Lung transplantation (LT) is a therapeutic option with controversial results in chronic obstructive pulmonary disease (COPD). We aimed to analyze the outcomes of transplantation in terms of lung function and to identify prognostic factors.
MethodA retrospective analysis of 107 patients with COPD receiving lung transplants in the La Fe Hospital between 1991 and 2008 was performed. Preoperative variables, functional examinations pre and post-LT, surgical procedure variables and long-term monitoring, expressed as mean or percentage, as applicable, were analyzed. Spirometric results before and after LT were analyzed. Linear or logistic regression was used for multivariate analysis depending on the variable.
ResultsNinety-four men (87.9%) and 13 women (12.1%) were transplanted, with a mean age±standard deviation of 52.58±8.05 years; 71% of LTs were double-lung transplantations. Spirometric values improved after LT: FVC: +1.22L (+34.9%), FEV1: +1.66L (+56.7%) and FEF25–75: +1.85L (+50.8%); P=.001. This functional improvement was maintained after 5 years only in the group with BODE score >7 (P=.001). Recipient height, type of LT, use of extracorporeal circulation during the surgical procedure, presence of bronchiolitis obliterans syndrome and the age and cause of death of the donor significantly influenced lung function over time.
ConclusionsLT improves lung function in COPD patients. This improvement was maintained at 5years only in patients with BODE>7. Double lung transplantation provides better functional results than single-lung transplantation.
El trasplante pulmonar (TP) es una opción terapéutica con resultados controvertidos en la enfermedad pulmonar obstructiva crónica (EPOC). Nuestro objetivo es analizar los resultados del trasplante en términos de función pulmonar, así como identificar los factores pronósticos.
MétodoSe realizó un análisis retrospectivo de 107 pacientes con EPOC trasplantados en el Hospital Universitario La Fe entre 1991 y 2008. Se analizaron variables preoperatorias, estudio funcional pre y post-TP, variables del procedimiento quirúrgico y del seguimiento a largo plazo, expresadas en media o porcentaje según el caso, comparándose los resultados espirométricos antes y después del TP. Para el análisis multivariante se utilizó regresión lineal o logística según la variable.
ResultadosFueron trasplantados 94 hombres (87,9%) y 13 mujeres (12,1%), con una edad media±desviación estándar de 52,58±8,05años; el 71% de TP fueron bipulmonares. Los valores espirométricos mejoraron tras el TP: FVC: +1,22l (+34,9%), FEV1: +1,66l (+56,7%) y FEF25–75: +1,85l (+50,8%); p=0,001, manteniéndose esta mejoría funcional tras 5años solo en el grupo con puntuación BODE>7 (p=0,001). La talla del receptor, el tipo de TP, la utilización de circulación extracorpórea durante el procedimiento quirúrgico, la presencia de síndrome de bronquiolitis obliterante junto con la edad y la causa de muerte del donante influyeron significativamente en la función pulmonar a largo plazo.
ConclusionesEl TP mejora la función pulmonar de los pacientes con EPOC. Esta mejoría se mantiene a los 5años solo en los pacientes con BODE mayor de 7. El trasplante bipulmonar proporciona mejores resultados funcionales que el unipulmonar.
Chronic obstructive pulmonary disease (COPD) is a health problem of the first magnitude, and is currently estimated to be the fourth cause of death worldwide. Incidence of COPD is on the rise, and in the near future it will take third place in the global mortality ranking.1,2
Despite constant advances and updates in the treatment of this disease,1,3–5 COPD is one of the few chronic diseases that has shown an increase in mortality in recent years.6
In the last few decades, lung transplantation (LT) has been a therapeutic alternative in patients with end-stage disease and with chronic respiratory failure,5,7 and this procedure has yielded 5-year survival rates of around 50% in highly selected patients.7,8
However, the use of this intervention in COPD remains controversial. Several authors have reported the efficacy of LT in terminal disease, both in terms of survival and quality of life,8–11 while other have questioned the usefulness of the procedure in this entity,4,12 since it yields the poorest outcomes in terms of long-term survival, matched only by pulmonary fibrosis.7,13
The latest report of the International Society for Heart and Lung Transplantation (ISHLT) (2013)7 analyzes the functional status of patients receiving LT according to the Karnofsky scale, and their reincorporation into the workplace. However, very few studies have analyzed the course of lung function in recipients, determined by spirometry, over the years following LT.8
The aim of this study was to analyze the evolution of lung function values in COPD patients undergoing LT, and to identify variables that may affect their outcome.
MethodThis was a retrospective analysis of 107 COPD patients undergoing lung transplantation in the Hospital Universitario La Fe, from the introduction of the transplantation program in 1991 up to December 31, 2008. Follow-up comprised the period between the performance of the procedure and the death of the patient, or for survivors, until the date of study closure on January 1, 2010.
The clinical diagnosis of COPD was made on the basis of current international guidelines3 or those in force at the time of diagnosis. All patients accepted for LT were included in the program on the basis of established international criteria.14
The following pre-operative variables were analyzed: age, sex, height, weight, body mass index (BMI), accumulated tobacco use expressed in pack-years, diagnosis (COPD or alpha-1-antitripsin deficit [A1ATD]), BODE index,15 full evaluation of respiratory function, including forced vital capacity (FVC), forced expiratory volume in 1s (FEV1) forced expiratory flows (FEF25–75), residual volume to total lung capacity ratio (RV/TLC), suggestive of pulmonary hypersufflation, and carbon monoxide diffusing capacity (DLCO), all of which were expressed in liters and percentage, and 6-min walking test in meters. Donor age and cause of death were recorded, together with intra-operative variables such as type of intervention, single-lung transplantation (SLT) or double-lung transplantation (DLT) and use of extracorporeal circulation (ECC).
The following variables were collected in each of the scheduled visits during the immediate perioperative phase and in the protocolized follow-up, 1, 3 and 6 months, and 1, 2 and 5 years post-LT, or until death: partial pressure of oxygen in arterial blood/fraction of inspired oxygen ratio (PaO2/FiO2), 6 and 48h after LT, BMI, and signs of bronchiolitis obliterans syndrome (BOS)16 suggestive of chronic graft rejection, and the above-mentioned lung function values.
Analysis and comparison of means for continuous quantitative variables were performed using the Student's t-test17 for independent or paired samples for related means. Analysis of variance (ANOVA) was used to compare the quantitative variables of several groups.
The chi-squared17 method was used for analysis and comparison of qualitative variables, or, if conditions for chi-squared validity were not met, Fisher's exact test was used.
The multivariate analysis was performed using the linear regression test for continuous quantitative variables and the logistics regression test for qualitative variables.
Statistical significance was set at P≤.05.
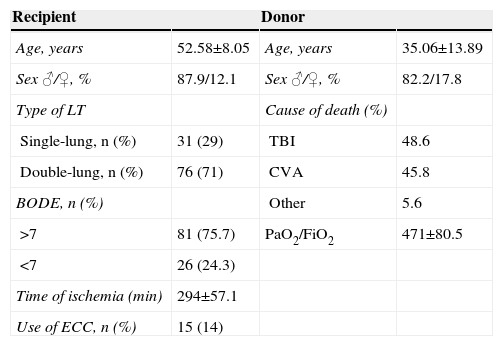
ResultsA total of 94 men (87.9%) and 13 women (12.1%) with a mean age±standard deviation of 52.58±8.05were transplanted. A total of 92 patients (86%) of patients had COPD, while 15 patients (14%) had a diagnosis of A1ATD. The most important characteristics of recipients and donors are described in Table 1.
Demographic Characteristics of Recipients and Donors.
| Recipient | Donor | ||
|---|---|---|---|
| Age, years | 52.58±8.05 | Age, years | 35.06±13.89 |
| Sex ♂/♀, % | 87.9/12.1 | Sex ♂/♀, % | 82.2/17.8 |
| Type of LT | Cause of death (%) | ||
| Single-lung, n (%) | 31 (29) | TBI | 48.6 |
| Double-lung, n (%) | 76 (71) | CVA | 45.8 |
| BODE, n (%) | Other | 5.6 | |
| >7 | 81 (75.7) | PaO2/FiO2 | 471±80.5 |
| <7 | 26 (24.3) | ||
| Time of ischemia (min) | 294±57.1 | ||
| Use of ECC, n (%) | 15 (14) |
CVA: cerebrovascular accident; ECC: extracorporeal circulation; PaO2/FiO2: partial pressure of oxygen in arterial blood/fraction of inspired oxygen ratio; LT: lung transplantation; TBI: traumatic brain injury.
The mean height of recipients was 1.66±0.72m, weight was 63.57±11.46kg, and BMI 22.84±3.22kg/m2.
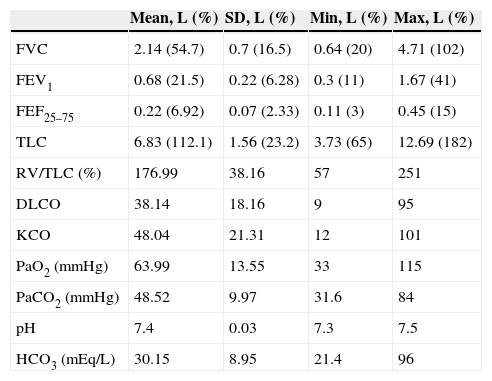
Results of lung function tests and pre-LT blood gases are given in Table 2.
Pre-Transplantation Lung Function Results.
| Mean, L (%) | SD, L (%) | Min, L (%) | Max, L (%) | |
|---|---|---|---|---|
| FVC | 2.14 (54.7) | 0.7 (16.5) | 0.64 (20) | 4.71 (102) |
| FEV1 | 0.68 (21.5) | 0.22 (6.28) | 0.3 (11) | 1.67 (41) |
| FEF25–75 | 0.22 (6.92) | 0.07 (2.33) | 0.11 (3) | 0.45 (15) |
| TLC | 6.83 (112.1) | 1.56 (23.2) | 3.73 (65) | 12.69 (182) |
| RV/TLC (%) | 176.99 | 38.16 | 57 | 251 |
| DLCO | 38.14 | 18.16 | 9 | 95 |
| KCO | 48.04 | 21.31 | 12 | 101 |
| PaO2 (mmHg) | 63.99 | 13.55 | 33 | 115 |
| PaCO2 (mmHg) | 48.52 | 9.97 | 31.6 | 84 |
| pH | 7.4 | 0.03 | 7.3 | 7.5 |
| HCO3 (mEq/L) | 30.15 | 8.95 | 21.4 | 96 |
DLCO: carbon monoxide diffusing capacity; FEF25–75: forced expiratory flow between 25% and 75% of vital capacity; FEV1: forced expiratory volume in 1s; FVC: forced vital capacity; KCO: DLCO adjusted for alveolar volume; mEq/L: milliequivalents/liter; L: liters; mmHg: millimeters of mercury; PaCO2: partial pressure of carbon dioxide in arterial blood; PaO2: partial pressure of oxygen in arterial blood/fraction of inspired oxygen ratio; TLC: total lung capacity; RV: residual volume.
Of the transplantations, 76 (71%) were double-lung. ECC was necessary in 14% of procedures, all of which were DLT. Mean donor age was 35.06±13.89 years and cause of death was traumatic brain injury in 48.6%, cerebrovascular accident in 45.8% and other causes in 5.6%.
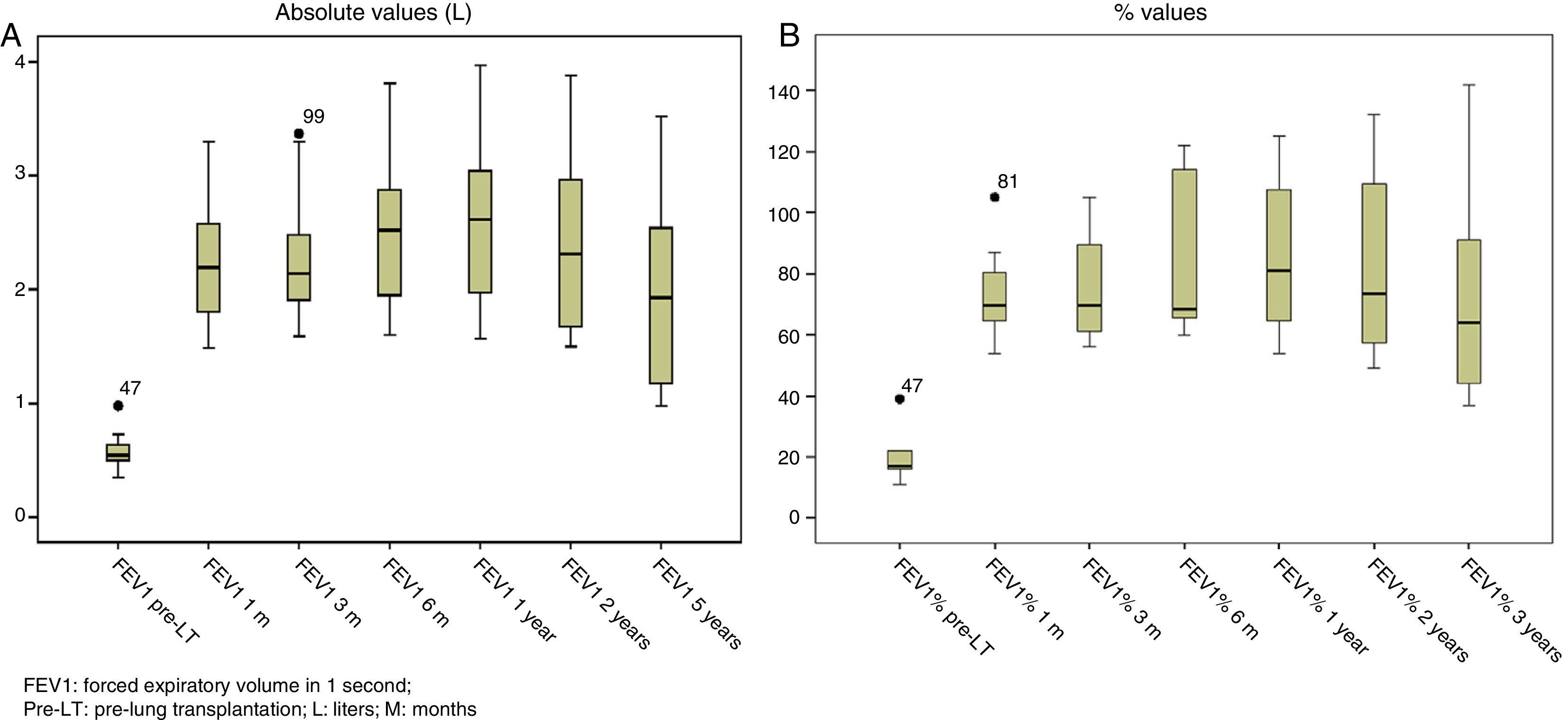
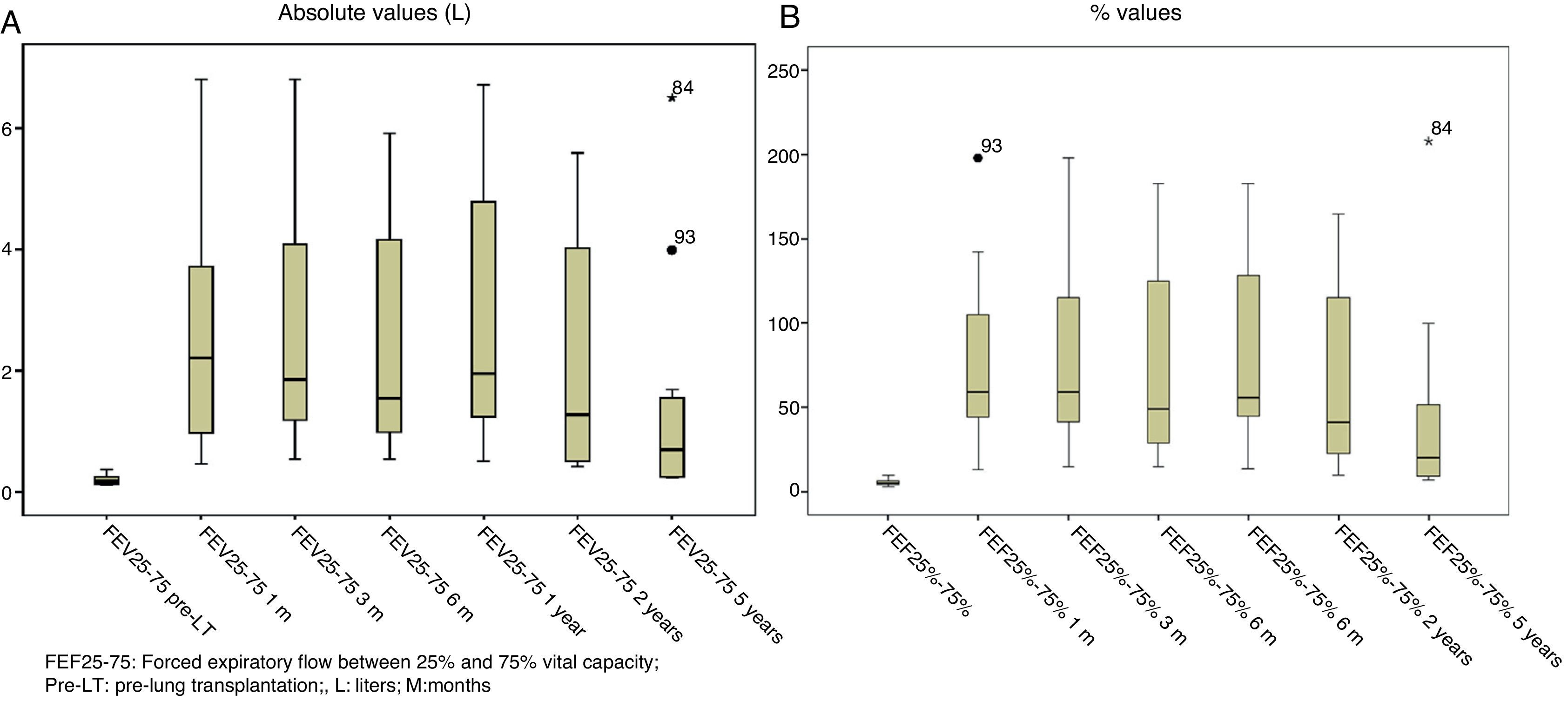
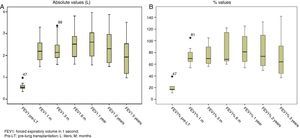
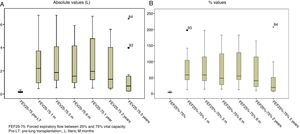
Lung function test values improved significantly after LT, both in absolute and in relative terms, and remained stable for the 5 years following the procedure, with the exception of FEF25–75, that fell sharply after year 5, reflecting the development of BOS and, as such, chronic graft rejection (Figs. 1 and 2).
Overall 1-year, 2-year and 5-year survival in our series was 65.4%, 56.8% and 40.9%, respectively.
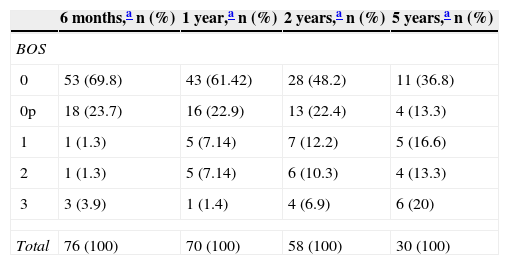
Lung function test results were used to define long-term lung graft status, and BOS status was determined for all survivors in each check-up (Table 3), using the ISHLT international consensus document.16
Bronchiolitis Obliterans Syndrome (BOS) Status at Follow-Up Visits.
Lung function values of patients before LT, in absolute and relative terms, were compared with results obtained in the scheduled follow-up visits. Statistically significant differences were found in FVC [+1.22L (+34.9%)], L1 [+1.66 L (+56.7%)] and FEF25–75 [+1.8 L (+50.8%)] (P=.001); these were maintained 5 years after the procedure.
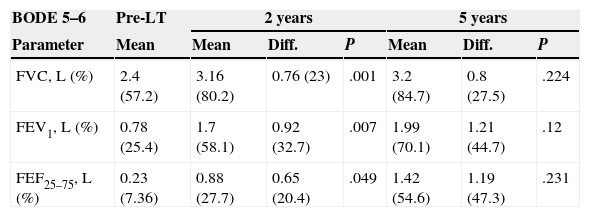
When patients were stratified into quartiles according to their BODE index and lung function results were compared, statistically significant improvements were only seen in the group with a BODE index higher than 7 (Table 4).
Comparison of Lung Function Tests Pre and Post-Lung Transplantations Stratified by BODE Score.
| BODE 5–6 | Pre-LT | 2 years | 5 years | ||||
|---|---|---|---|---|---|---|---|
| Parameter | Mean | Mean | Diff. | P | Mean | Diff. | P |
| FVC, L (%) | 2.4 (57.2) | 3.16 (80.2) | 0.76 (23) | .001 | 3.2 (84.7) | 0.8 (27.5) | .224 |
| FEV1, L (%) | 0.78 (25.4) | 1.7 (58.1) | 0.92 (32.7) | .007 | 1.99 (70.1) | 1.21 (44.7) | .12 |
| FEF25–75, L (%) | 0.23 (7.36) | 0.88 (27.7) | 0.65 (20.4) | .049 | 1.42 (54.6) | 1.19 (47.3) | .231 |
| BODE 7–10 | Pre-LT | 2 years | 5 years | ||||
|---|---|---|---|---|---|---|---|
| Parameter | Mean | Mean | Diff. | P | Mean | Diff. | P |
| FVC, L (%) | 2.05 (53.3) | 3.33 (87.4) | 1.28 (34.1) | <.001 | 3.33 (89.3) | 1.28 (36) | <.001 |
| FEV1, L (%) | 0.62 (20) | 2.38 (78.8) | 1.76 (58.8) | <.001 | 2.34 (78.4) | 1.72 (58.4) | <.001 |
| FEF25–75, L (%) | 0.22 (6.9) | 2.25 (61.8) | 2.03 (54.9) | <.001 | 2.17 (58.2) | 1.95 (51.3) | <.001 |
Diff: difference; FEF25–75: forced expiratory flow between 25% and 75% of vital capacity; FEV1: forced expiratory volume in 1s; FVC: forced vital capacity; L: liters; Pre-LT: pre-lung transplantation.
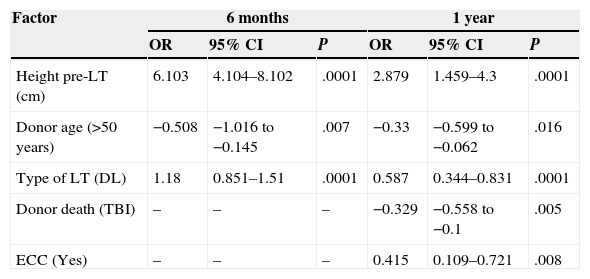
In the multivariate analysis, regression variables with a statistically significant impact during follow-up were age, cause of donor death, recipient height, type of LT, use of ECC during surgery, and the presence of BOS in the long-term evaluations, as shown in Table 5.
Prognostic Factors for Long-Term Functional Outcome (FEV1) (liters) Multivariate Analysis.
| Factor | 6 months | 1 year | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | |
| Height pre-LT (cm) | 6.103 | 4.104–8.102 | .0001 | 2.879 | 1.459–4.3 | .0001 |
| Donor age (>50 years) | −0.508 | −1.016 to −0.145 | .007 | −0.33 | −0.599 to −0.062 | .016 |
| Type of LT (DL) | 1.18 | 0.851–1.51 | .0001 | 0.587 | 0.344–0.831 | .0001 |
| Donor death (TBI) | – | – | – | −0.329 | −0.558 to −0.1 | .005 |
| ECC (Yes) | – | – | – | 0.415 | 0.109–0.721 | .008 |
| Factor | 2 years | 5 years | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | |
| Height pre-LT (cm) | 3.842 | 1.492–6.192 | .002 | 3.144 | 0.144–6.145 | .041 |
| Type of LT (DL) | 0.856 | 0.418–1.295 | .0001 | – | – | – |
| BOS (Yes) | −0.6 | −0.105 to −0.015 | .01 | −1.469 | −2.023 to −0.915 | .0001 |
BOS: bronchiolitis obliterans syndrome; DL: double-lung; ECC: extracorporeal circulation; CI: confidence interval; OR: odds ratio; pre-LT: pre-lung transplantation; TBI: traumatic brain injury.
It has been our experience that COPD patients who receive LT show improved lung function values during the 5 years post-surgery. Among these values, FEV1, the main indicator of COPD severity, was the parameter that improved most after LT, as shown by the spirometry evaluations performed at 1 month. Values remained above the pre-LT reference values for over 5 years.
These results are in line with many studies that also analyzed these parameters. These improvements in lung function values after LT, with absolute FEV1 values of over 2 L18 and relative improvements of over 25%–75%,19 were observed as early as the 1990s.
These results were later consolidated in many publications, and better lung function values have been demonstrated after LT, generally reflected in improved FEV1 figures.8,20–27 No authors have reported contradictory results.
When pre- and post-LT lung function values are compared, with patients stratified according to their BODE index quartile,15 significant differences are observed between spirometry results in the group with BODE scores of between 7 and 10; these were maintained as long as 5 years after LT. However, these results were not repeated in the group with BODE scores of between 5 and 6, in whom the spirometric benefit was only maintained during the first 2 years post-LT: at 5 years, none of the values analyzed achieved statistical significance.
In our series, 26 patients with BODE scores below 7 were transplanted, mainly during the first stages of the program before the international consensus had been published.14 They were included in the LT program on the basis of deteriorating clinical and lung function criteria that in the early days were the main basis for LT indication. Today, these criteria might be questionable, although they are still recognized as an alternative or add-on to the BODE index.
We have found no other references or earlier contributions analyzing the differences in lung function results according to BODE quartile after LT, although some studies have analyzed the stratification of patients according to their BODE group in terms of survival,12,28 raising doubts regarding the suitability of the procedure for patients with a score of less than 7.
Our results suggest that COPD patients with a poorer clinical status (BODE index greater than 7) derive greater and longer-lasting benefits from LT, in terms of long-term lung function; improvement is not so clear-cut in patients who are initially more stable.
Possible factors influencing this spirometric improvement were analyzed and the type of LT was found to affect long-term lung function, even if it did not impact on survival in our series.29 Similarly, several other studies have also reported significantly better outcomes in patients undergoing DLT compared to SLT, with absolute long-term gains in FEV1 of around 1L.18,19,21,22
We found that the use of ECC was associated with improved lung function at 1 year. This finding is difficult to explain, since it has not been observed in previous studies, unless it can be taken as a confounding factor associated with the type of LT, since ECC was only used in DLT. This also seems to contradict previous publications that suggest that the use of ECC has a deleterious effect on the lung, since it increases acute lung insult and may even cause early lung graft dysfunction,7,30,31 which of course would be a risk factor for long-term functionality.
Other variables analyzed in our study, such as donor age or oxygenation status in the first hours post-LT, affected long-term function. However, the fact that the differences only achieved significance in certain moments of the disease course suggest that our results should be interpreted with caution, and that consistent conclusions cannot be drawn.
It was interesting to find that the height of the recipient influenced outcome, since it was consistently identified as a factor for lung function improvement: the taller the recipient, the better their long-term lung function.
The incidence of BOS in our series varied depending on when it was analyzed during the course of the disease. At the 6-month evaluation, 6.5% of survivors were found to have developed BOS, while it was detected in 45.5% of survivors at the 5-year visit. These data are similar to those of the latest ISHLT report that set the 5-year rate of BOS at 49%.7
Our study has some significant limitations. First, its retrospective nature may cause memory and detection bias, which may also be affected by the long period under study, during which diagnostic methodology has changed. Moreover, because of the small size of our sample, understandable in view of the rarity of the study procedure, we must be cautious in interpreting the data and results. Multicenter, randomized, prospective studies are needed to provide better evidence on which to base conclusions.
To conclude, LT, and in particular DLT, confer long-term, stable improvement in lung function in COPD patients with a BODE index greater than 7. This improvement could not be confirmed in patients with lower BODE scores.
AuthorshipJosé Cerón Navarro, principal investigator, contributed to the database set-up, analysis and writing of the article.
Karol de Aguiar Quevedo, Carlos Jordá Aragón, Emilio Ansótegui Barrera, Juan Carlos Peñalver Cuesta and Nuria Mancheño Franch participated actively in data collection, database set-up and data analysis.
José Padilla Alarcón and Francisco José Vera Sempere
contributed to writing the manuscript and overseeing the study.
Conflict of InterestsThe authors declare that they have receiving no funding for this study.
Please cite this article as: Cerón Navarro J, de Aguiar Quevedo K, Ansótegui Barrera E, Jordá Aragón C, Peñalver Cuesta JC, Mancheño Franch N, et al. Resultados funcionales del trasplante pulmonar en la enfermedad pulmonar obstructiva crónica. Arch Bronconeumol. 2015;51:109–114.