The objective of this study was to investigate whether a patient's maximum capacity is comparable in 2 different stair-climbing tests, allowing the simplest to be used in clinical practice.
MethodProspective, observational study of repeated measures on 33 consecutive patients scheduled for lung resection. Stair-climbing tests were: the standard test (climb to 27m) and the alternative fixed-altitude test (climb to 12m). In both cases, heart rate and oxygen saturation were monitored before and after the test. The power output of stair-climbing for each test (Watt1 for the standard and Watt2 for the fixed-altitude test) was calculated using the following equation: Power (W)=weight (kg)*9.8*height (m)/time (s). Concordance between tests was evaluated using a regression model and the residuals were plotted against Watt1. Finally, power output values were analyzed using a Bland–Altman plot.
ResultsTwenty-one male and 12 female patients (mean age 63.2±11.2) completed both tests. Only 12 patients finished the standard test, while all finished the fixed-altitude test. Mean power output values were Watt1: 184.1±65 and Watt2: 214.5±75.1. The coefficient of determination (R2) in the linear regression was 0.67. No fixed bias was detected after plotting the residuals. The Bland–Altman plot showed that 32 out of 33 values were within 2 standard deviations of the differences between methods.
ConclusionsThe results of this study show a reasonable level of concordance between both stair-climbing tests. The standard test can be replaced by the fixed-altitude test up to 12m.
El objetivo de este estudio es conocer si en una prueba de subir escaleras en la que solo se asciende una altura fija de 12m se desarrolla una potencia similar a la de la prueba estándar, lo que significaría que ambas son equivalentes.
MétodoEstudio prospectivo, observacional de medidas repetidas en 33 pacientes consecutivos valorados para resección pulmonar. Prueba estándar: límite de 27m de altura; prueba altura fija: 12m. Se monitorizaron saturación de oxígeno y frecuencia cardiaca al inicio y al final del ejercicio y se midió el tiempo de esfuerzo. La potencia desarrollada en cada prueba se calculó (Watt1: estándar y Watt2: altura fija) mediante: Potencia (Watt)=peso (kg)*9,8*altura (m)/tiempo(seg). Para evaluar la equivalencia entre potencias, se construyó un modelo de regresión lineal y se contrastaron gráficamente los residuos. Los valores de las potencias se analizaron mediante el método de Bland y Altman.
ResultadosVeintiún varones y 12 mujeres realizaron ambas pruebas. Edad media 63,2±11,2. Solo 12 pacientes terminaron la prueba estándar. Todos acabaron la prueba de 12m. Los valores de potencia alcanzados fueron Watt1: 184,1±65 y Watt2: 214,5±75,1. En la regresión lineal, R2 fue 0,67. No se encontró ningún sesgo en la distribución gráfica de los residuos. El análisis de Bland y Altman mostró que 32 de los 33 valores de potencia estaban dentro de las 2desviaciones estándar de las diferencias entre métodos.
ConclusiónLos resultados muestran un nivel razonable de concordancia entre ambas pruebas de subir escaleras por lo que la prueba corta podría sustituir a la estándar.
Predictive models allow patients to be classified according to their surgical risk in lung resection. If the risk is considered excessive, non-surgical treatment of the neoplasm is recommended. According to general consensus, the cardiopulmonary exercise test (CPET) with measurement of oxygen consumption (VO2), performed in the lung function laboratory, is the most sensitive and specific method for predicting this risk.1 However, this test is not available in all hospitals, and in those where it is used, a considerable number of candidates may have to forego it due to limited availability and other circumstances.2
The European Respiratory Society and European Society of Thoracic Surgeons (ERS/ESTS) clinical practice guidelines published in 20093 recommend that patients undergo a low technology screening test prior to prescribing a CPET.1,3 This enables clinicians to identify patients with a high VO2 level despite abnormal lung function tests. The symptom-limited stair-climbing test is one of 2 recommended.1,3 This test, however, has its drawbacks, suggesting that a low cost, low technology (compared with CPET) test that is easier to standardize and safer for the patient than the 22m climb test would be an interesting alternative.
Patients who cannot reach 22m in the standard stair-climbing test4 have been shown to have a higher probability of postoperative cardiopulmonary complications (CPC), as these are patients with deconditioned cardiopulmonary, vascular and muscular systems.5
In recent years, 2 groups of investigators have published a variation of the symptom-limited stair-climbing test.6–8 Ambrozin et al.8 named their variation the fixed altitude stair-climbing test. Both groups encouraged the patient to climb to a fixed altitude (12.6m or 20m), less than in the symptom-limited test, as fast as they could. The variation lies in that it is the time taken6,8 or speed.7,9 at which the patient climbs to this altitude that is measured. Both groups found a significant association between the parameters measured and CPC,8 and also with the patient's VO2.7,9 However, none of these studies analyzed the possible relationship between these variations of the stair-climbing test and the test described by Brunelli et al.4 and recommended in the latest 2 clinical guidelines published.1,3
The aim of this study was to determine whether a variant of the symptom-limited stair-climbing test, in which the patient is invited to climb to a fixed altitude of 12m as quickly as possible, generates a power output similar to that of the symptom-limited stair-climbing test (to at least 22m). This would suggest that both tests are equivalent. If this is the case, the short test could replace the standard test accepted in clinical practice guidelines.
MethodsThis was a prospective, repeated-measures observational study conducted in March 2014.
Study PopulationWe included 33 consecutive patients with any diagnosis who were referred to the thoracic surgery clinic for lung resection assessment. All patients met the minimum operability criteria published previously,10 agreed to undergo the proposed lung surgery, and had no limitations for climbing stairs due to joint problems or unstable comorbidities. The inclusion of patients with ischemic heart disease in the study was conditional upon previous coronary revascularization or evidence of good functional capacity evidenced by ergometry or an equivalent examination.
All patients signed an informed consent form and the study was authorized by the local ethics committee.
Exercise TestsAll patients performed the 2 stair-climbing tests in the hospital, on the same stairs and accompanied by the same team of doctors. The 2 doctors who accompanied the patient monitored their vital signs and took the appropriate measurements. They were prepared to halt the test if the patient's condition so advised, and to provide medical assistance if required.
The height of the stairs was measured at various levels to determine the real altitude of each flight of stairs, and to accurately determine the altitude reached by the patient in the long test and the point at which the patient had climbed 12m from a fixed starting point.
Both tests were carried out within 3 weeks of each other. As a rule, the symptom-limited stair-climbing test was done on the day of the assessment in outpatients, while the fixed-altitude test was done on the day of admission prior to the procedure. All patients were weighed before performing the second test to confirm that there had been no changes in their weight between both tests.
Before climbing the stairs, the patient did a 3–5min leg warm-up on an unloaded cycle ergometer.
Both types of tests ended when the patient stopped at any point on the flight of stairs, the doctor accompanying the patient suspended the test due to the onset of warning signs, or when the stipulated altitude of 12m or 27m was reached.
The standard test4 consisted of climbing up to 27m (8 floors), at a steady pace as far as possible, without holding on to the banister except in the case of instability. In the fixed-altitude test, the patient was asked to climb 12m as quickly as possible. In both tests, the patients were encouraged by the staff accompanying them to keep going.
Variables CollectedPatient demographic variables were recorded: age, sex, weight, height and lung function studies (FVC%, FEV1%, FEV1%/FVC and DLCO%).
The following parameters were recorded during the exercise tests: heart rate and oxygen saturation immediately before beginning the ascent and on finishing the test; exact altitude climbed; time taken and reason for not completing the test: dyspnea, claudication of the lower extremities, angina, dizziness, joint pain or other problems.
Using these data, the speed of ascent and power output in each exercise were calculated. The following formula was used for the latter: Power (W)=weight (kg)*9.8* altitude ascended (m)/time taken (s).
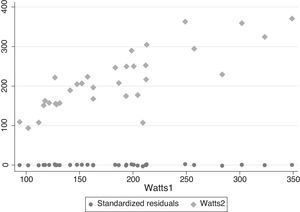
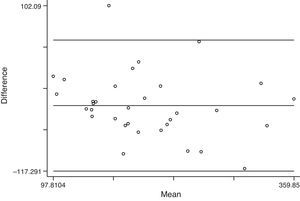
Statistical AnalysisFirst, a linear regression model was developed to determine whether a linear relationship existed between the power output reached in each test. In this model, the power output reached during the 12m stair-climbing test (Watt2) was considered the dependent variable and the power output reached in the 27m test (Watt1) the independent variable. In order to detect any possible fixed bias in the measurement of the power outputs, the residuals of this regression were plotted against the Watt1 value in a graph. Finally, a Bland–Altman plot was constructed,11 and Pitman's test was performed to calculate the probability that the differences between the variances of the mean power output values and the values of the 2 power outputs (Watt1 and Watt2) were due to chance. The calculations were performed using Stata 13.
ResultsTwenty-one male and 12 female patients completed both tests. Mean patient age was 63.2 years (Table 1).
In the symptom-limited stair-climbing test, 21 patients did not reach the altitude of 27m; of these, 17 did not reach 22m, recognized as the limit for classifying the patient as low risk and excluding the need for CPET. Nine patients stopped the test due to dyspnea, 9 due to claudication of the lower extremities, 2 due to joint pain, and 1 due to dizziness and unsteadiness. All patients reached 12m in the second test. On comparing the data obtained in the 2 tests (Table 2), the heart rate and saturation on finishing the exercise and the percentage increase in the heart rate with respect to the maximum heart rate calculated according to the patient's age were similar.
Average Data Obtained From the 2 Stair-climbing Tests.
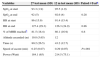
| Variables | 27 test mean (SD) | 12m test mean (SD) | Paired t-Testa |
|---|---|---|---|
| SpO2 at start | 93.3 (1.9) | 95.5 (1.9) | |
| SpO2 at end | 92 (5) | 92.6 (4) | 0.28 |
| HR at start | 86 (15.9) | 91.4 (15.4) | |
| HR at end | 127.4 (29.3) | 126.3 (24.9) | 0.86 |
| % of MHR reachedb | 81.5 (18.4) | 80.1 (16.9) | 0.8 |
| Altitude ascended (m) | 19.8 (5.65) | 12 | |
| Time (s) | 80.2 (26.5) | 43.2 (12.7) | |
| Speed of ascent (m/s) | 0.25 (0.07) | 0.29 (0.07) | P<.001 |
| Power (Watt) | 184.1 (65) | 214.5 (75.1) |
HR: heart rate.
Fig. 1 shows the graph of the relationship between the 2 power outputs calculated. There is a linear relationship between both variables (P>.001) and the model explains to a large extent the variability found in power outputs (R2=0.67). Residual analysis did not detect any specific bias in the measurements (Fig. 1). Finally, the Bland–Altman plot (Fig. 2) showed that 32 out of 33 values were within 2 standard deviations of the difference of the power output values obtained with both tests (P=.173).
Out results suggest that both tests are reasonably equivalent. This is not only shown by the specific study of power outputs, but by similarities in heart rate on finishing the exercise, percentage variation in heart rate with respect to age during the exercise, and saturation on finishing both types of exercise (Table 2). However, a substantial number of patients were unable to complete the standard test, while all were able to reach 12m with relative ease.
Despite having been accepted in the latest 2 clinical practice guidelines,1,3 the symptom-limited stair-climbing test4 as a low technology screening test has been highly criticized, particularly for its lack of standardization and patient safety. Increasing patient safety during the exercise is difficult, as the test takes place outside a controlled environment. To improve standardization, it must be carried out on a single stairway where the height of the stairs has been carefully measured, and the point at which each key event occurs can be accurately determined: the altitude at which the exercise ends, and the altitude of 22m, considered as a cutoff point for classification of the patient's surgical risk. These 22m correspond to approximately 7 floors, although they can vary according to the architectural characteristics of the building.
The physiological rationale for the stair-climbing test is based on the need for the patient to reach a certain level of metabolic stress that somehow mirrors the stress to which they will be subjected during the perioperative period. The level of activity in preoperative studies has been found to be greater than the level required for the intervention.12 It is estimated that in order to maintain a perioperative VO2 demand of 5ml/kg/min, the patient's anaerobic threshold should be above 11ml/kg/min in normal conditions.12 In the low technology tests, the degree of activity, or more accurately, the power output reached during the test, gives an estimation of the patient's aerobic capacity, as power output is one of the main factors in the VO2 calculation.13
The recent introduction of alternative stair-climbing tests, published by Brunelli et al.4 and accepted in the most recent guidelines, is innovative because of the different relationships between established and analyzed variables. Various groups have studied other versions of the stair-climbing test, reporting that all were able to detect patients with a very high risk of complications,14–16 or correlating the altitude reached by the patient with their lung function.17,18 Pollock et al.18 were the first to correlate the climbing test with the patient's VO2. In their test, however, patients climbed at their own pace, without being encouraged to keep up the effort. Brunelli et al. modified that aspect by inviting patients to climb at a faster, less comfortable pace than they would have used in a normal situation, and to maintain this speed. This meant that patients climbed to a much higher altitude than that recorded in previous studies. Developing a shorter test but encouraging the patient as they climbed, Cataneo and Cataneo found that the time taken to climb to 12.16m maintained a good correlation (R2=−0.7) with the patient's VO2 measured in the standardized laboratory test.6 In a later study, Ambrozin et al.8 found significant differences between mean time and mean power output reached by patients with CPC with respect patients with no CPC in the postoperative period following lung resection. This study showed that the prevalence of CPC was directly proportional to the time needed to make the ascent: they recorded 14% CPC in those who took less than 30s and 60% in those who needed more than 50s. The South African group, meanwhile, found speed of ascent to be the parameter that predicted CPC.7,9 This speed had a high correlation with the VO2 measured in the laboratory test (R2=0.67), and they concluded that a patient capable of climbing at a speed of 15m/min had an estimated VO2 of at least 20ml/kg/min and could therefore even tolerate a pneumonectomy without the need for further studies.7
A stair-climb of only 12m is consistent with the findings of various investigators4,6,15 that have shown that ascending to an altitude of 12–14m (approximately 3 floors) was sufficient to identify patients with a low risk of suffering postoperative complications despite having abnormal lung function tests. Furthermore, this altitude of 3 floors is very tolerable when compared with the altitude used in the standard test (at least 7 floors). It also enables patients who are least fit but with an acceptable VO2 level to climb without stopping. Our experience with the standard test has shown that a significant number of patients sent for CPET because they did not reach the critical altitude of 22m have a good VO2 level, but performed poorly because they were unused to physical exercise (unpublished data).
This study has some limitations. Firstly, it is a pilot study, so the results have yet to be confirmed in a larger population and validated by other investigators. Additionally, all the patients included had already been selected for surgery in other centers in accordance with some consensual criteria. This limitation is very difficult to overcome, and is inherent to all surgical departments. Finally, it is important to note that during the first visit, patients learn breathing exercises and are encouraged to increase their daily of physical exercise.19 This could suggest that the 2 tests were performed in different conditions.
In conclusion, the data suggest that the 2 stair-climbing tests are reasonably equivalent, and therefore the 12m fixed-altitude test can be used instead of the symptom-limited stair-climbing test in the preoperative evaluation of patients referred for lung resection assessment. The cutoff point for evaluating the surgical risk has yet to be determined.
Conflict of InterestsThe authors declare that they do not have any conflict of interests that could cause any bias in this study.
Please cite this article as: Novoa NM, Rodríguez M, Gómez MT, Jiménez MF, Varela G. La prueba de escaleras limitada por altura podría sustituir a la prueba estándar en la evaluación funcional previa a la resección pulmonar. Estudio piloto. Arch Bronconeumol. 2015;51:268–272.