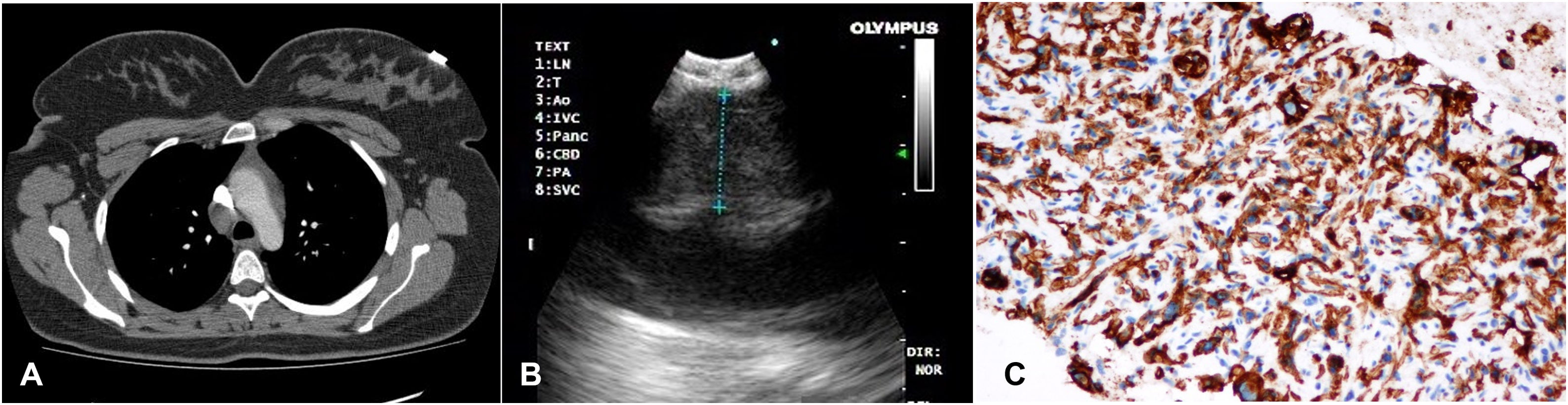
A 30-year-old female patient referred to our clinic because of the opacity located on the right lower paratracheal region, diagnosed on postero-anterior chest X-ray. She presented with complaints of chronic dry cough and weight loss. Thorax computed tomography revealed a lymphadenopathy with 20mm×15mm in length on the right lower paratracheal region (Fig. 1A). 18F-FDG (flourodeoxyglucose) PET-CT (Positron Emission Tomography-Computed Tomography) imaging revealed intense FDG-uptake value (SUVmax) with 8.7 on the lesion located at the region of 4R lymph node station (lower paratracheal region). We performed endobronchial ultrasound (EBUS) and transbronchial needle aspiration (TBNA). We visualized a well-circumscribed, round shaped, hypoechogenic lesion with the diameter of 11.6mm that was compressing the vena cava superior (Fig. 1B). Immunohistochemistry examination revealed the mesenchymal tumour cells to be strongly positive for vimentin and CD34 (Fig. 1C). Ki67 proliferation index was determined as 5%. No lymphoid cells were observed on microscopic examination. Patient was diagnosed with epithelioid hemangioendothelioma of the superior vena cava. Surgery was recommended to the patient, but she did not accept the operation.
Computed tomography showed a right lower paratracheal lesion (A), endobronchial ultrasound revealed a well-circumscribed, round shaped, hypoechogenic lesion with the diameter of 11.6mm compressing the vena cava superior (B), and immunohistochemical examination showed diffuse expression of CD34 (C).
Epithelioid hemangioendotheliomas usually originate from angioendothelial cells in different anatomical regions (such as the liver, lung, bone, etc.).1 Clinical behaviour of this neoplasm is defined as intermediate between benign hemangiomas and malignant angiosarcomas.2 Involvement of the vena cava is a very rare site for primary tumour. To our knowledge, this is the first case report of epithelioid hemangioendothelioma of the vena cava superior that was diagnosed with EBUS-TBNA.