Exacerbations of Chronic Obstructive Pulmonary Disease (COPD) that require hospital admission have a major impact on the progression of disease and generate high health costs.
MethodA multi-center, cross-sectional, observational study was conducted with the aim to identify factors associated with hospital admission in patients with COPD. We obtained data of socio-demographic and anthropometric characteristics, quality of life, respiratory symptoms, anxiety and depression, physical activity and pulmonary function tests. We analyzed their association with hospital admission with a multivariate analysis using a logistic regression model.
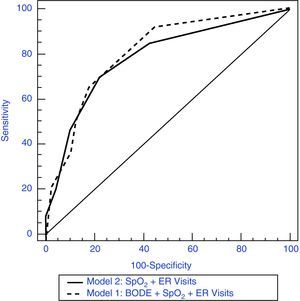
ResultsWe analyzed 127 patients, 50 (39%) of whom had been hospitalized. 93.7% were men, mean age 67 years (SD=9) and a FEV1 of 41.9% (SD=15.3). In the first model obtained, the baseline SpO2, the BODE index and emergency room (ER) visits were associated with hospital admission and the area under the ROC curve (AUC) was 0.809. In a second model we included only variables readily available (without the 6min walking test) and only the SpO2 and previous visits to the ER were significant with an AUC ROC 0.783.
ConclusionsHospital admission for exacerbation of COPD is associated with poor SpO2, higher BODE index score and a greater number of visits to the ER. In case you do not have the 6min walking test, the other two variables offer a similar discriminative ability.
Las exacerbaciones de la enfermedad pulmonar obstructiva crónica (EPOC) que precisan ingreso hospitalario tienen un gran impacto en la progresión de la enfermedad y generan un alto gasto sanitario.
MétodoSe trata de un estudio observacional, multicéntrico y transversal, con el objetivo de identificar los factores asociados a las hospitalizaciones por exacerbaciones de la EPOC. Se obtuvieron variables sociodemográficas, antropométricas, de calidad de vida, síntomas respiratorios, presencia de ansiedad y depresión, actividad física y pruebas de función pulmonar. Se analizó su asociación con el ingreso hospitalario mediante análisis multivariante con un modelo de regresión logística.
ResultadosSe analizaron 127 pacientes, 50 (39%) de los cuales habían sido hospitalizados. El 93,7% fueron hombres, con una edad media de 67 años (DE=9) y un FEV1 del 41,9% (DE=15,3). En el primer modelo obtenido, la SpO2 basal, el índice BODE y las visitas a urgencias se asociaron con el ingreso, y el área bajo la curva (ABC) ROC fue de 0,809. En un segundo modelo incluimos solo variables de fácil obtención (sin la prueba de la marcha), y solo la SpO2 y las visitas previas a urgencias fueron significativas, con un ABC ROC de 0,783.
ConclusionesEl ingreso hospitalario por exacerbación de la EPOC se asocia a peor SpO2, mayor puntuación del índice BODE y un mayor número de visitas al servicio de urgencias. En caso de no disponer de la prueba de caminar 6min, las otras dos variables ofrecen una capacidad discriminativa similar.
Due to its high mortality and morbidity, chronic obstructive pulmonary disease (COPD) is a public health problem in developed countries that will extend worldwide in the near future.1
The course of COPD shows periods of abrupt worsening of the symptoms, known as exacerbations, which may have multiple etiologies.2,3 These episodes entail an increase in bronchial and systemic inflammation in addition to the chronic inflammation associated with COPD.
COPD patients suffer approximately between 1 and 2 exacerbation episodes annually, with an even greater frequency in more severe patients. Patients with frequent exacerbations (more than 3 annual episodes) likewise present a faster fall in FEV1,4 demonstrate more airway inflammation when clinically stable5 and have poorer health-related quality of life.6,7
COPD exacerbations represent the large majority of COPD treatment costs. This expense comes mainly from hospitalizations, especially from hospital admissions after outpatient treatment has failed,8,9 which ranges between 13% and 25%. Due to its importance, there is special interest in understanding the factors associated with the development of COPD exacerbations and the factors that can predict hospitalization. The identification of these factors would enable us to recognize high-risk patients in whom medical intervention should be more intensive in order for such patients to avoid hospitalization, with an improvement in health parameters and the consequent reduction in costs that hospitalization entails.
The present study has been designed with the aim to identify factors associated with hospitalization due to COPD in a group of patients recruited from hospital centers in Spain.
Patients and MethodsOurs is a cross-sectional, observational, multi-center study of COPD patients who were seen in an ambulatory setting during stable phase of their disease. The individuals eligible for the study were required to meet the following inclusion criteria: age≥40, smoker or ex-smoker of at least 10 pack-years, diagnosed with COPD based on the criteria of the GOLD guidelines1 (post-bronchodilator FEV1/FVC ratio<0.70) in stable phase as determined by the clinician in charge and at least one month after hospital discharge. The patients included in the study were divided into two subgroups according to whether they had needed hospitalization in the previous year. In cases where there was clinical suspicion of sleep apnea-hypopnea syndrome (SAHS), the standard complementary tests were carried out.
The study was approved by the local ethics committee and the clinical research committee of the Hospital Puerta del Mar in Cádiz, Spain. All the participants gave their written informed consent.
For each patient included in the study, data were compiled for socioeconomic level, pharmacological treatment, the number of hospitalizations and their duration, visits to the emergency room and unscheduled visits to the primary-care physician in the previous year due to COPD exacerbation. Blood samples were obtained and a complete blood work-up and biochemistry were ordered with plasma determinations of ferritin, alpha-1-antitrypsin and C-reactive protein (CRP). The patients also underwent resting arterial blood gas studies, lung function testing and a 6-min walk test, all in accordance with published protocols.10 The degree of baseline dyspnea was measured with the Medical Research Council (MRC) scale.11 In order to evaluate the cardiac function, electrocardiograms and echocardiography were performed. Finally, for each patient body mass index, obstruction, dyspnea and exercise capacity (BODE index) were calculated.12
Comorbidities were quantified by means of the Charlson comorbidity index.13 The evaluation of the health-related quality of life was evaluated with the 5-dimension EuroQOL questionnaire (EQ-5D),14 translated and validated in Spanish, the physical activity scale of the London Chest Activity of Daily Living (LCADL),15 also translated and validated in Spanish, and the Spanish version of the Hospital Anxiety and Depression scale (HAD).16
Statistical AnalysisThe quantitative variables are shown as number of subjects that present the datum, mean and standard deviation. For qualitative variables, absolute and relative frequencies are presented. The comparison of the continuous variables was done with the use of the Student's t-test in the case of normal distribution and the Mann–Whitney U-test for the variables with non-normal distribution. For the comparison of categorical variables, the Chi-squared test was used and the P values associated with said test are presented.
A multivariate analysis was completed using a logistic regression model, adjusting the variable being studied (hospitalization) with the variables that demonstrated significant differences between the two groups in the bivariate analysis: sex, age, level of studies, EQ-5D score, Charlson index, LCADL and HAD-Anxiety and HAD-Depression subscales, degree of dyspnea on the MRC, BODE, visits to the ER, FEV1, and partial oxygen saturation (SpO2). The variables were outside the logistic regression model when P>.1.
With the variables in the regression analysis associated with hospital admittance, two models were constructed, for which the area under the curve (AUC) was calculated along with the 95% confidence interval.
The tables, lists, analyses and charts were produced with the SPSS v.18 statistical software package. A P value <.05 was considered statistically significant.
ResultsThirteen researchers participated in the study that included 127 patients. Table 1 shows the anthropometric and sociodemographic characteristics of the included subjects. Of these, 93.7% were men, with a mean age of 67.3 (SD=8.7), and the majority had either no studies or only primary school studies (72.4%). Only 25.2% were active smokers, but the accumulated tobacco consumption was high at 55.5 pack-years (SD=27.8). No significant differences were found in these parameters regarding previous hospitalization (Table 1).
Study Population Characteristics.
| Parameter | Hospitalization 50 (39.4%) | No Hospitalization 77 (60.6%) | Total 127 (100%) | P value |
| Age | 68.5 (9.3) | 66.5 (8.2) | 67.3 (8.7) | .193 |
| Sex – male | 48 (96.0%) | 71 (92.2%) | 119 (93.7%) | .376 |
| Family situation | ||||
| Lives alone | 5 (10%) | 6 (7.8%) | 11 (8.6%) | .707 |
| With spouse | 35 (70%) | 51 (66.2%) | 86 (67.7%) | |
| With family members | 10 (20%) | 20 (26%) | 30 (23.6%) | |
| BMI, kg/m2 | 25.8 (5.3) | 27.3 (4.9) | 26.7 (5.1) | .089 |
| Level of studies | ||||
| No studies | 16 (32%) | 20 (26%) | 36 (28.3%) | .089 |
| Primary | 26 (52%) | 30 (39%) | 56 (44.1%) | |
| Secondary | 6 (12%) | 16 (20.8%) | 22 (17.3%) | |
| University | 2 (4%) | 11 (14.3%) | 13 (10.2%) | |
| Employment | ||||
| Active | 27 (54.0%) | 54 (70.1%) | 81 (63.8%) | .066 |
| Smoking | ||||
| Smoker | 12 (24.0%) | 20 (26%) | 32 (25.2%) | .80 |
| Non-smoker/ex-smoker | 38 (76%) | 57 (74%) | 95 (74.8%) | |
| Pack-years | 56.1 (27.8) | 55 (28) | 55.5 (27.8) | .84 |
| Alcohol abuse | 20 (20%) | 9 (11.7%) | 19 (14.9%) | .19 |
| % ER visits in the previous yeara | 35 (70%) | 17 (22.1%) | 52 (40.9%) | <.001 |
| ER visits in the previous year | 2.02 (2.6) | 0.6 (1.5) | 1.2 (2.1) | <.001 |
| % Primary-care visits in the previous yearb | 22 (44%) | 23 (29.9%) | 45 (35.4%) | .10 |
| Usual treatment | ||||
| Short-acting B2-agonists | 42 (84%) | 55 (71.4%) | 97 (76.4%) | .10 |
| Long-acting B2-agonists | 47 (94%) | 69 (89.6%) | 116 (91.3%) | .52 |
| Short-acting anticholinergics | 5 (10.2%) | 6 (7.9%) | 11 (8.6%) | 0.75 |
| Long-acting anticholinergics | 44 (88%) | 65 (84.4%) | 109 (85.8%) | .57 |
| Theophyllines | 13 (26.0%) | 10 (13.0%) | 23 (18.1%) | .06 |
| Inhaled corticosteroids | 48 (96.0%) | 68 (88.3%) | 116 (91.3%) | .19 |
| Mucolytics | 27 (54.0%) | 22 (28.6%) | 49 (38.6%) | .004 |
| Oxygen therapy | 21 (42.9%) | 8 (10.4%) | 29 (22.8%) | <.001 |
| Home mechanical ventilation | 7 (14%) | 2 (2.6%) | 9 (7.1%) | .028 |
| Respiratory rehabilitation | 6 (12.2%) | 8 (10.4%) | 14 (11.3%) | .74 |
| Anti-flu vaccine | 40 (80%) | 51 (66.2%) | 91 (73.4%) | .09 |
| Anti-pneumococcal vaccine | 14 (28%) | 29 (37.7%) | 43 (36.2%) | .26 |
The results are expressed as means (standard deviation). BMI: body mass index.
The data on the consumption of resources over the course of recent years are reflected in Table 1. No significant differences were detected in unscheduled outpatient care, but the patients with previous hospitalizations had more ER visits than those who had not been hospitalized (2.02±2.62 in the former vs 0.61±1.53 in the latter).
As for the standard treatment, those patients who were hospitalized more frequently received mucolytics (54% vs 28.6%; P=.004), as well as oxygen therapy (42.9% vs 10.4%; P<.001) and home mechanical ventilation (14% vs 2.6%; P=.03). There was an observed non-significant tendency towards a higher prescription of theophyllines and anti-flu vaccination among patients with previous hospital admittance (Table 1).
The degree of dyspnea was significantly greater in the group of hospitalized patients (36% had dyspnea grade 3 or 4, compared with only 15.6% in the non-hospitalized patients; P=.001). Differences were also obtained in arterial oxygen saturation, which showed much lower values in this subgroup of patients. As for the lung function, FEV1 in milliliters (ml) was lower in the patients who had been hospitalized, but not the FEV1 (%). Differences were detected in FVC (%), which was significantly lower in the group of patients requiring hospitalization (58.7% vs 74%; P<.001). The patients with prior hospital admittance had a more altered CO diffusion (Table 2).
Lung Function Testing.
| Parameter | Hospitalization (n=50) | No Hospitalization (n=77) | Total (n=127) | P value |
| pH | 7.4 (0) | 7.4 (0) | 7.4 (0) | .54 |
| pO2 | 63.1 (11.4) | 71.5 (10.7) | 68.2 (11.7) | <.001 |
| pCO2 | 46.6 (8.6) | 42.9 (8.3) | 44.4 (8.6) | .027 |
| SpO2, % | 90.9 (4.9) | 94.0 (3.2) | 92.8 (4.2) | <.001 |
| FEV1, % | 38.8 (14.1) | 44.3 (15.9) | 41.9 (15.3) | .07 |
| FEV1, mL | 1005 (398) | 1214 (492) | 1124 (464) | .020 |
| FVC, % | 58.7 (18.4) | 74.0 (19.7) | 67.4 (20.5) | <.001 |
| FVC, mL | 2056 (791) | 2640 (950) | 2490 (959) | <.001 |
| FEV1/FVC | 50.4 (13.9) | 45.9 (12.3) | 47.9 (13.1) | .08 |
| RV, % | 141.5 (56.6) | 150.6 (46.1) | 147.9 (49.3) | .43 |
| TLC, % | 99.9 (24.4) | 109.5 (22.6) | 106.4 (23.5) | .07 |
| DLCO, % | 47.3 (19.6) | 61.1 (19.1) | 56.7 (20.6) | .002 |
| Grade of dyspnea (MRC) | ||||
| 0 | 1 (2%) | 7 (9.1%) | 8 (6.3%) | .001 |
| 1 | 13 (26%) | 43 (55.8%) | 56 (44.1%) | |
| 2 | 18 (36%) | 15 (19.5%) | 33 (25.9%) | |
| 3 | 13 (26%) | 10 (13%) | 23 (18.1%) | |
| 4 | 5 (10%) | 2 (2.6%) | 7 (5.5%) | |
The values are expressed as means (standard deviation).
SpO2: transcutaneous oxygen saturation; RV: residual volume; FVC: forced vital capacity; FEV1: forced expiratory volume in one second; TLC: total lung capacity; DLCO: diffusing capacity of the lung for carbon monoxide.
In a subgroup of 60 patients, complete data were obtained for blood analysis and an echocardiogram was available. The results obtained are presented in Table 3. The patients hospitalized for COPD exacerbation showed lower levels of hemoglobin and total protein and, contrarily, greater total leukocyte count and greater concentration of serum fibrinogen. The echocardiographic examination showed greater pulmonary artery systolic pressure (PASP) and a greater frequency of tricuspid insufficiency in hospitalized patients.
Characteristics of the Biochemical Parameters and of the Echocardiographic Examination.
| Parameter | Hospitalization 23 (38.33%) | No Hospitalization 37 (61.66%) | P value |
| Hemoglobin, g/dl | 14.1 (1.4) | 14.9 (1.4) | .015 |
| Total leucocytes, 103/μl | 9.3 (2.5) | 8.1 (2.2) | .011 |
| Fibrinogen, mg/dl | 446.4 (156.6) | 356.5 (173.4) | .001 |
| Total proteins, mg/dl | 6.6 (0.5) | 7.2 (0.6) | <.001 |
| Alpha1-antitrypsin, mg/dl | 136.3 (37.7) | 144.1 (26.1) | .34 |
| CRP (ultra-sensitive), mg/dl | 3.9 (6.8) | 2.6 (4.2) | .38 |
| Ferritin, mg/dl | 186.6 (135) | 196.5 (142) | .81 |
| PASP, mmHg | 25.7 (24.8) | 13.1 (15.6) | .009 |
| Ejection fraction, VI (%) | 59.1 (12.9) | 61.3 (10.4) | .34 |
| Diastolic dysfunction, n (%) | 13 (17.6%) | 17 (22.9%) | .85 |
| Increase in right cavities, n (%) | 7 (9.5%) | 4 (5.4%) | .27 |
| Tricuspid insufficiency, n (%) | 19 (25.7%) | 14 (18.9%) | .04 |
The values are expressed as means (standard deviation). CRP: C-reactive protein; PASP: pulmonary artery systolic pressure.
The patients who were hospitalized presented a significantly more deteriorated quality of life, and their score in the EQ-5D index was 0.55 (SD=0.2) vs 0.64 (SD=0.2) in non-hospitalized patients (P=.01). There was a tendency towards lower scores in the anxiety and depression scales in hospitalized patients, but without reaching statistical significance although significant differences were found in the prevalence of possible anxiety and depression disorders between both groups. The BODE index showed a greater deterioration in the patients who required hospitalization (4.98 vs 3.02; P<.001) (Table 4).
BODE Index, Comorbidity, Physical Activity, Quality of Life and Anxiety and Depression Scales.
| Parameter | Hospitalization (n=50) | No Hospitalization (n=77) | P value |
| BODE index | 4.9 (2.3) | 3 (2.1) | <.001 |
| 6-min walk test, distance in meters | 315.9 (118) | 431 (117) | <.002 |
| Baseline dyspnea, MRC | 2.2 (1) | 1.4 (0.9) | <.001 |
| Charlson index | 3.7 (2.1) | 3.4±2.2 | .36 |
| London chest (LCADL) | |||
| Total score | 44.1 (15.9) | 41 (12.8) | .23 |
| EUROQOL | |||
| EQ-5D | 7.8 (2.1) | 6.5 (1.6) | .002 |
| EQ-5D (VAS) | 55.09±19.68 | 64.84±18.60 | .004 |
| Hospital scale for anxiety/depression | |||
| Anxiety subscale | 5.8 (4) | 4.5 (4) | .07 |
| Depression subscale | 5.6 (4) | 4.4 (4) | .08 |
| Hospital anxiety/depression scale (probable/confirmed cases) | |||
| Anxiety | 18 (32.7%) | 15 (18.9%) | .041 |
| Depression | 16 (29.09%) | 15 (18.9%) | .043 |
| Anxiety and depression | 10 (18.8%) | 7 (8.86%) | .053 |
The values are expressed as means (standard deviation). EQ-5D: EuroQoL five-dimension quality-of-life questionnaire; EQ-5D (VAS): EuroQoL quality-of-life questionnaire in visual analogue scale; LCADL: London Chest Activity of Daily Living scale.
The multivariate analysis included the variables obtained in the total population; therefore, the blood analysis variables and echocardiogram could not be used. Poorer SpO2, higher BODE index score and a greater number of ER visits were the variables that were significantly associated with having been hospitalized, with an AUC of 0.809 (Table 5, Fig. 1). In a second model, the 6-min walk test was excluded (and with it the BODE index), as it is a test that is not usually done in clinical practice. In this case, once again a poorer SpO2 and a greater number of previous ER visits were significantly associated with hospitalization, with an AUC that was very similar to the former model (0.783) (Table 6, Fig. 1).
Multivariable Analysis; Determining Factors for Hospitalization (Model 1).
| Parameter | OR | 95% CI |
| ER visits | 1.485 | 1.092–2.019 |
| EuroQuol-5D | 1.324 | 0.968–1.810 |
| EuroQuol (VAS) | 0.997 | 0.969–1.026 |
| Charlson | 1.053 | 0.849–1.306 |
| HAD anxiety | 0.996 | 0.866–1.145 |
| HAD depression | 0.880 | 0.866–1.145 |
| BODE | 1.303 | 1.054–1.610 |
| LCADL | 0.993 | 0.960–1.028 |
| SpO2 | 0.858 | 0.761–0.967 |
| Characteristics of Diagnostic Performance | |
| Sensitivity | 76.2% |
| Specificity | 77.3% |
| Positive predictive value (PPV) | 61.5% |
| Negative predictive value (NPV) | 87.2% |
| ROC curve | |
| AUC (visits index+BODE+SpO2) | 0.809 |
HAD anxiety: score on the hospital anxiety and depression scale, in the anxiety sections; HAD depression: score on the hospital anxiety and depression scale, in the depression sections depression; LCADL: London Chest Activity of Daily Living physical activity scale; SpO2: partial oxygen saturation.
Multivariable Analysis; Determining Factors for Hospitalization (Model 2).
| Parameter | OR | 95% CI |
| ER Visitas | 1.504 | 1.102–2.052 |
| EuroQuol-5D | 1.277 | 0.922–1.769 |
| EuroQuol (VAS) | 0.998 | 0.970–1.027 |
| Charlson | 1.073 | 0.863–1.335 |
| HAD anxiety | 0.997 | 0.865–1.149 |
| HAD depression | 0.879 | 0.744–1.039 |
| Dyspnea (MRC) | 1.644 | 0.932–2.899 |
| LCADL | 0.986 | 0.954–1.019 |
| BMI | 1.017 | 0.942–1.097 |
| SpO2 | 0.843 | 0.753–0.944 |
| Characteristics of Diagnostic Performance | |
| Sensitivity | 74.8% |
| Specificity | 78.1% |
| Positive predictive value (PPV) | 62.4% |
| Negative predictive value (NPV) | 86.1% |
| ROC curve | |
| AUC (SpO2 index+visits) | 0.783 |
HAD anxiety: score on the hospital anxiety and depression scale, in the anxiety sections; HAD depression: score on the hospital anxiety and depression scale, in the depression sections depression; LCADL: London Chest Activity of Daily Living physical activity scale; BMI: body mass index; SpO2: transcutaneous oxygen saturation.
The patients who had been hospitalized for COPD exacerbation reported a greater number of ER visits, had poorer scores on the BODE index and poorer arterial blood oxygen saturation. When the results of the 6-min walk test were not available, arterial O2 saturation and ER visits provided us with information that is very similar to that obtained by analyzing the BODE index. These variables are those that have been significantly and independently associated with previous hospitalization in a cohort of COPD patients from several hospital centers in Spain. Although the models proposed in this paper should be validated with a prospective cohort, the results described can aide in identifying patients with poorer prognosis and can be used at any health-care level.
COPD exacerbations requiring hospitalization, in addition to their prognostic importance, generate the majority of the health-care expenses of the disease.5,14 Thus, there are numerous studies that try to identify the factors associated with severe exacerbations that require hospitalization. One systematic review of 17 studies17 identified a greater variety of risk factors that included sociodemographic, psychological, lung function and treatment aspects together with the frequency of previous exacerbations. Nevertheless, the majority of the existing studies about risk factors for hospitalization are of the descriptive type, showing associated variables without establishing a clear cause-effect relationship. This would partially explain the heterogeneity of the results, as many of the factors analyzed can be confounding variables. In order to obviate as much as possible this contingency, a discriminating analysis is usually carried out. This was true in our case, in which we identified a small group of independent factors associated with hospitalization from a larger group observed in the univariate analysis.
Initially, the univariate analysis identified the poorer lung function, with lower FEV1 (ml), FVC and DLCO values with previous hospitalization, but these parameters were not significant in the multivariate analysis. This indicates that oxygen saturation is a better predictor of severity than spirometric variables, at least in this population of severe COPD from hospitals. In populations of patients seen in primary care with a greater spectrum of severity, FEV1 (%) was a factor associated with hospital admittance.18,19 In addition, in a recent epidemiological study, García-Aymerich et al.20 observed an association between the severity of COPD and the risk of hospitalization. In the cited study, however, other severity variables, like blood gases, were not analyzed, while in our population these variables were better predictors for hospitalization. We have not found significant differences in the frequency of active smoking or comorbidity between groups, and it is possible that in severe patients these factors are less decisive in the prognosis than in mild or moderate patients.
Dyspnea is the main symptom of COPD and it usually worsens during exacerbations. Despite being a prognostic indicator of mortality and even more precise than the degree of obstruction,21 it has not been described as an important factor in the prediction of hospitalization in COPD. Contrarily, in our study the intensity of dyspnea measured with the MRC scale was significantly higher in the hospitalized group. More intense dyspnea and poorer oxygen saturation indicate poorer physical aptitude; consequently, the distance walked was lower overall in hospitalized patients, above the clinically relevant difference.22 This would explain the differences observed in the BODE index between hospitalized and non-hospitalized patients, as the differences in FEV1 (%) and BMI were small in magnitude. Our results complement previous studies that have described the importance of the BODE index as a predictor for the risk of severe COPD exacerbations,23 and they have also observed that the BODE worsens significantly after exacerbations.24
Chronic diseases like COPD may be accompanied by psychiatric disorders, especially depression, which complicate and aggravate the prognosis and quality of life.25 The patients with previous hospitalization presented a greater prevalence of depressive disorders and anxiety than the non-hospitalized ones, but in the model obtained neither depression nor anxiety was independently associated with hospitalization. Our study probably does not have sufficient statistical power to demonstrate these associations, although they have been observed in previous papers.26 In any event, our data suggest an association between greater severity of COPD, greater frequency of psychiatric disorders and poorer quality of life, factors that can promote each other. Indeed, the hospitalization group showed poorer scores on the generic EQ-5D questionnaire, which was consistent with the studies that have reported a relationship between poorer quality of life, greater frequency of exacerbations and hospitalizations6 and even higher mortality in COPD.27
Due to organizational reasons, in some participating centers it was not possible to obtain variables for blood analysis variables or echocardiography in all the patients, so these variables were not included in the multivariate models in order to avoid losing the populations. This is one of the limitations of the study that has not allowed us to evaluate the impact of these alterations and their association with hospital admittance. However, from the analysis of the results obtained in the subgroup of 60 patients, we can suggest that the hospitalized patients have greater signs of chronicity (more anemia and lower concentrations of plasma proteins) and greater systemic inflammation (greater concentrations of fibrinogen and leukocytes). In an extensive series of COPD patients, anemia was more frequent (17%) than polycythemia (6%) and it was associated with greater dyspnea and a lower exercise capacity,28 but there is no evidence of its association with a higher risk for hospitalization. Anemia has also been associated with more intense systemic inflammation in COPD,29 as observed in our patients with previous hospitalization.
The presence of systemic inflammation in COPD has been well documented,30 and in particular high concentrations of circulating fibrinogen have been reported in COPD patients.29 This we have also identified in the patients with hospitalization. The high concentrations of fibrinogen have been associated with an increased risk of COPD exacerbations.31 A previous study observed that the elevated concentrations of fibrinogen, as observed in this current paper, were associated with poorer lung function and a higher risk for hospitalization, even after adjusting for possible confounding factors.32
In COPD, it is frequent to find cardiovascular comorbidity, which has an impact on its evolution and prognosis.33 From the echocardiographic study, we deduce that the hospitalized patients had greater signs of pulmonary arterial hypertension, with a greater systolic pressure in the pulmonary artery and greater frequency of tricuspid insufficiency. We have only found the identification of the greater pulmonary arterial pressure as a factor associated with risk for hospitalization in one previous study with 64 patients in whom this factor, together with high PaCO2, were the only hospitalization predictors in moderate–severe COPD patients.34 It is interesting to point out that our results agree with previous studies that relate the presence of pulmonary hypertension with a greater intensity of systemic inflammation,35 as occurs in our subgroup of patients with previous hospitalization.
Among the limitations of our study, we should mention its cross-sectional design, which allows us to suggest associations but does not enable us to identify causal relationships. The data obtained from previous studies suggest that the identified factors can work both ways: as markers that identify patients at greater risk for hospitalization,17,18 while also showing how hospitalizations can cause the disease to worsen, entailing a deterioration of the BODE index.22 The results presented should be interpreted as generators of hypotheses that would need to be demonstrated in more extensive and complex studies that are beyond the reach of this research group. On the other hand, we should also highlight two strengths of our study: its multi-center design and the diversity of the variables analyzed of COPD itself as well as its most important comorbidities, enabling us to analyze the main factors associated with hospitalization.
In conclusion, of the several differential factors between COPD patients with or without previous hospitalization, ER visits in the previous year, BODE index score and oxygen saturation levels are all variables that are significantly and independently associated with hospitalization due to COPD exacerbation. We propose two models that help to identify the most severe patients who are susceptible to being hospitalized due to an exacerbation with similar diagnostic reliability, allowing for modifications in the therapeutic approach in order to try to prevent hospital admittance.
FundingThis study has been made possible thanks to the unrestricted research aid provided by GlaxoSmithKline to the InCOPD group.
Conflict of InterestsThe authors declare having no conflict of interests.
Please cite this article as: Alcázar B, et al. Factores asociados a la hospitalización por exacerbación de la enfermedad pulmonar obstructiva crónica. Arch Bronconeumol. 2012;48:70-6.