstrated that the possibilities for survival in COPD decrease with the age of the patient and the degree of hypoxemia and hypercapnia. Likewise, there is an observed progressive increase in the pulmonary artery pressure as FEV1, DLCO and body weight decrease.7 Also, the measurement of the health-related quality of life is able to predict mortality.9 The most modern approach to the prognosis of COPD has been done by means of the BODE index (Body, Obstruction, Densitometry, Exercise), a scale that analyses these parameters and goes from 0 to 10 points. It has been confirmed that patients with a BODE between 7 and 10 have a mortality of 80% in 52 meses.10
There are no prospective studies that evaluate the BODE in LT. A retrospective LT study showed that the candidate patients for LT in our setting presented a BODE between 7 and 10.11 In another study, almost 30% of the patients transplanted for COPD would be excluded if the only criteria for LT had been a BODE index equal to or higher than 7.12 We then consider that the BODE index has been an important advance in the multidimensional evaluation of COPD, but it does not contemplate some parameters that also have prognostic importance, such as the number of exacerbations, especially if they are accompanied by hypercapnia or the presence of pulmonary hypertension with signs of right cardiac failure.13
In the light of these observations, we indicate for COPD patients:
- 1.
Referral: (consistent recommendation, moderate quality of evidence) BODE higher than 5.
- 2.
Transplantation: (consistent recommendation, moderate quality of evidence) BODE 7-10 and one of the following:
- ∘
Hospitalization with documented hypercapnia (pCO2>50mmHg).
- ∘
Cor pulmonale.
- ∘
FEV1<20% and DLCO<20% or diffuse homogenous emphysema.
- ∘
Diffuse interstitial lung disease (ILD) is a group of diseases among which idiopathic PF (IPF) or unusual interstitial pneumonia (UIN) represent the second indication of LT.1 It is calculated that patients with IPF live on average 2-4 years after the diagnosis and are the group of patients with the highest mortality on the waiting list.1 The histological diagnosis is important as the forms of ILD other than UIN present better prognoses. The histology of UIN also identifies the patients with poorer prognosis.14,15 In contrast, the patients with non-specific interstitial pneumonia (NSIP) histology have a better prognosis that worsens as the NSIP presents features of UIN.16 Thus, the international recommendation2 and that of this consensus is that patients with IPF be remitted to an LT center as early as possible.
Both UIN as well as NSIP are usually idiopathic, but they are also observed associated with diseases of the connective tissue such as scleroderma, rheumatoid arthritis or mixed connective tissue disease. In this case, the prognosis is as uncertain as in the case of the idiopathic forms and, therefore, the time to refer a patient with a systemic disease and lung affectation follows the same severity parameters as in the idiopathic forms. In practice, the indication of LT due to systemic disease with pulmonary affectation represents a small percentage of the total1 and, consequently, the published LT results in this group of patients are more limited.17
Another important prognostic factor is lung function and effort capacity. The presence of an FVC lower than 60% has been associated with an increase in mortality,18 although recent studies observe that the mortality of patients with good lung volumes is similar to that observed in patients with low FVC.19 It is probably better to make a prognostic judgment from the serial lung function measurements of the patients. Recent studies show that the decrease in FVC other lung function parameters or oxygen saturation (SaO2) are associated with greater mortality. A decrease in FVC of more than 10% in 6 months would identify those patients with higher mortality with a positive predictive value of 31% and a negative predictive value of 91%.20 It is important to consider that, in practice, some patients can present a rapid deterioration that can lead to death in a short period of time.21 Similar data have been observed in patients with fibrotic forms of NSIP. Also, DLCO less than 40% has been identified as a parameter to predict greater risk for death.22 SaO2 less than 88% during the 6min walk test identified a subgroup of patients with UIN and poor prognosis.23 The radiological appearance on the computed tomography (CT) also helps to establish the prognosis in such as way that the patients that present clear images of UIN-type fibrosis have a poorer prognosis.24
The patients with UIN today do not have a pharmacological treatment able to improve the course of the disease. Clinical assays have been completed with prednisone,25 prednisone plus azathioprine,26 colchicine,25 interferon gamma,27 pirfenidone,28 etanercept29 and bosentan.30 In addition, there are currently several assays in progress that include cell therapy, the results of which are expected in coming years. Meanwhile, patients with UIN or NSIP should be referred without delay to an LT center even if they are participating in a clinical assay.
- 1.
Referral (consistent recommendation, moderate quality of evidence):
- ∘
Histological or radiological evidence of UIN, regardless of FVC.
- ∘
Histological evidence of fibrotic NSIP.
- ∘
- 2.
Transplant (consistent recommendation, moderate quality of evidence):
- ∘
Histological or radiological evidence of UIN and at least one of the following criteria:
▪DLCO less than 40%.
▪Decrease of 10% or more in FVC in 6 months.
▪Decrease in SaO2 under 88% in the 6min walk test.
▪Presence of honeycomb images on chest CT.
- ∘
Histological evidence of NSIP and one of the following:
▪DLCO less than 35%.
▪Decrease of 10% or more in FVC or decrease in 15% of DLCO in 6 months.
- ∘
CF is one of the three most frequent indications for LT.1 The most important differential fact in this group of patients is the presence of chronic bronchial infection with colonization of the upper airway and paranasal sinuses, a fact which probably increases the post-operative risk for infections by these germs. In addition, the multisystemic affectation of CF makes this population peculiar. Despite all these added problems, it should be stated that the survival of CF transplanted patients is very good, in adults as well as in children.4,31–39 The infections by germs that are resistant to antibiotics can increase the risk of LT for these patients although this fact does not constitute an absolute contraindication for LT. It has been reported that the colonization by pan-resistant Pseudomonas aeruginosa does not influence the short-term results of LT.37,40–42 Nor are the colonizations by resistant Staphylococcus aureus meticilin, Stenotrophomonas maltophilia, Alcaligenes xylosoxidans or Aspergillus fumigatus2 considered contraindications. The exception seems to lie in those patients colonized by Burkholderia cepacia complex, who present higher post-op mortality,40,43 particularly genomovar III.44 Care of these patients should include periodic antibiograms, particularly while on the waiting list, in order to better identify the optimal combination of antibiotics as prophylaxis during the LT process.
The hepatopathy that accompanies these patients is not usually sufficiently severe enough to impede performing LT in most cases. The presence of the same usually does not have prognostic impact on survival of CF patients, as long as it is not an advanced hepatopathy. In case of severe hepatic deterioration, a multidisciplinary evaluation with the hepatic transplant team is the proper approach.
The need for invasive mechanical ventilation in patients that are on the waiting list and, therefore, have been evaluated and accepted, is not an absolute contraindication for LT, although the fact of the ventilation probably supposes accepting an increased risk in the intervention.1,45,46 In any event, it is totally desirable to try to avoid this situation. In the case that a patient with CF on a waiting list for LT needs mechanical ventilation, this should be done only under the following circumstances: 1) the patient was evaluated before the mechanical ventilation, as there is no protocol for LT evaluation validated in patients in this situation; 2) the patient and the family should know that the worsened state after ventilation could obligate the patient being withdrawn from the waiting list; 3) the patient should not have other damaged organs that compromise the success of the LT; and lastly, 4) the patient and the family need to accept the mechanical ventilation.
From the earliest studies until now, the prognostic factors in CF have slowly improved. In fact, two large cohort studies in American patients have been able to predict the 2- and 5-year survivals, although with discrepant results.32,47 In the second study,47 the model has a modest predictive power, no higher than what can be predicted by an FEV1 lower than 30%. This difficulty in developing reliable prognostic models probably lies in the fact that the prognosis of CF is highly variable between different individuals, as corresponds to a complex disease with multisystemic affectation.
In the clinical practice, in order to make an adequate decision about when to remit the patient to an LT center, one must consider the usual prognostic variables as well as the opinion of the patient and family. It is clear that one must remit the patients with an FEV1 of less than 30% or who rapidly worsen and after the hospital discharge of a patient hospitalized in the ICU for a severe exacerbation.48 An attempt must be made at referring young female patients earlier because it is accepted that they present poorer prognoses.49 The final decision of LT will take into account several factors, such as FEV1, the need for oxygen, the presence or not of hypercapnia, the need for non-invasive ventilation, the clinical course of the patient and history of exacerbations, the functional state and the situation of the rest of the economy of the patient.
- 1.
Referral (consistent recommendation, moderate quality of evidence):
- ∘
FEV1 less than 30% or rapid descent, especially in young women.
- ∘
Exacerbation requiring ICU hospitalization.
- ∘
Increase in the frequency of exacerbations requiring antibiotics.
- ∘
Recurring or refractory pneumothorax
- ∘
Recurring hemoptysis or hemoptysis that is not well controlled with bronchial embolization.
- ∘
Uncontrollable malnutrition with no other cause than chronic bronchial infection.
- ∘
- 2.
Transplant (consistent recommendation, moderate quality of evidence):
- ∘
Respiratory failure that requires continuous oxygen therapy.
- ∘
Presence of hypercapnia.
- ∘
Presence of PAH.
- ∘
PAH is a severe progressive disease that, in its final phases, courses with right ventricular failure as the fundamental cause of death in these patients. The natural history of the disease without treatment, described in the 1980s,50 established a mean survival of 2.8 years. During the 80s and the 90s, LT was the only available treatment and a significant number of patients in Europe received cardiopulmonary, unilateral or, fundamentally, bilateral lung transplants.51 The same happened in Spain.52 At the end of the 90s, the life expectancy of these patients clearly improved thanks to the combination of three pharmaceutical drug families. This meant that the previous 10% of LT indicated due to lung hypertension was reduced to the current 3%.1 Nevertheless, despite such important advances, the disease still has no cure and we have to consider that LT is still a very important tool for the treatment of patients with poor evolution, as reflected by an international consensus on the diagnosis and treatment of this disease.53,54
When to consider LT in patients with PAH is a difficult question in clinical practice. Although there are known prognostic factors that aid in decision-making, choosing the right moment for remission to a transplantation center and, especially, deciding the moment when the patient should be transplanted are two questions that have yet to be resolved in the literature. Within the prognostic factors, it is well-known that patients with PAH associated with scleroderma have poorer prognoses than patients with PAH associated with a congenital cardiopathy or patients with idiopathic PAH. The functional class as well as the distance walked in the 6min walk test correlate well with survival in patients with idiopathic PAH. The lung hemodynamics can identify a small percentage of patients who are capable of responding to a vasodilator test and who present a good prognosis. The classic article by D’Alonzo et al.50 reported that the presence of a cardiac index less than 2l/min/m2 and a mean right auricle pressure higher than 20mmHg identified the patients with poor prognosis. The presence of these hemodynamic data are not able to predict the response to pharmacological treatment, which should always be initiated and be maximized in accordance with the established international guidelines.53–55 The close contact between the pulmonary hypertension reference unit and the transplant center is very important to be able to offer LT at the appropriate time.
- 1.
Referral (consistent recommendation, moderate quality of evidence):
- ∘
Functional class III or IV (NYHA) and poor response to treatment.
- ∘
Rapidly progressive disease.
- ∘
Need for treatment with intravenous prostacyclins.
- ∘
- 2.
Transplantation (consistent recommendation, moderate quality of evidence):
- ∘
Persistence of class III or IV despite the maximum medical treatment possible.
- ∘
6min walk test <300m or progressive worsening.
- ∘
No response to epoprostenol or equivalent.
- ∘
Hemodynamic signs of poor prognosis.
- ∘
LT is feasible in all chronic respiratory diseases that evolve with progressive, invalidating respiratory failure. Among these diseases, we can highlight for their frequency bronchiectasis, sarcoidosis, lymphangioleiomyomatosis and Langerhans cell histiocytosis. Lung neoplasms contraindicate LT, although the eventual indication of LT is controversial in patients with localized bronchioloalveolar carcinoma. In general, we consider in this consensus that the same general principles for LT indication should be applied for these less prevalent pathologies when a poor prognosis can be established in the patient at 1-2 years and there is no contraindication for LT.
- 1.
Referral (consistent recommendation, low quality of evidence):
- ∘
Dyspnea upon low-medium effort.
- ∘
Discussion with the LT team about indication.
- ∘
- 2.
Transplantation (consistent recommendation, low quality of evidence):
- ∘
Poor lung function and dyspnea upon low-grade effort.
- ∘
In general, when there is a need for continuous oxygen therapy.
- ∘
The final decision on the indication of LT in each specific patient will be established by the multidisciplinary team of the hospital specialized in LT, which will also manage the moment of the inclusion and possible exclusion from the waiting list. Therefore, when a pulmonologist who does not belong to an LT group is contemplating this possibility for one of his/her patients, he/she should propose the referral to an LT center only after being convinced that the patient meets the criteria defined in these guidelines. In cases of doubt, it is extremely recommendable to contact the transplant center directly in order to discuss the patient's possibilities. The proposition of this procedure is to avoid the creation of false expectations in some patients.
LT should be posed as a possibility that competes with optimal pharmacological treatment that the patient already receives. It should also be emphasized that the final decision, whatever it may be, will be the best to help him/her as much as possible. Certainly the patient should be encouraged to accept the LT challenge, but it is not correct to set forth LT in any case as either a cure-all or as the only possibility to keep on living. It is disheartening for LT specialists to have to inform a patient that their case has been rejected for lung transplantation. After almost 30 years of LT in the world, this technique continues to be a treatment for selected patients who, when adequately informed, are able to accept the procedure and have the capability to overcome the wait and the intervention.
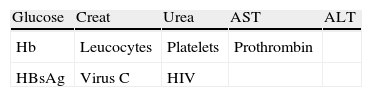
Patients should be referred with complete clinical reports, including all the fundamental clinical and personal data (Appendix A).
Conflict of InterestThe authors declare having no conflict of interests.
Personal data:
Name:
Address:
Telephone numbers (home/mobile):
Doctor making the referral:
Sex:
Age:
Weight:
Height:
BMI:
Diagnosis and lung function parameters
Functional class (NYHA):
Home OT (yes/no): start date:
NIMV (yes/no): start date:
FVC (ml/%):
FEV1 ml/%):
DLCO (%):
Arterial blood gas (FiO2): PaO2: PaCO2: pH:
Medical history
Allergies (yes/no): Type:
Tobacco habit (packs/year): Quit date:
Arterial hypertension (yes/no): Treatment:
Tuberculosis (yes/no): Treatment:
Diabetes (yes/no): Treatment:
Dyslipidemia (yes/no): Treatment:
Hyperuricemia (yes/no): Treatment:
Cardiological history (yes/no): Type and treatment:
Previous neoplasms (date of diagnosis and disease-free time):
Previous thoracic surgery (yes/no): describe the type of intervention and effects on CT.
Please cite this article as: Román A, et al. Normativa para la selección de pacientes candidatos a trasplante pulmonar. Arch Bronconeumol. 2011;47:303-9.