Although most lung abscesses communicate with the tracheobronchial tree, direct visualization of the necrotic cavity is uncommon. We present two cases were this bronchoscopic perspective was possible.
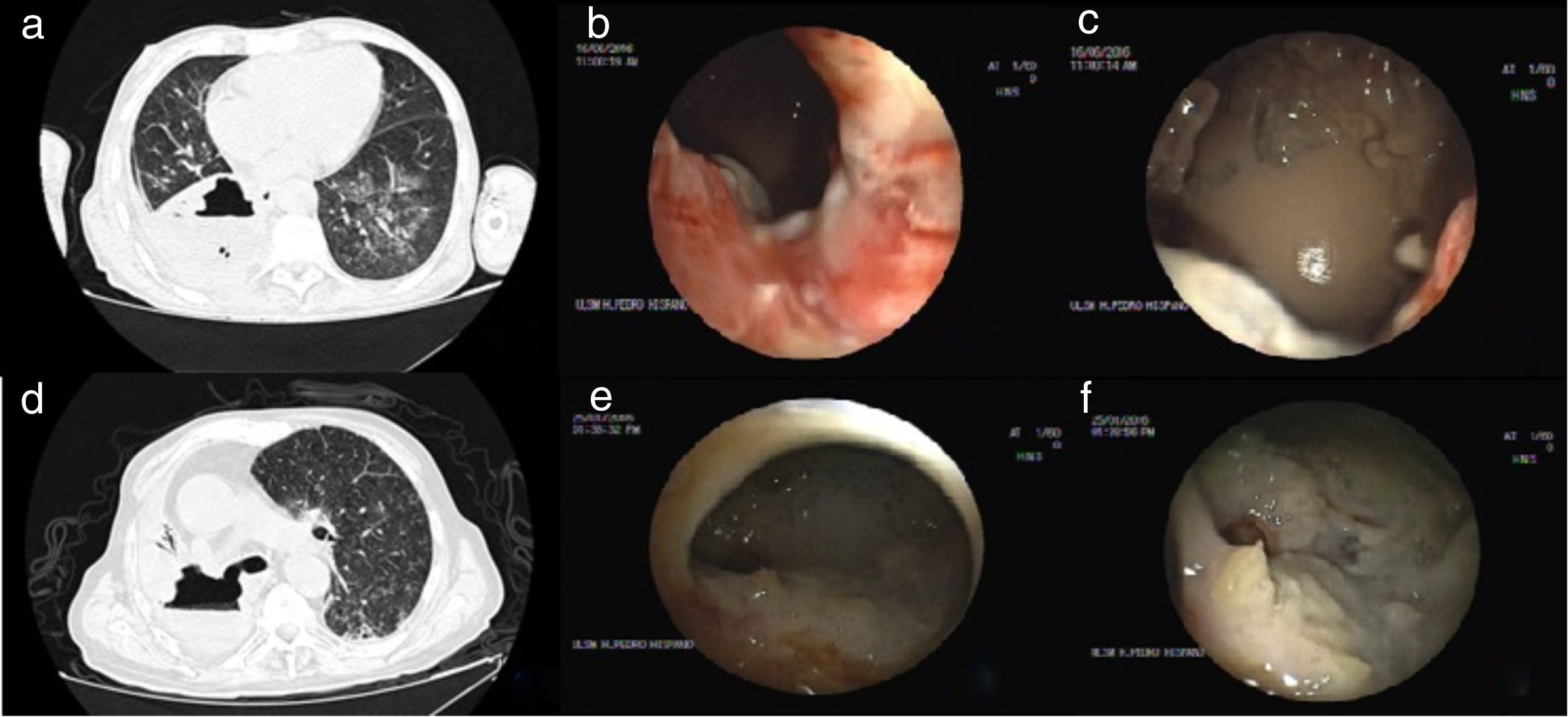
A 64-year-old male with previously treated oral squamous-cell carcinoma and dysphagia, under broad-spectrum antibiotics for an abscess on the right lower lobe(a); bronchoscopy revealed complete necrosis of the basal segments (B8-B10) throughout a bronchopulmonary fistula(b•c).
A 74-year-old male with stage IIIB lung squamous-cell carcinoma with extensive necrosis of the right upper lobe(d); bronchoscopy showed an obstructive tumoral infiltration of the right main bronchus with fistulization through the lateral wall to the necrotic cavity(e•f).
No microbiological isolation occurred in both cases. Considering their low impairment status, no other therapeutic approach was considered and the patients died after a month under antibiotics (Fig. 1).
Obstruction (tumour, foreign body), erroneous microbiologic diagnosis (mycobacteria), large abscesses and nonbacterial causes (vasculitis, pulmonary sequestration) can result in antibiotic failure. In this setting, bronchoscopic drainage via endobronchial catheter has emerged as a therapeutic option in those who are not eligible for surgery, in abscesses without an air-fluid level (cavity under high tension and risk of sudden endobronchial decompression) or if risk of massive hemoptysis (especially in hemodynamically unstable patients)1,2.