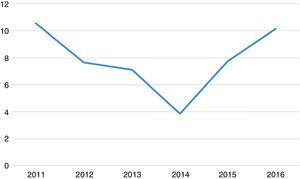
Streptococcus pneumoniae is one of the major microorganisms involved in community-acquired respiratory infections, including pneumonia, which may occur with pneumococcal bacteremia.1 The incidence of bacteremic pneumococcal infection is higher in certain groups of the population, particularly the elderly and patients with underlying debilitating diseases. This severe invasive presentation is associated with high mortality.2 The inclusion of antipneumococcal vaccination in European immunization programs and the selective pressure of antibiotics on the circulating strains have produced changes in the incidence and epidemiology of the disease.3 Recent years have seen a re-emergence of strains of S. pneumoniae resistant to penicillin and other antimicrobial agents, making these infections difficult to treat and complicating the prognosis. The main limitation of the 23-valent polysaccharide vaccine (PPSV23) is that it has shown no significant effect on the risk of developing bacteremic pneumococcal pneumonia (BPP).4 The impact of the 13-valent conjugate vaccine (PVC13) on bacteremia and other invasive forms of pneumococcal disease in adults is still under evaluation.4 In this paper, we describe the epidemiological characteristics and predictors of mortality in patients with a diagnosis of BPP, and the antimicrobial resistance profile and distribution of serotypes of the isolated strains. All patients older than 14 years diagnosed with pneumonia and positive blood culture for S. pneumoniae during the period 2011–2016 were selected. In total, 159 episodes of BPP in 159 patients were included. Distribution by sex was 100 (62.9%) men and 59 (37.1%) women. Mean age was 75 years (IQR: 59–85); 73% patients showed a minimum inhibitory concentration (MIC) ≤0.06 for penicillin and 94% showed an MIC ≤1 for cefotaxime. As for other antimicrobials, 8% were resistant to levofloxacin, 27% to erythromycin, and 20% to clindamycin. Twenty-eight percent of the clindamycin-resistant strains showed an inducible resistance pattern. Serotypes were determined in 158 strains, and up to 33 different serotypes were identified. The most frequent were serotypes 3 (16%), 19A (11%), 14 (8%), 22F (7%), 19F (5%), 6C (4%) and 12F (4%). The group of strains with serotype 19A was of particular interest, as they showed a high rate of resistance to each of the antibiotics studied: 67% had a MIC >2 for penicillin, 70% had an MIC >1 for cefotaxime, and 33%, 28% and 31% of the strains were resistant to erythromycin, clindamycin, and levofloxacin, respectively. Mean incidence of BPP was 7.8 cases per 100000 inhabitants/year (range: 3.9–10.6) (Fig. 1). In total, 72% of patients had an underlying disease, such as diabetes, heart disease, cancer, respiratory disease, immunosuppression, among others. Overall in-hospital mortality was 23%. Risk factors significantly associated with mortality were age ≥65 years (OR: 3.13; 95% CI: 1.21–8.07; P=0.02), heart disease (OR: 2.61; 95% CI: 1.09–6.25; P=0.03), and cancer (OR: 3.13; 95% CI: 1.35–7.25; P=0.01). Despite the aging of the population and the increase in life expectancy of patients with debilitating diseases, we did not observe a significant variation in the incidence of BPP between the beginning and the end of the study period. The number of strains in which penicillin resistance was detected (27%) is similar to figures published in the literature.5 In our population we are unaware of vaccination rates with PCV13 and PPV23, but PPV23 vaccination in the adult population (>60 years) in Spain ranges between 52.5% and 66%.6,7 Despite this, serotype 19A, included in the PPV23 and PCV13 vaccines, was the second most common, and the one that was most frequently associated with multiresistance. In our series, we found no association between mortality and the different serotypes, due probably to a type II error. BPP mortality ranges from 13% to 16%, and is higher in certain population groups, such as the elderly, who present mortality rates of 22%–51%.8 The high mortality rate found in our study (23%) may be due to the high proportion of elderly patients with comorbidities in our series.
Please cite this article as: Galán-Ros J, Escudero-Jiménez Á, Solves-Ferriz V, Escribano Garaizábal E. Neumonía neumocócica bacteriémica en el adulto. Arch Bronconeumol. 2018;54:54–55.