The association of gender with health status (HS) response to long-term oxygen therapy (LTOT) in very severe COPD is unclear. The aims of this study were: (1) to compare dyspnea perception and HS between male and female with very severe COPD at baseline and (2) to provide a prospective assessment of HS response to LTOT, according to gender.
Patients and methodsHypoxemic COPD (n=97, age: 65.5±9.6 years, 53% males) were enrolled in a prospective longitudinal study over 12 months or until death. St. George's Respiratory Questionnaire (SGRQ) and baseline dyspnea index (BDI) were assessed.
ResultsAt baseline, HS impairment and dyspnea sensation were similar between genders. After 12 months of LTOT, women presented improvement in symptom (64.1±20.6 versus 40.6±22.9; P<.0001) and total SGRQ scores. Men also showed improvement in symptoms after 12 months (62.7±23.3 versus 49.6±22.8; P<.0005); however, they presented deterioration of activity, impact, and total scores during the study period, with markedly decline of activity domain (68.5±20.0 versus 75.9±16.9; P=.008). BDI did not show significant difference by gender over the study period.
ConclusionsOur results show that the HS course in very severe COPD patients differs according to gender, as females show greater response longitudinally to LTOT.
En la enfermedad pulmonar obstructiva crónica (EPOC) muy grave no está clara la asociación del sexo con el estado de salud (ES) en respuesta a la oxigenoterapia crónica domiciliaria (OCD). Los objetivos del presente estudio fueron: 1) comparar la percepción de la disnea y del ES entre hombres y mujeres con EPOC muy grave en el período basal, y 2) proporcionar una evaluación prospectiva de la respuesta del estado de salud a la OCD, de acuerdo con el sexo.
Pacientes y métodosEn un estudio longitudinal, prospectivo, se incluyeron pacientes con EPOC hipoxémica (n=97, edad: 65,5±9,6 años, 53% de hombres) durante 12 meses o hasta su muerte. Se evaluaron con el Cuestionario Respiratorio de St George (St. George's Respiratory Questionnaire [SGRQ]) y el índice de disnea basal (IDB).
ResultadosEn el período basal, el deterioro del ES y la sensación de disnea fueron similares entre ambos sexos. Después de 12 meses de OCD, en mujeres se detectó una mejoría de los síntomas (64,1±20,6 frente a 40,6±22,9; p<0,0001) y de las puntuaciones totales obtenidas en el SGRQ. En hombres también se demostró una mejoría de los síntomas después de 12 meses (62,7±23,3 frente a 49,6±22,8; p<0,0005); sin embargo, presentaron un deterioro de las puntuaciones de la esfera de actividad, impacto y totales durante el período de estudio, con un declive destacado en la esfera de actividad (68,5±20,0 frente a 75,9±16,9; p=0,008). Para el IDB no se demostraron diferencias significativas por sexos durante el período del estudio.
ConclusionesLos resultados del presente estudio demuestran que, en pacientes con EPOC muy grave, el curso del estado de salud difiere de acuerdo con el sexo, puesto que en las mujeres se demuestra una mayor respuesta longitudinal a la OCD.
Women represent a rapidly growing proportion of patients with chronic obstructive pulmonary disease (COPD), as can be deduced from the increasing prevalence of female tobacco use as well as the possible greater influence of cigarette smoke on those of the female gender.1,2 Women with COPD are younger,3–5 smoke less,3–5 respond at a lesser degree to lung rehabilitation treatment,6 manifest greater reactivity of the airways2 and report more dyspnea than men for the same degree of airflow obstruction.7
Health status (HS) is an important evaluation criterion in patients with COPD and its deterioration is considerable, corresponding with the severity of the disease.8–10 Among the medical studies published, there are hardly any data that suggest women being more vulnerable to the negative effects of COPD on state of health.5,11 Nevertheless, these studies included few patients with very severe COPD who were being treated with long-term oxygen therapy (LTOT). In addition, we have not found prospective studies comparing the changes in health status between men and women with COPD after said treatment.
We hypothesize that very severe COPD patients may present different responses to LTOT, depending on their gender. Therefore, this present study was designed: 1) to report the differences between men and women with very severe COPD, regarding degree of dyspnea and specific HS of the disease and 2) to provide a prospective evaluation of the response of the health status to LTOT, according to gender.
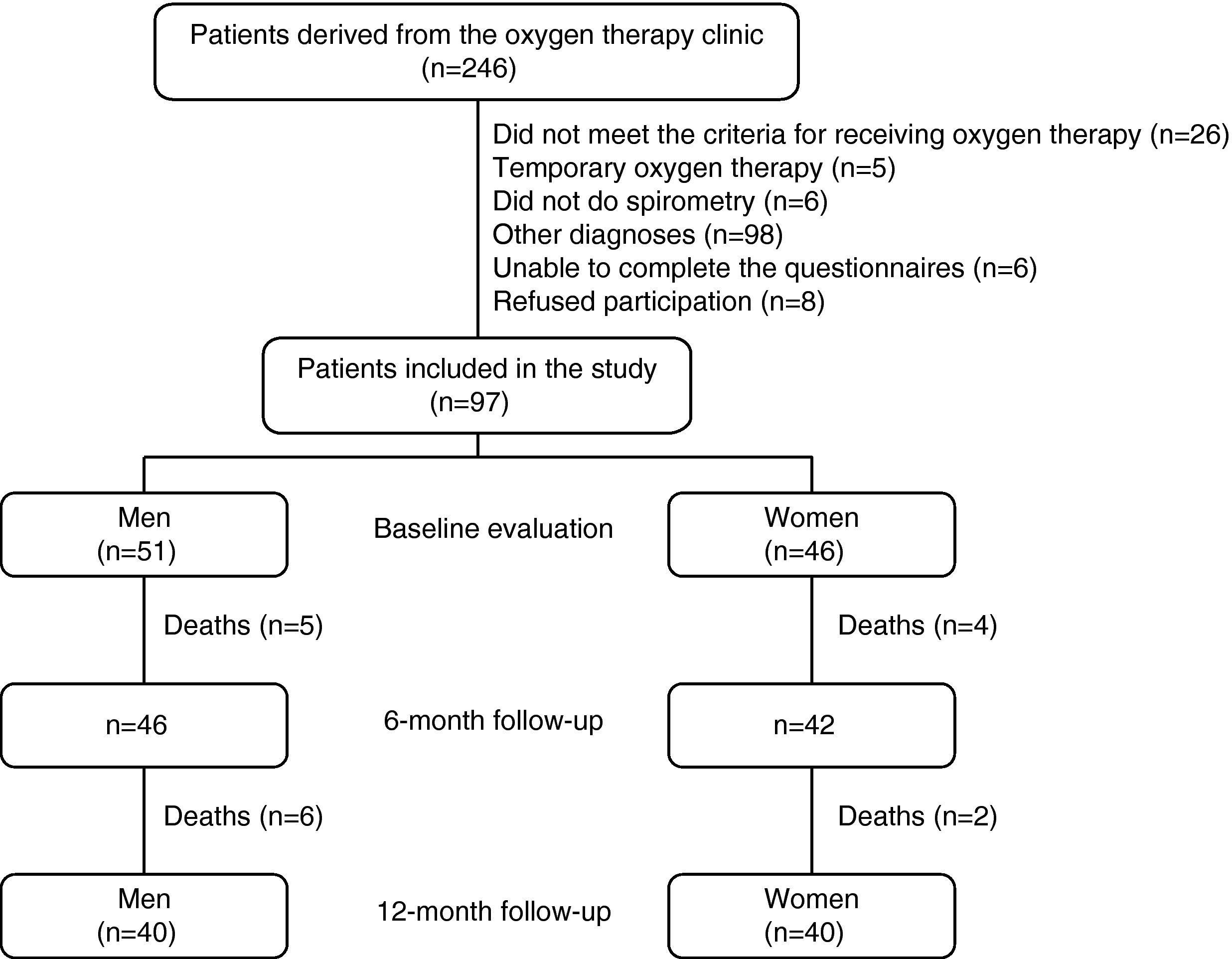
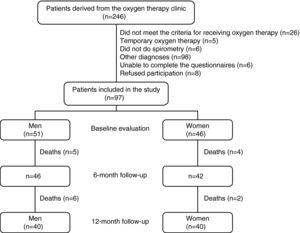
Patients and MethodsWe carried out a prospective, observational study of COPD patients, recruited from the LTOT program from a third-level university hospital (Botucatu Medical School, UNESP-São Paulo State University, Brazil). All the patients met the criteria established by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) and by the Brazilian Thoracic Society (BTS) for the diagnosis of COPD (post-bronchodilator FEV1/FVC ratio <0.70) and for LTOT.12,13 The additional inclusion criteria were the following: 1) stable disease, from a clinical standpoint (with no changes in dosage of the medication or administration intervals and with no exacerbations of the disease or hospitalizations in the 6 weeks prior to evaluation) and 2) patients with persistent hypoxemia after three months of oxygen therapy (to avoid the inclusion of those who received temporary oxygen supplements). The exclusion criteria were patients with concomitant respiratory diseases, such as: associated restrictive disease, sleep apnea/hypopnea syndrome, asthma, bronchiectasis and those incapable of either understanding or completing the health status questionnaire. Fig. 1 describes the study design.
All the patients were seen in the oxygen therapy clinic every three months in order to evaluate the compliance with LTOT, determine the incidence of exacerbations/hospitalizations and adjust the oxygen flow, if necessary. During the study period, the patients received the treatment recommended for COPD and were treated appropriately for the exacerbations.12 For those subjects who missed a follow-up visit, the data for the survival state of the patient were obtained by means of a telephone call to the family, and a new appointment was scheduled, when appropriate.
The study was approved by the research committee of the Botucatu Medical School University Hospital and all the patients gave their written informed consent.
Evaluation ProceduresFor each patient, we evaluated the smoking history (pack-years), body weight and stature, and calculated the body mass index (BMI=kg/m2). The comorbidities were quantified with the Charlson comorbidity index.14 Spirometry (Med-Graph 1070 spirometer; Medical Graphics Corporation; St. Paul, MN, USA) was done prior to and 15min after the inhalation of 400μg of salbutamol, in accordance with the criteria established by the American Thoracic Society.15 We determined the values for forced expiratory volume in one second (FEV1) and forced vital capacity (FVC) and these were expressed in liters and as percentages of the reference values.16 PaO2 and PaCO2 (Stat Profile 5 Plus; Nova Biomedical; Waltham, MA, USA) were determined, as well as pulse-oximetry (SpO2), using a portable oximeter (Model 9500 Oximeter; Nonin Medical Inc.; Minneapolis, MN, USA) while the patient was at rest breathing room air.
In order to evaluate the health status of the patients at baseline and after 6 and 12 months of follow-up, a translated version of St. George's Respiratory Questionnaire (SGRQ) was used, which had been validated for use in Brazil.17 Scored from 0 (best score) to 100 (worst score), a change of 4 units was considered clinically significant.18 The severity of the dyspnea was evaluated by means of the modified Brazilian version of the baseline dyspnea index (BDI), formulated by Mahler et al.19,20 The BDI is made up of three subscales that are used to evaluate the severity of the disease: 1) magnitude of the effort necessary to produce dyspnea; 2) magnitude of the task necessary to produce dyspnea; and 3) degree of functional deterioration due to the dyspnea. The score obtained from each subscale is added, which provides a total score that varies from 0 to 12, the highest values representing a lower perception of dyspnea.20
Oxygen TherapyOxygen therapy was prescribed for a minimum of 18h/day, using nasal cannula. The flow rate necessary for obtaining SpO2 ≥90% was determined in the oxygen therapy clinic and was readjusted every three months. The oxygen was distributed by an oxygen concentrator in 84.4% of patients and by large tanks (size K or H) in 15.5%. The personnel of the oxygen therapy clinic instructed the patients and their families in the use of the oxygen distribution system. The supplier provided the patient with the material and home technical services. The LTOT compliance data were evaluated by means of self-evaluation obtained from the patients and their care-takers, and the researcher classified them depending on whether the reported use complied with the prescription. No ambulatory oxygen therapy was provided.
Statistical AnalysisEach variable is reported as means±SD or median (25th to 75th percentiles), depending on its distribution. The comparisons of the baseline characteristics between sexes were done using the Student's t-test for variables with an approximately normal distribution, and the Mann–Whitney U test was used for variables without normal distribution. In order to investigate the changes in the 6- and 12-month follow-ups, repeated measure analysis of variance (2×2: gender×time) was used. We also evaluated the proportion of patients that presented a minimal clinically important difference (MCID) for scoring each sphere and for the total score obtained in the SGRQ18 at the following visits: 0–6, 6–12, and 0–12 months. The patients were stratified into three categories in accordance with the MCID for the SGRQ: better (decrease≥4 units), worse (increase≥4 units) or no change. The associations between gender and MCID were evaluated by means of the χ2 test. The level of significance of all the analyses was established at 5%. All the data were analyzed and processed by means of the Proc GENMOD program by SAS 9.1.3 (SAS Institute Inc., Cary, NC, USA).
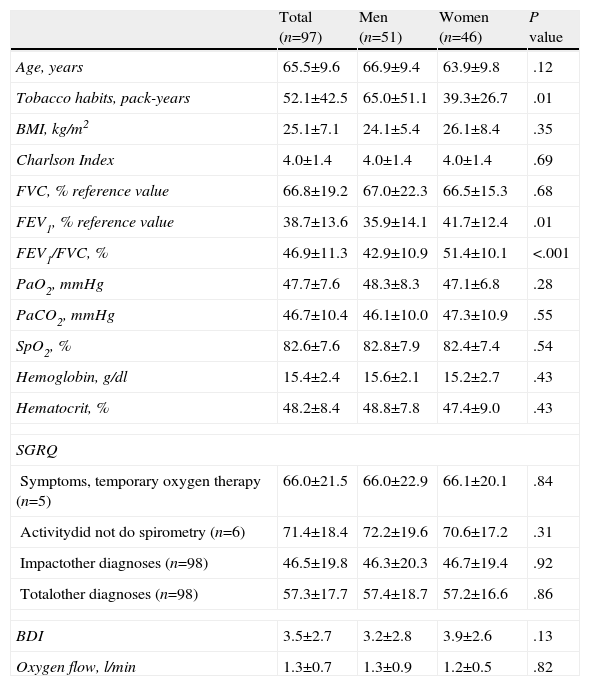
ResultsBaseline CharacteristicsOut of a total of 246 patients with respiratory insufficiency derived from the oxygen therapy clinic between October 2003 and August 2007, included for study were 97 COPD patients (51 men and 46 women) (Fig. 1). Table 1 shows the baseline characteristics of the 97 patients with COPD. The pharmacological treatment included inhaled β2 agonists (60.8%), inhaled ipratropium bromide (54.6%), inhaled corticosteroids (16.5%), diuretics (39.2%), xanthine (4.1%), and oral corticosteroids (9.3%), with no observed differences between men and women. Despite similar age, the women referred less tobacco use, obtained greater FEV1 values as percentage of the reference value and a greater FEV1/FVC ratio than the men. However, the FEV1 response to the bronchodilator was not different between groups. In both groups, no significant differences were identified concerning BMI, Charlson comorbidity index, gas exchange, hemogram, health status or sensation of dyspnea at the time of inclusion (Table 1).
Baseline Characteristics of the COPD Patients Who Received Long-Term Oxygen Therapy.
| Total (n=97) | Men (n=51) | Women (n=46) | P value | |
| Age, years | 65.5±9.6 | 66.9±9.4 | 63.9±9.8 | .12 |
| Tobacco habits, pack-years | 52.1±42.5 | 65.0±51.1 | 39.3±26.7 | .01 |
| BMI, kg/m2 | 25.1±7.1 | 24.1±5.4 | 26.1±8.4 | .35 |
| Charlson Index | 4.0±1.4 | 4.0±1.4 | 4.0±1.4 | .69 |
| FVC, % reference value | 66.8±19.2 | 67.0±22.3 | 66.5±15.3 | .68 |
| FEV1, % reference value | 38.7±13.6 | 35.9±14.1 | 41.7±12.4 | .01 |
| FEV1/FVC, % | 46.9±11.3 | 42.9±10.9 | 51.4±10.1 | <.001 |
| PaO2, mmHg | 47.7±7.6 | 48.3±8.3 | 47.1±6.8 | .28 |
| PaCO2, mmHg | 46.7±10.4 | 46.1±10.0 | 47.3±10.9 | .55 |
| SpO2, % | 82.6±7.6 | 82.8±7.9 | 82.4±7.4 | .54 |
| Hemoglobin, g/dl | 15.4±2.4 | 15.6±2.1 | 15.2±2.7 | .43 |
| Hematocrit, % | 48.2±8.4 | 48.8±7.8 | 47.4±9.0 | .43 |
| SGRQ | ||||
| Symptoms, temporary oxygen therapy (n=5) | 66.0±21.5 | 66.0±22.9 | 66.1±20.1 | .84 |
| Activitydid not do spirometry (n=6) | 71.4±18.4 | 72.2±19.6 | 70.6±17.2 | .31 |
| Impactother diagnoses (n=98) | 46.5±19.8 | 46.3±20.3 | 46.7±19.4 | .92 |
| Totalother diagnoses (n=98) | 57.3±17.7 | 57.4±18.7 | 57.2±16.6 | .86 |
| BDI | 3.5±2.7 | 3.2±2.8 | 3.9±2.6 | .13 |
| Oxygen flow, l/min | 1.3±0.7 | 1.3±0.9 | 1.2±0.5 | .82 |
The data are presented as means±SD. The statistical tests used were the Student's t test for independent data or the Mann–Whitney U test.
FEV1, forced expiratory volume in one second; FVC, forced vital capacity; BDI, Baseline Dyspnea Index; BMI, Body Mass Index; PaCO2, arterial carbon dioxide pressure; PaO2, arterial oxygen pressure; SGRQ, St. George's Respiratory Questionnaire; SpO2, pulse-oximetry.
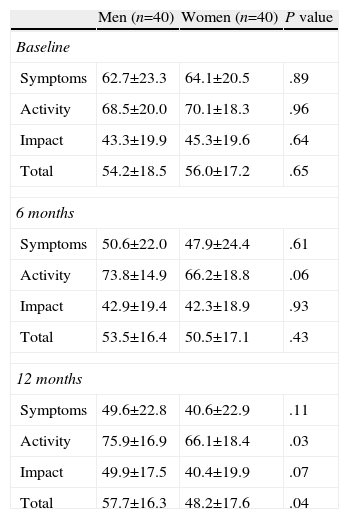
In the statistical analysis of the changes detected during follow-up, 80 patients (40 men and 40 women) who had survived 12 months were included. The global analysis demonstrated a significant improvement in the total score obtained on the SGRQ after 6 months of treatment with LTOT (P=.03) and in the symptoms domain at the 6-month follow-up (P<.001), which continued at 12 months (P<.001).
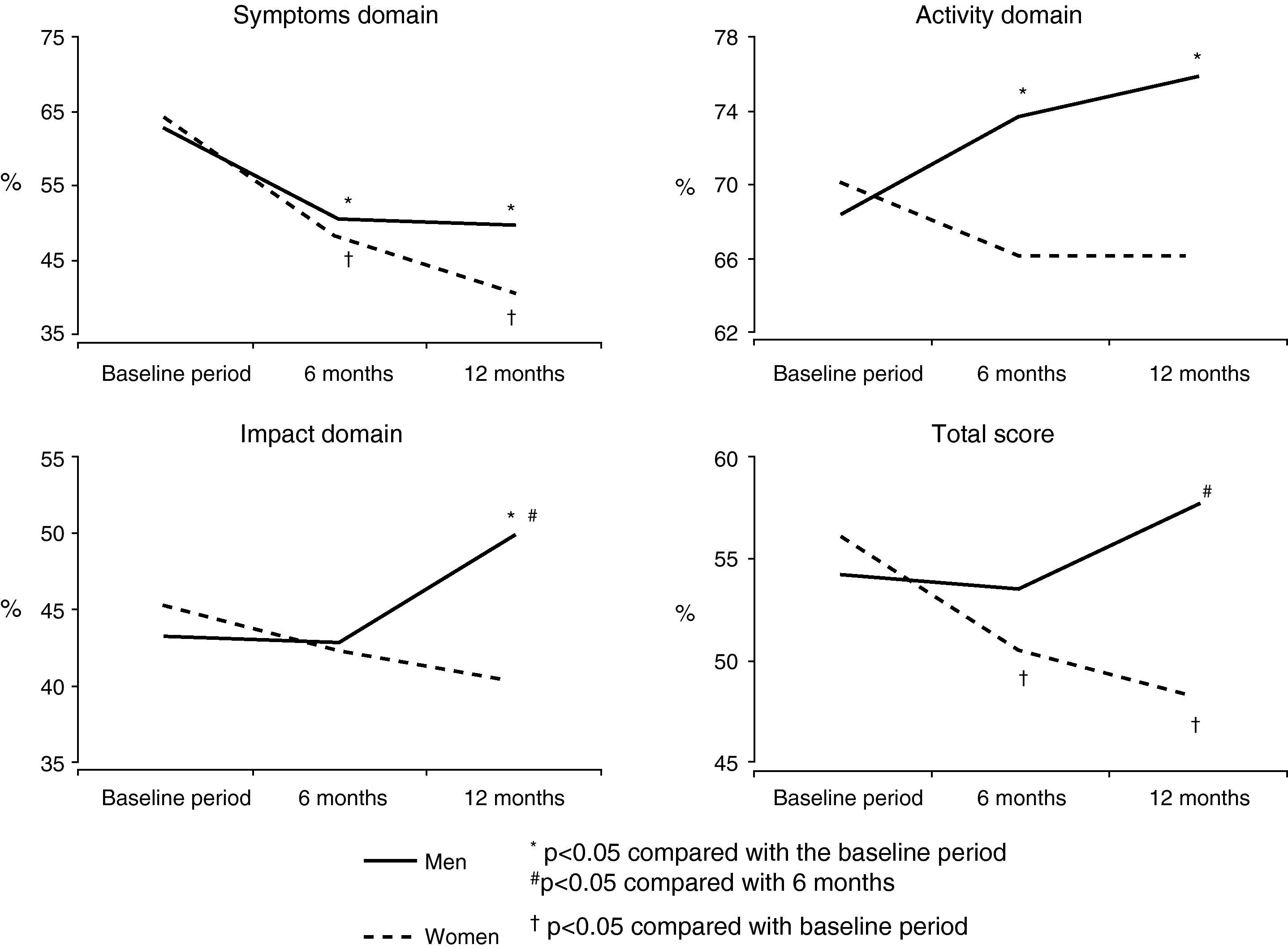
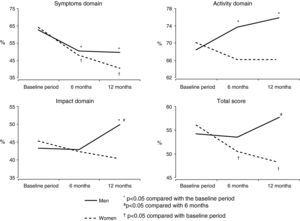
We found an interaction of gender with time that was statistically significant for the scores of activity, impact, and total scores obtained on the SGRQ. For the women, the total score showed a significant improvement after 6 months (P=.0008) that continued at the 12-month follow-up (P=.0004). The scores in the activity (P=.08) and impact (P=.009) domains on the SGRQ were stable during the 12-month period (Fig. 2).
In comparison with the women, during the first 6 months the men presented a stable total SGRQ score (P=.78) but a significantly poorer score in the last 6 months of the study (P=.03). Moreover, the activity score was significantly poorer in men after 6 months (P=.05), which continued at the 12-month follow-up (P=.008), and the impact score significantly worsened during the last 6 months of the study (P=.003) (Fig. 2).
The comparison between men and women demonstrated similar results for all the domains of the questionnaire in the baseline period and at 6 months; however, after 12 months the men presented a poorer score for activity (P=.03) and total score on the questionnaire (P=.04) than women (Table 2).
Comparison Between Men and Women for Each Domain of the SGRQ in the Different Study Periods.
| Men (n=40) | Women (n=40) | P value | |
| Baseline | |||
| Symptoms | 62.7±23.3 | 64.1±20.5 | .89 |
| Activity | 68.5±20.0 | 70.1±18.3 | .96 |
| Impact | 43.3±19.9 | 45.3±19.6 | .64 |
| Total | 54.2±18.5 | 56.0±17.2 | .65 |
| 6 months | |||
| Symptoms | 50.6±22.0 | 47.9±24.4 | .61 |
| Activity | 73.8±14.9 | 66.2±18.8 | .06 |
| Impact | 42.9±19.4 | 42.3±18.9 | .93 |
| Total | 53.5±16.4 | 50.5±17.1 | .43 |
| 12 months | |||
| Symptoms | 49.6±22.8 | 40.6±22.9 | .11 |
| Activity | 75.9±16.9 | 66.1±18.4 | .03 |
| Impact | 49.9±17.5 | 40.4±19.9 | .07 |
| Total | 57.7±16.3 | 48.2±17.6 | .04 |
The data are presented as means±SD.
During the 12-month follow-up period, the severity of dyspnea, calculated by the sum of the three subscales of the BDI, did not change for women (baseline: 4.2±2.6 and 12-month: 4.7±2.5; P=.29) or for men (baseline: 3.7±2.8 and 12-month: 3.4±2.6; P=.47).
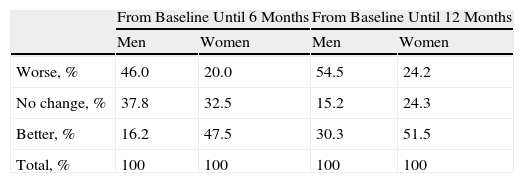
Minimal Clinically Significant DifferenceAn association was found between gender and MCID for the activity score and the total score of the questionnaire. After 6 months, 47.5% of women obtained an improvement, reaching 51.5% after 12 months. In comparison for the same domain, after 6 months 46.6% of men obtained clinically significant poorer scores, which reached 54.5% after 12 months (Table 3).
Percentage of Patients With COPD in the Categories With a Clinically Significant Difference in the Activity Domain of the SGRQ During Oxygen Therapy, According to Gender.
| From Baseline Until 6 Months | From Baseline Until 12 Months | |||
| Men | Women | Men | Women | |
| Worse, % | 46.0 | 20.0 | 54.5 | 24.2 |
| No change, % | 37.8 | 32.5 | 15.2 | 24.3 |
| Better, % | 16.2 | 47.5 | 30.3 | 51.5 |
| Total, % | 100 | 100 | 100 | 100 |
For the total score obtained on the questionnaire, the association between sex and MCID observed after only 12 months of follow-up revealed a clinically-pertinent improvement in 30.3% of men and 66.7% of women (P=.01).
Oxygen UseThe median rate of oxygen flow used was 1.0L/min. The oxygen flow prescribed was 0.5L/min in 18.6% of patients, 1.0L/min in 49.5% of patients, 1.5L/min in 14.4%, 2.0L/min in 9.3% and ≥2.5L/min in 8.2%, with no differences detected between men and women. According to what was previously defined, the overall compliance with the treatment was 60% after 6 months (women: 63%, men: 58%; P=0.96) and 61% after 12 months (women: 63%, men: 59%; P=0.98).
DiscussionThis present study clearly demonstrates a benefit of oxygen therapy on health status in hypoxemic patients with chronic obstructive pulmonary disease. The analysis of the 80 patients who completed the study demonstrated a significant improvement in the total score obtained in the SGRQ after 6 months and a significant improvement in the symptom domain after 6 months, which continued 12 months later. In the baseline period, both genders presented a similar deterioration in the state of health. However, in the analyses stratified by gender, longitudinal differences were demonstrated between men and women. In women, a persistent improvement was observed in the symptom score and total score and, in comparison, in the men there were observed significantly poorer activity and impact scores as well as total score on the questionnaire during treatment with LTOT.
During the baseline period, we identified differences between sexes in the history of tobacco use and airflow obstruction in patients who received oxygen therapy. This is a new finding and we interpreted this observation as an indication that women with COPD develop hypoxemia with a lower degree of airflow obstruction and a significantly shorter history of smoking than men. The results of this present study also support the concept that women could be more vulnerable to the harmful effects of inhaled smoke. In previous studies, designed to compare the clinical differences between genders among patients with stable COPD, the women were younger and smoked less than the men when paired by FEV1 values as a percentage of the reference values.4,5
The interest in evaluating health status has increased in recent years, as has the interest in the influence of gender in the expression of COPD. In patients with very severe disease, we have shown a substantial deterioration in state of health. This finding coincides with the results of previous studies demonstrating that health status deterioration runs parallel to disease severity.8–11 In fact, in previous studies carried out in patients with COPD with a wide variety of airflow obstruction, a greater deterioration in quality of life was reported related with health in women.4,5,7,8,11 However, when patients were classified by the severity of the obstruction (depending on the FEV1% values), there were no differences in the health status for the group of patients with more severe disease.4,8 The baseline characteristics of the patients of the present study support these findings, suggesting that those with very severe COPD present a deterioration of such a degree in their health status when they receive LTOT that it is possible that no differences are observed between sexes.
One exclusive finding of this prospective, longitudinal, interventionist study was the difference between genders in the response to oxygen therapy in COPD patients. The findings demonstrate that the women manifested significant improvements in the symptom score and total score obtained in the questionnaire during the study period; on the other hand, the activity and impact domains did not change. Nevertheless, despite a significant improvement of the symptoms, the men presented a notably poorer score in the activity domain, impact, and total score obtained in the questionnaire at the 12-month follow-up. As far as the authors are aware, only one previous longitudinal study has been published that demonstrates differences between genders after the start of oxygen therapy.21 The study evaluated patients with chronic airflow limitation in the baseline period and after initiating oxygen therapy at 3, 6, and 12 months, using both generic and specific disease questionnaires. The results obtained with the disease-specific Chronic Respiratory Questionnaire (CRQ) showed that the women obtained a significant improvement in all the domains, while the men obtained an improvement in the CRQ fatigue domain.21 The data of this present study back these findings in COPD patients, suggesting an improvement in the quality of life during oxygen therapy in women, although with a less-convincing response than in men.
Very few longitudinal studies have examined the effect of oxygen therapy on the health status of COPD patients without an analysis stratified by gender,22,23 and the results are controversial. The findings of the present study coincide with those by Eaton et al.23 who, in patients with severe COPD that met the inclusion criteria after the introduction of oxygen therapy, demonstrated a significant improvement in the health-related quality of life with a maintained or additional response at 6 months. In comparison, using the SGRQ questionnaire during a period of 6 months, Okubadejo et al.22 did not demonstrate a change in health status; nevertheless, it was a small-scale study and consequently might not have had sufficient power.
The activity domain includes the physical activities that either induce dyspnea or are limited by it. The results of the present study demonstrate that the limitation of activity, as evaluated by the activity subscale of the SGRQ, was the health status variable that notably deteriorated in men. Compared with women of the same age group, men usually perform a greater physical effort and, in contrast with this, it is predictable that the patients receiving oxygen therapy spend more time at home and reduce their general level of exercise. For this reason, it would in part explain the differences in the activity domain of the questionnaire observed between sexes during follow-up.
Dyspnea is one of the main determinants of health status in COPD patients. A previous study found a powerful correlation between the degree of dyspnea and health status on each of the subscales (symptoms, activities, and impact) obtained from the SGRQ in an extensive series of patients with COPD.24 In a later study, it was demonstrated that in patients with more severe obstruction, baseline dyspnea offered the best explanation of the general state of health and also of the activity domain and symptoms.25 Furthermore, the sensation of dyspnea is a valid indicator of survival in the first year among patients with very severe COPD treated with oxygen therapy.26 However, the index of baseline dyspnea did not change during the study period for men and women in this present research. One possible explanation of this result is that LTOT does not improve the sensation of dyspnea.9,27 Similarly, in a previous study it was observed that the dyspnea scores (Borg scale and oxygen-cost diagram) did not change after 12 months of oxygen therapy.28 In the NOTT and MRC studies, the effects of oxygen therapy on survival seemed to depend on the daily duration of the treatment, observing the better outcome among those individuals who received oxygen therapy during a greater number of hours per day.29,30
We strongly recommended the patients of the present study to use the oxygen in compliance with the prescription, and this advice was reinforced upon each visit to the clinic. In this study, the overall compliance with the treatment was 61%, and other researchers have reported similar findings.23,28 In general, the compliance with oxygen therapy was far from ideal as the percentage of patients who used oxygen for more than 15h per day varied from 37% to 65%.23,28,31 It is worrying that the underuse of oxygen therapy limits its effectiveness, but we observed a similar compliance in patients of both genders (63% compared to 59%; P=.98); therefore, the reported differences for gender regarding health status in this present study cannot be explained by the lack of treatment compliance.
When interpreting the results of the present study, some potential limitations should be considered. In the first place, the compliance with oxygen therapy was evaluated by what was reported by each patient. Nevertheless, the methods generally used for quantifying the number of hours that the patients use oxygen, such as the number of empty oxygen tanks and the readings of the mean oxygen flow received by the patient through a self-controlled device, are also prone to error. Second of all, although the smokers were not candidates for oxygen therapy, tobacco use was not confirmed with laboratory tests. Last of all, we did not analyze other variables that may influence the health status, such as psychosocial factors, socio-economic position and marital status as well as the years studied.
The present study takes on for the first time the course of the state of health in men and women with very severe COPD, treated with oxygen therapy. In the baseline period, the patients referred deterioration similar to the health status and a similar sensation of dyspnea. After treatment, in both sexes the symptom domain of the SGRQ improved. However, after 12 months of the study, in men there were significantly worse scores for the activity domain, impact and total score, at the same time there was a clinically significant poorer activity and impact in the same period. These results demonstrate that, in patients with very severe COPD, health status differs according to gender as women show a greater longitudinal response to oxygen therapy.
Conflict of InterestsThe authors declare having no conflict of interests.
Please cite this article as: Coleta KD, et al. Asociación del sexo con el estado de salud en respuesta a la oxigenoterapia crónica domiciliaria en pacientes con enfermedad pulmonar obstructiva crónica. Arch Bronconeumol. 2011;47:382–8.