Gastric perforation is a rare complication of bronchoscopy, and in recent decades, some cases associated with the administration of oxygen therapy by nasopharyngeal tube have been published.
We report the case of a 72-year-old woman with a history of uterine cancer in 2004, in complete remission until 2011, when she attended a follow-up visit in which a chest X-ray was performed that showed a nodule in the right lower lobe. The finding was confirmed by chest computed tomography (CT), which revealed a 35mm mass in the apical segment of the right lower lobe. Malignancy was suspected. For pathological confirmation, a fiberoptic bronchoscopy was performed under conscious sedation (intravenous midazolam 4mg and fentanyl 0.5mg), and samples were collected with bronchoalveolar lavage and blind brushing, in a procedure that took less than 30min.
During this procedure, oxygen therapy was administered with a nasopharyngeal tube at a flow rate of 2lpm according to protocol: the nose–ear distance was measured and this length of tube was introduced into the free nostril.
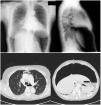
After completing the procedure, the patient presented significant abdominal distention with diffuse pain on palpation, but remained hemodynamically stable. Due to the increase in abdominal pain, a nasogastric tube was placed, with no improvement, so she was referred to the emergency room, where additional tests revealed leukocytosis (16900leukocytes/mcg) with neutrophilia (93%). Chest X-ray showed significant pneumoperitoneum (Fig. 1). A CT of the chest and abdomen was performed, which also showed the presence of pneumomediastinum and partial pneumothorax in the anterior right lung base (Fig. 1). In view of the previous bronchial manipulation, the fiberoptic bronchoscopy was repeated, ruling out bronchial perforation within the limits of the endoscopic vision.
An emergency exploratory laparotomy was performed, showing a 3mm perforation of the lesser gastric curvature. This was sutured in 2 planes with separate resorbable 3–0 sutures. The patient's subsequent progress was good, and she was discharged 12 days later. The patient recovered completely from the event, and has had no complications is the subsequent follow-up period of over 2 years.
The lung lesion was classified with intraoperative examination of the biopsy as pulmonary adenocarcinoma (T2N0M0), so right lower lobectomy was performed without incident. The patient is currently attending follow-up visits, and continues in excellent general condition with no signs of relapse after 5 years.
Flexible fiberoptic bronchoscopy is a safe diagnostic and therapeutic technique (mortality <0.1%).1,2 Complications are rare and depend on the patient's comorbidities, factors associated with anesthesia and procedures, and duration of the intervention. These include, most notably, bleeding, hypoxemia, bronchospasm, pneumothorax, and the appearance of arrhythmias.3 Gastric perforation associated with this technique is an extraordinary complication.
The administration of oxygen therapy via a nasopharyngeal tube during bronchoscopy has been associated with gastric perforation in some publications.4 Migration of the tube to the esophagus is an obvious cause of abdominal distension which might contribute to perforation.5 However, this complication has also been described in cases in which the nasopharyngeal tube was correctly positioned, even with low oxygen flows.4,6–11 Some authors have pointed out that, while the esophageal sphincter under normal conditions requires more than 15–25mmHg pressure to insufflate gas into the stomach,12 the use of muscle relaxants in anesthesia, along with the increased negative pressure that occurs in the esophagus during inspiration and other individual variables may cause this phenomenon.13 Since the lesser curvature of the stomach contains fewer gastric folds, this region is the least elastic and the one most prone to perforation.14 This, however, is unlikely to have occurred in our patient, who only received low doses of midazolam during the procedure.
In our hospital, only 1 case of gastric perforation related with this technique has been recorded. However, it should be suspected in any patient who presents abdominal distension, particularly after the administration of oxygen therapy, the use of mechanical ventilation, or endoscopic manipulation. When gastric perforation occurs, the air and the stomach contents pass into the peritoneal cavity, causing abdominal distension, bloating, and rigidity. In some cases, subcutaneous emphysema and pneumomediastinum may occur. If not treated promptly, signs of shock and hemodynamic instability can develop rapidly.
Standard X-rays of the chest and abdomen may be useful for visualizing the pneumoperitoneum, but abdominal CT will reveal less obvious cases and help assess the existence, severity, and extension of associated pneumomediastinum or pneumothorax. On occasions, it is also useful for evaluating the site of the perforation, but in many cases, surgical techniques are required to locate the lesion.
Treatment of choice for gastric rupture is urgent surgery. Mortality caused by peritonitis due to perforation increases rapidly if repair is delayed. In addition to surgical treatment, antibiotic coverage against the habitual Gram negative gut flora must be given.
Given the speed with which this entity can evolve, observation is required to monitor for signs of hemodynamic instability, and on occasions, vasoactive agents are required to stabilize the patient.
This complication, though extremely rare during bronchoscopy, is a life-threatening emergency that should be suspected in the presence of abdominal distension after the procedure, and its association with the administration of oxygen therapy via a nasopharyngeal tube should be borne in mind. Use in elderly women should be avoided.7 Correct measurement and placement of the nasopharyngeal tube, and correction of the position of the tube with bronchoscopic vision as it is advanced, wherever possible, should further decrease the incidence of this rare complication. Moreover, other alternatives not associated with this event, such as facial masks that provide greater FiO2 than nasal or nasopharyngeal tubes, are available.
Please cite this article as: Giménez Velando A, Rodriguez Nieto MJ, Flandes Aldeyturriaga J. Perforación gástrica durante la broncoscopia al administrar oxigenoterapia por cánula nasofaríngea. Arch Bronconeumol. 2018;54:293–294.