Emphysematous cystitis (EC) is an uncommon complication of urinary tract infection, defined by the presence of gas in the bladder and/or bladder walls.1 It mainly affects elderly women with diabetes mellitus, poor blood glucose control, and a history of bladder catheterization. Other factors, while less important, may also be associated with this disease, such as renal transplantation, immunosuppression, and recurrent urinary tract infections.1 The most commonly isolated causative pathogens on urine culture are Escherichia coli, Klebsiella pneumoniae and Enterococcus.2 Clinical presentation is non-specific but most patients present urinary symptoms and abdominal pain. Pneumaturia is a key but infrequent pointer to suspecting EC.3 For diagnosis, standard radiography of the urinary tract is unspecific, and the superior resolution and greater ability of computed tomography (CT) to rule out other causes of EC, such as enterovesical fistula due an inflammatory or malignant process, make it the examination of choice.4 Initial treatment consists of empirical antibiotics, intensive metabolic control, and urinary diversion (transurethral catheterization or bladder drainage).5 The clinical response of patients varies from rapid clinical improvement to general deterioration with a high rate of complications, such as emphysematous pyelonephritis, bladder perforation, septic shock, and rapid death.5
We report the unusual case of a male patient, non-diabetic, with normal blood glucose levels and no significant urological history, who presented EC during admission to the pulmonology ward for a severe COPD exacerbation caused by infection. E. coli was cultured from both sputum and urine samples. Our patient was a 66-year-old man, retired from employment in an iron foundry, who had given up smoking 5 years previously (70 pack-years). He had a history of childhood tuberculosis, arterial hypertension, moderate COPD, non-exacerbator emphysematous phenotype (GOLD category A) and, 5 years previously, community-acquired pneumonia. He reported a 5-day history of clinical symptoms of infection, with rhinorrhea, increased cough with purulent sputum, dyspnea, and fever 38.3°C. He had no urinary symptoms and no changes in bowel habits. He also showed overall acute respiratory failure, with left-shift leukocytosis and increased PCR on clinical laboratory tests. Blood glucose was normal. Urine antigen testing for pneumococci and Legionella and sputum culture were performed, which were negative. The physical examination showed significant deterioration of the patient's general status, with tachypnea, and disperse rhonchi on lung auscultation. No signs of abdominal disease were observed at that time.
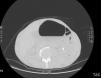
On day 3 of admission, the patient's clinical situation deteriorated, with symptoms of urinary infection (tenesmus, dysuria, and hematuria). An examination of urinary sediment was requested, showing abundant red blood cells per field and positive nitrites. Gram-negative antibiotic cover was administered, and urine culture was requested, which was positive for E. coli, so piperacillin–tazobactam was given, in line with the microbiological sensitivity results. A chest-abdominal computed tomography was performed to complete the study, revealing gas in the bladder lumen, infiltrating the walls (Fig. 1). After diagnosing EC, and following consultations with the urology department, we introduced a bladder catheter, obtaining 400ml of urine with a slightly hematic tinge and abundant air. Intravenous piperacillin–tazobactam was also initiated and continued for 15 days. The urine culture was repeated after the antibiotic cycle, and results were negative. The bladder catheter was removed and the patient's abdominal symptoms resolved. Despite the initial improvement, respiratory symptoms persisted with purulent expectoration, and a repeat sputum culture was again positive for E. coli that showed intermediate sensitivity to piperacillin–tazobactam, so antibiotic therapy was switched to intravenous meropenem. The patient finally showed satisfactory progress, and after completing the intravenous treatment regiment, he was discharged with subsequent follow-up by the respiratory medicine department.
Our thanks to the Functional Examination Laboratory of the Hospital Universitario Cruces.
Please cite this article as: Rodríguez López DP, Marina Malanda N, Salinas Garrido I, Gáldiz Iturri JB. Cistitis enfisematosa y agudización infecciosa de la EPOC. Un hallazgo altamente infrecuente. Arch Bronconeumol. 2017;53:406–407.