The spectrum of presentation of SARS-CoV-2 disease (Covid-19) severity is very broad, ranging from asymptomatic infection to pneumonia that can progress to acute respiratory distress syndrome.1 To date, numerous series of patients admitted to hospitals have been described and certain factors are known to be associated with higher severity.2,3 However, there is still little information in Spain on the course of consecutive patients and factors related to hospital admission versus outpatient management.
In order to explore this area in greater depth, we retrospectively reviewed the first consecutive patients diagnosed with Covid-19 in our province (population: 329,587 inhabitants), selected from the complete list of subjects with confirmed SARS-CoV-2 infection. According to the protocol, patients with no initial symptoms of alarm (confusion, dyspnea, chest tightness) but older than 60 years, pregnant, or with comorbidities were included in a telehealth program (including daily O2 saturation monitoring) managed by a hospital team, and the rest were followed by telephone by their primary care physicians. Patients were referred to the hospital if they showed clinical deterioration during follow-up. The general criteria for admission were pulmonary infiltrates, O2 saturation < 95%, respiratory rate > 25 bpm, confusion, hemodynamic instability, or clinical severity at the discretion of the attending physician. The existence of stable comorbidities was not a criterion for admission per se.
Patients were included in the study if they were followed up for at least 15 days after diagnosis.
Results are expressed as mean ± standard deviation or number of observations (%). Groups were compared using the Mann-Whitney test for quantitative variables, and X2 for qualitative variables. Cox univariate and multivariate analyses were performed (dependent variable: hospital admission).
A total of 506 subjects were included from March 9th to 31st, 2020. Fewer men presented infection (187; 36.9%) than women (319; 63.0%) (P < .0001). Mean age: 56.0 ± 17.6 years (range: 12–93). Follow-up time: 18.7 ± 5.4 days. After the first evaluation, 94 patients (18.5%) were admitted. Initial mean SpO2 was 90.9 ± 0.7%. The remaining 412 subjects were followed as outpatients. SpO2 was available in 53.4% of these cases (96.1 ± 0.14%). Of those followed on an outpatient basis, 20 individuals were subsequently admitted (4.8% of this group). Four others died at home after admission was ruled out: 3 were ≥88 years old and had cancer or dementia; the fourth was receiving palliative treatment for incurable cancer. The subjects admitted were older than those treated as outpatients (70.0 ± 12.8 vs. 51.7 ± 16.5 years, P < .0001), were more often men (51.7% of those admitted vs. 32.3% of outpatients, P < .0001) and more frequently had comorbidities (85.0% vs. 40.8%, P < .0001). Comorbidities with different prevalences in inpatients vs. outpatients were arterial hypertension (58.7 vs. 20.6%, P < .0001), diabetes (36.8 vs. 8.4%, P < .0001), heart disease (23.6 vs. 4.0%, P < .0001), dyslipidemia (50% vs. 17.3%, P < .0001), cancer (7.0 vs. 2.2%, P = .02), and renal failure (4.3 vs. 0.7%, P = .02). Other comorbidities recorded with low prevalence (< 5%) and no differences between groups were: sleep apnea syndrome, rheumatoid arthritis, dementia or psychomotor retardation, peripheral arterial disease, multiple sclerosis, Crohn disease, and bronchiectasis. Asthma was reported in 7.8% of admitted patients and 4.5% of outpatients (P = .25) and COPD was reported in 3.5% and 1.5%, respectively (P = .34).
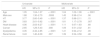
Table 1 shows the results of the Cox analysis. Variables that were significantly different in both groups were included. Age was coded in 1-year increments, and the remaining variables were dichotomized. In the multivariate analysis, age and diabetes were independently associated with admission.
Cox proportional risks, univariate and multivariate analyses for hospital admission risk.
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P | HR | 95% CI | P | |
| Age | 1.05 | 1.04–1.07 | < .0001 | 1.04 | 1.02–1.06 | < .0001 |
| Male sex | 1.88 | 1.30–2.70 | .0008 | 1.45 | 0.98–2.14 | .06 |
| HT | 3.77 | 2.60–5.49 | < .0001 | 1.37 | 0.88–2.11 | .15 |
| DM | 3.83 | 2.61–5.62 | < .0001 | 1.81 | 1.17–2.78 | .007 |
| Heart disease | 4.06 | 2.63–6.27 | < .0001 | 1.11 | 0.67–1.83 | .68 |
| Cancer | 2.65 | 1.29–5.43 | .008 | 1.09 | 0.51–2.32 | .81 |
| Dyslipidemia | 3.35 | 2.32–4.85 | < .0001 | 1.41 | 0.94–2.12 | .09 |
| Renal failure | 3.43 | 1.40–8.39 | .007 | 1.39 | 0.54–3.58 | .48 |
HT: hypertension, DM: diabetes mellitus.
Patients admitted for Covid-19, older age, male sex, and comorbid conditions have been associated with more severe disease.4 In our series of consecutive patients, 80% of the cases were followed up as outpatients, and less than 5% needed admission. The variables associated with admission were also higher age, male sex, and comorbidities. These data suggest that profiles of patients who do not present with immediately severe disease may be established. Thus, candidates may be selected for outpatient follow-up, and the intensity of the follow-up required may be graded, with a less specialized level of care being implemented in younger subjects without comorbidities. The results of the multivariate analysis suggest that diabetes may be particularly relevant for closer follow-up, but this analysis must be interpreted prudently because the study might not have sufficient statistical power.
Our study has some strengths, such as the inclusion of consecutive patients, and the availability of a unified electronic history that allows access to reliable data on the study variables. Several limitations must be highlighted. The retrospective design implies a risk of information bias. Despite including consecutive subjects, the gender distribution is not in line with the data published in the National Epidemiological Surveillance Network report available at the time of the analysis (52.2% women, 47.8% men),5 and may reflect a selection bias (inclusion of a high percentage of health workers or caregivers). Our data also come from a health area that has experienced relatively low hospital pressure, so the admission criteria may differ from other areas or epidemiological situations with higher case saturation. This, or a different prevalence of comorbidities in other areas, would plausibly limit the generalization of our results. This study, then, is a preliminary description of a care model of patients with SARS-CoV-2 infection which could serve to guide other teams in the future design of patient follow-up programs or the implementation of referral criteria between care levels during the pandemic.
Conflict of interestsThe authors declare that they have no conflict of interests related with the contents of this manuscript.
Please cite this article as: Golpe R, Blanco N, Castro-Añón O, Corredoira J, García-Pais MJ, Pérez-de-Llano LA, et al. Factores asociados al ingreso hospitalario en un protocolo asistencial en COVID-19. Arch Bronconeumol. 2020;56:676–677.