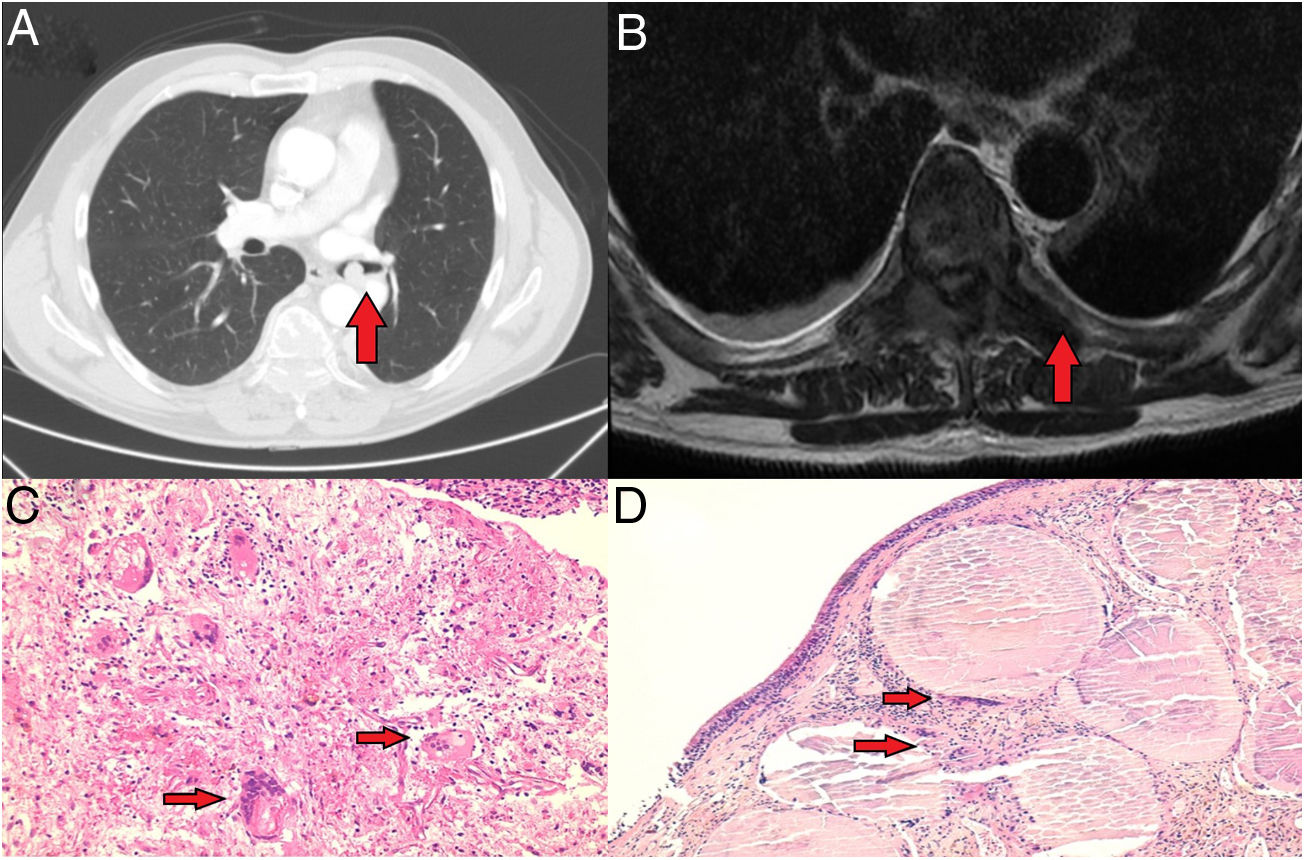
A 60-year-old male patient under study for loss of muscle strength in the lower limbs and advanced asthenia with the presence of hypoaesthesia of the L5 territory of the right lower limb. Computed axial tomography and magnetic resonance imaging requested as a complementary study revealed the presence of a 10.5mm×11mm endobronchial nodular lesion in the left main bronchus (Fig. 1A), as well as the existence of a pathological fracture in the D11 vertebral body and a hyperinflating lytic lesion in the D7 vertebra, with partial infiltration of its posterior elements and edema of the adjacent prevertebral soft tissues (Fig. 1B).
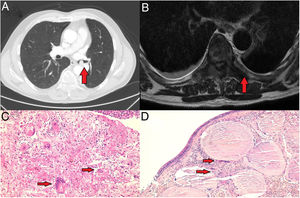
(A) 10.5mm×11mm endobronchial nodular lesion located in the left main bronchus. (B) Hyperinflating lytic lesion in the D7 vertebra, with partial infiltration of its posterior elements and edema of the adjacent prevertebral soft tissues. (C) Soft tissue biopsy (×20): multinucleated giant cells (red arrows) loosely distributed along with numerous mononuclear cells in a fibrous background (×20 magnification). (D) Bronchial mucosa (×10): atypical cell proliferation located at the level of the submucosa composed of soft-looking mononuclear cells, multinucleated giant cells (red arrow) and formation of metaplastic bone tissue (red arrow).
A bone and soft tissue biopsy was performed at location D7 for histological study (Fig. 1C), as well as decompression by arthrodesis D5-L1 and therapeutic rigid bronchoscopy with excision of the excrescent hypervascularized and friable lesion in the distal lateral wall of the left main bronchus, which caused a 60% stenosis of the bronchial lumen undergoing histological study (Fig. 1D) compatible with giant cell tumor metastasis of bone tissue. The patient received treatment with denosumab, with good tolerance, achieving tumor stability and absence of endobronchial recurrence and spinal radiotherapy (D7–8 and D11) of 20Gy in 5 sessions with good tolerance and clinical improvement.
The patient was diagnosed with a vertebral giant cell bone tumor (GCT) with endobronchial metastatic involvement. Said neoformation is considered a locally aggressive, benign neoplasm composed of cytologically banal, oval or polyhedral mononuclear cells, mixed with numerous evenly distributed giant cells similar to osteoclasts. They constitute 5% of primary bone tumors and generally affect the epiphyseal–metaphyseal region of long tubular bones, infrequently occurring in the spine. GCT incidence is higher between the third and fifth decade of life, with a slightly greater affectation in women. Its incidence in childhood is exceptional.1
GCT is a tumor with a generally benign behavior, infrequently causing metastasis or death. The presence of metastases in the bone, in the form of highly infrequent pathological fractures, and in the lung occurs between 1.8% and 9.1% when the tumor is located in the epiphyseal–metaphyseal region of long tubular bones and up to 13.5% if it is located in the spinal column. When there is lung involvement, the tumor loses its benign condition, reaching a mortality rate of 14–25%.2
Among the possible causes of coexisting pulmonary and bone lesions, we must assess the existence of pulmonary neoplasia with bone metastases, which occur in up to 40% of patients with lung cancer.3 Other neoplasms that frequently also present metastatic involvement at the lung and bone level are breast and prostate neoplasms, and it is important to include them in the differential diagnosis.4,5
In conclusion, although very infrequent in healthcare practice, the possibility of a giant cell bone tumor must be considered within the differential diagnosis in patients with lung and bone lesions.
FinancingThis work has not received any funding.