Empyema necessitatis is a rare complication of pleural infections treated late or inadequately. It is characterized by pus spreading from the pleural cavity through the underlying tissues to form an abscess in the chest wall that sometimes even forms a skin fistula.1,2 Most cases are caused by Mycobacterium tuberculosis infection, although it has also been described, albeit less frequently, in association with other microorganisms such as Streptococcus pneumoniae, Staphylococcus, Gram-negative bacilli and polymicrobial infections.1 We report a case of empyema necessitatis caused by Corynebacterium jeikeium. Treatment was complex but exclusively medical, and to our knowledge this is the first case with these characteristics described in the literature.
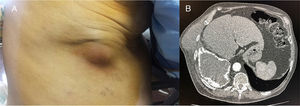
Our patient was an 84-year-old man with a history of pulmonary tuberculosis (TB) at the age of 20 years, treated with collapse therapy. He consulted due to a painful swelling in the right lower hemithorax in the upper quadrant of the abdomen, accompanied by dyspnea, non-productive cough, and fever of 38.2°C. Of note on examination was an erythematous, swollen, painful area in the lower axillary mid-line, measuring 8cm (Fig. 1A). Signs of right pleural effusion were detected on auscultation. Chest X-ray showed right pleural effusion encapsulated with extensive fibrothorax and loss of volume with an image of a calcified outer surface, measuring about 14×8cm, and bronchiectasis. Chest CT revealed a pleural collection with a calcified outer shell, air-fluid level, and a soft tissue lesion in the lower chest wall measuring 8.2×7cm, containing fluid. The lesion extended through the intercostal space to the right subphrenic region (Fig. 1B). Communication was identified between the most posterior and anterior area of the fibrothorax and the described mass. Fiberoptic bronchoscopy (FB) ruled out bronchopleural fistula. Both collections were drained by incision and evacuation of the purulent material from the abscess in the chest wall, and a 22F chest tube was placed, with total drainage of 2400ml of pus. Urokinase was instilled every day and the abscess was packed for healing by secondary intention. Serial cultures of pleural fluid and FB specimens were negative for mycobacteria, and aerobic and anaerobic bacteria. The patient was treated with amoxicillin-clavulanic acid, initially intravenously and then orally for a total of 3 months, after which he remained asymptomatic. Radiological monitoring showed resolution of the pleural effusion, disappearance of the fibrothorax, and cure of the skin abscess. Seven months later, the patient presented spontaneously due to general malaise and recurrence of the skin abscess, although it was smaller in size than the initial lesion. X-ray confirmed relapse of the empyema. Thoracentesis retrieved pus with similar characteristics and an aerobic, Gram-positive, catalase-positive bacteria identified as C. jeikeium was grown on culture. Susceptibility testing showed a multiresistance pattern, with susceptibility to erythromycin, vancomycin, and clindamycin only. A Veress needle was used to drain 800ml from the pleural cavity and local abscess care was given. After outpatient treatment with clarithromycin 1g/24h and clindamycin 300mg/8h, the patient's clinical and radiological situation had resolved and hospital admission was not required.
Empyema necessitatis is a rare complication that occurs when pleural empyema spreads to form an abscess in the chest wall, penetrating the adjacent tissues and forming a skin fistula. It occurs most frequently in the subcutaneous tissue of the chest wall, between the clavicular and the anterior axillary mid-lines,3 although it has also been described in the esophagus, paravertebral soft tissue, retroperitoneum, pericardium, and groin. Empyema necessitatis was already a rare complication (10%) in the days before antibiotics. Up to 75% of the cases were caused by M. tuberculosis,1 although it only grows in 10%–40% of cultures.1 Other causes described less frequently are pyogenic infections (Staphylococcus aureus, S. pneumoniae, Gram-negative bacilli), actinomycosis, cancers,1,2,4 or complications after chest injuries,3 pneumonectomy, or thoracoplasty.5 Clinical and radiological suspicion are essential. CT is useful for confirming the diagnosis and for evaluating communication of the collection with the pleural space through the chest wall and revealing, as in our case, an extrapleural mass in the chest wall, in addition to the findings in the pleural cavity. Chest ultrasound is also useful for evaluating both the lesions and their progress, while avoiding unnecessary irradiation. C. jeikeium is a Gram-positive aerobic bacteria that on rare occasions causes opportunistic infections.6 Cases of bacteremia, septicemia, endocarditis, and osteomyelitis have been described, but this is the first report of this microorganism causing empyema necessitatis.
Although the standard treatment of a chronic chest cavity infection, isolated from the rest of thorax, and with no chance of becoming occupied by lung parenchyma, should be open thoracostomy with intensive draining and healing by second intention, we treated our patient conservatively, given his advanced age and underlying disease.
Please cite this article as: Molina V, Arlandis M, Chiner E. Empiema necessitatis por Corynebacterium jeikeium: preguntas del s. xix, respuestas del s. xxi. Arch Bronconeumol. 2018;54:53–54.