More than forty percent of patients with pectus excavatum have a family history of chest deformity. However, no studies of the frequency of the different phenotypes of pectus excavatum have been published.
MethodsA random sample of 300 non-syndromic pectus excavatum patients, from the chest wall deformities clinic at Children's Hospital of The King's Daughters in Norfolk, VA, was studied and classified according to a previously described classification system. Photographs and computed tomography (CT) scans were utilized.
ResultsTypical pectus excavatum. Photo data: localized deep depression (cup-shaped) deformity occurred in 67%; diffuse (saucer-shaped) 21%, trench-like (furrow-shaped) 10%, and Currarino-Silverman (mixed pectus excavatum/chondromanubrial carinatum) 1%. The deepest point was to the right of midline in 80%, left in 10% and central in 10%. As per the photograph, the deepest point was in the lower sternum in 75%. When asymmetric, the deepest point of the deformity was to the right of midline in 90%. CT data: the average Haller index was 4.9. Severe sternal torsion (>30°) was associated with greater Haller index (6.3) than mild torsion (4.5). The deepest point of the depression was at the mid- or lower sternum in more than 99%. It proved impossible to estimate width or length of the depression because of poorly defined borders.
ConclusionsTypical PE is cup-shaped in 67% of cases, to the right of the midline in 80%, and involving the mid-to-lower sternum in 99%. However, other phenotypes, like the saucer and long trench, comprised one-third. Definition of the deformity is more reliable by CT scan.
Más del 40% de los pacientes con pectus excavatum tienen antecedentes familiares de una deformidad torácica. Sin embargo, no se han publicado estudios de la frecuencia de los diferentes fenotipos de pectus excavatum.
MétodosSe estudió una muestra aleatoria de 300 pacientes con pectus excavatum no sindrómico de la clínica de deformidades de la pared torácica del Children's Hospital of the King's Daughters de Norfolk (Virginia, Estados Unidos) y se clasificó a los pacientes según un sistema descrito con anterioridad. Se utilizaron para ello fotografías e imágenes de tomografía computarizada (TC).
ResultadosPectus excavatum típico. Datos fotográficos: se observó una deformidad con depresión profunda localizada (forma de taza) en el 67% de los casos, difusa (en forma de platillo) en el 21%, de tipo trinchera (en forma de surco) en el 10%, y de tipo Currarino-Silverman (deformidad mixta de pectus excavatum/pectus carinatum condromanubrial) en el 1%. El punto más profundo se encontraba a la derecha de la línea media en el 80% de los casos, a la izquierda en el 10% y en el centro en el 10%. En las fotografías, el punto más profundo se encontraba en la parte inferior del esternón en el 75% de los casos. Cuando había asimetría, el punto más profundo de la deformidad estaba a la derecha de la línea media en el 90% de los casos. Datos de TC: la media del índice de Haller fue de 4,9. La torsión esternal intensa (>30 grados) se asoció a un índice de Haller más alto (6,3) que el observado en la torsión leve (4,5). El punto más profundo de la depresión se encontraba en la parte media o baja del esternón en más del 99% de los casos. Resultó imposible estimar la anchura o la longitud de la depresión, ya que los límites estaban mal definidos.
ConclusionesEl pectus excavatum típico tiene forma de copa en el 67% de los casos, se encuentra a la derecha de la línea media en el 80% y afecta a la parte media o baja del esternón en el 99%. Sin embargo, otros fenotipos, como el de forma de platillo y el de trinchera larga, constituyeron una tercera parte del total. La definición de la deformidad es más fiable mediante la TC.
Pectus excavatum is the most common chest wall anomaly. It affects one in every 400 newborns in the United States,1 and is characterized by depression of the anterior chest wall and sternum. Impaired cardiac and lung function has been widely described in patients with severe deformities,2 and the chest deformity causes body image issues in affected individuals. Although more than 40% of our patients report a family history of chest wall deformities,3 the etiology of the disorder remains unknown.
With increasing clinical experience, we were able to present a classification of the dysmorphology of pectus excavatum.4 We have conducted collaborative genetic studies on this disorder, which showed that inheritance occurs via different pathways in different families: autosomal dominant, autosomal recessive, X-linked and complex hereditary patterns have been observed.5
Genetic analysis attempts to establish a correlation between genotype and phenotype.6 Previously, both we and other authors7 have described several variants of typical pectus excavatum morphology. However, its frequency has not been reported, which is the object of this study. We also hoped to facilitate the genetic study by classifying those variants that did not occur in our clinical practice frequently enough to be able to present them reliably.
Materials and MethodsA random sample of 300 pectus excavatum patients, treated surgically at the Children's Hospital of The King's Daughters Eastern Virginia Medical School, Norfolk, VA, U.S.A. (CHKD/EVMS, U.S.A.) was studied and classified. The study was approved by the Eastern Virginia Medical School internal ethical review board (number 01-05-EX-0175). Three hundred patients were selected to ensure that the study could be evaluated in detail within an acceptable time frame, and to have a group that was large enough to encompass the variety of morphologies observed in the cohort of over 2300 patients in this unit. Patients with Ehlers–Danlos, Marfan or other genetic syndromes were excluded from the study, as were patients with complications due to comorbidities, such as congenital heart disease or congenital diaphragmatic hernias, and those with a previous history of thoracic surgery. There was no attempt to correlate other pathologies, the frequency or time evolution of a particular morphology.
Medical records, preoperative photographs and computed tomography (CT) images of 300 patients of both sexes with identified pectus excavatum were examined retrospectively, with special attention paid to the defining characteristics identified in our previous study: Haller index, asymmetry index, relative length of the depression with respect to the sternum, fraction of sternum affected, degree of sternal torsion and localized (cup-shaped), diffuse (saucer-shaped), trench-like or Currarino morphology.4 A total of 17 CT scans were considered unsuitable, leaving 283 patients for the study.
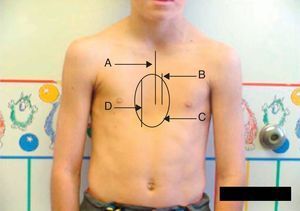
Eighty percent of patients were male. They were aged between 4 and 30 years at the time of the CT scan; the median age was 14.5 years. Minimally invasive repair of the pectus excavatum was performed in all the cases (Nuss procedure). Two staff surgeons (DN and RK) separately evaluated the preoperative photographs taken at the clinic and CT scans of each patient. In the photographs they examined: the shape of the deformity (cup-shaped, saucer-shaped, trench-like or Currarino),8 the position of the center of the depression (to the right, center or left of the midline), the upper, mid- or lower sternum, the length of the depression expressed as a fraction of the apparent sternal length, the symmetry of the depression (do the sides of the depression have a similar slope, or does one side have a steep slope and the other a slight, long slope?) and the presence of a winged or bell-shaped thorax (anterior protrusion of the inferior costal cartilage) (Fig. 1). These characteristics were chosen because they were significant morphological observations in a previous study of our large reference group.4
Information on the protocol used to show the morphology in the preoperative photograph of the patient. (A) Median/sternal line chest; (B) length of sternum affected; (C) area affected by depression; (D) vertical length of deformity. Note how the area is affected by the depression asymmetry to the right.
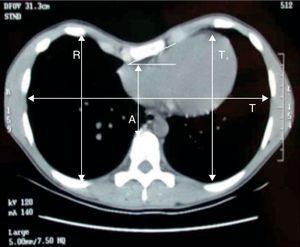
On the CT images, the deepest point of the depression, both in the craniocaudal and sagittal plane, symmetry (comparing the slope of both sides), length of the craniocaudal depression, sternal torsion (and whether this was greater or less than 30°), Haller index and asymmetry index were evaluated (Fig. 2). To this end, the methodology in our previous study was strictly followed.9 Most of the CT scans were obtained before digital imaging techniques became available, and the measurements were done manually. The radiologic assessment was not examined.
Since the majority of patients at CHKD/EVMS come from outside our area, most of them were selected initially based on their place of residence. Thus, we see a large number of patients with “typical” pectus excavatum.
Other rare variants such as the well-known laterolateral juxtaposition of pectus excavatum and pectus carinatum, were not included in the random sample or in the analysis.
ResultsTypical Pectus ExcavatumPhotographic DataLocalized deformity (cup-shaped) (Fig. 3) occurred in 67% of cases; diffuse (saucer-shaped) (Fig. 4) in 21%, trench-like (furrow-shaped) (Fig. 5) in 10%, and Currarino-Silverman (mixed pectus excavatum and carinatum) (Fig. 6) in 1%. The deepest point was to the right of the midline in 80% of patients, to the left in 10% and central in 10%. The deepest point of the depression was in the mid- or lower sternum in more than 99% of cases. Although the depression was to the right of the sternum in 80% of patients, the slope and shape of the sides of the depression were symmetrical in 67% of all cases. However, in patients in whom the shape of the deformity was asymmetric, this was centered to the right of the midline in 90% of cases (Tables 1 and 2). The sex and age of the patient did not seem to influence the distribution of the different forms. Measurements for craniocaudal length of the depression and thoracic widening based on examination of the photographs were unreliable.
The mean Haller index was 4.9. The presence of severe sternal torsion (>30°) was associated with a higher Haller index (6.3) than that was observed in mild torsion (Haller 4.5). The deepest point of the depression was in the mid- or lower sternum in more than 99% of cases. The previously described symmetry index (R/L×100%) was an average of 99%, which implies symmetry, but in this study it was observed that this index did not really represent the true configuration of the chest with respect to its symmetry. The assessments performed by the different observers were notably uniform in the CT images. As two-dimensional horizontal CT sections were used, the definition of the cranial and caudal borders of the depression was imprecise.
Rare variants of pectus excavatum presented were the mixed form of pectus excavatum and carinatum, bilateral depressions and focal depressions that affected areas of the chest other than the lower midline (Figs. 7–9).
DiscussionSurgical decision-making is affected by the type of pectus excavatum deformity presented by the patient when performing the Nuss procedure. Two bars are required in patients with trench-like dysmorphology. In many of the patients with a larger saucer-shaped pectus excavatum, placement of a second bar is also useful. Surgeons who use open surgery or the Ravitch procedure may have to perform additional resections of the costal cartilage and move the position of the sternotomy.
Recent treatment of a large number of patients with pectus excavatum has provided the opportunity to study its mode of inheritance. Family history is common in this disorder.2 A study of the family trees of 34 families in which there were two affected siblings showed that there was autosomal dominant inheritance in 41% of families, autosomal recessive in 12%, X-linked in 18% and complex inheritance patterns in the remaining patients (29%).5
Horth et al.10 evaluated 48 family trees with a total of more than 2000 individuals. These authors found clear evidence indicative of autosomal recessive, genetic control for this disorder. The proportion of males to females in their patients was 3.8–1, very similar to the 4:1 observed in our group. They considered that it was likely that there was more than one mutation responsible for the disorder. Although this group was able to evaluate 10 clinical features often associated with pectus excavatum (e.g. thin, tall, and long fingers), they were unable to correlate these characteristics with the phenotype.
The correlation of the genetic findings with the phenotype may be obtained by knowing the frequency of the phenotypes. In order to determine this frequency, 283 of the 1215 patients who had been previously diagnosed with a severe type of pectus excavatum and had been treated with a minimally invasive repair were randomly selected. Preoperative photographs and CT images were available for all the patients, and were used to classify them by applying the method described in 2006.4
The study limitations derive from patient selection that was not population-based. While we recognize this fact, the classification of patients with a typical deformity (a deformity that is severe enough to warrant an operation) has the value of a clear diagnosis. The exclusion of patients with Marfan syndrome and Ehlers–Danlos syndrome was necessary due to the difficulty of the definition. Of the 1215 patients presented in 2010, Marfan syndrome was identified in 2.8%, but there were features that were clearly suggestive of Marfan syndrome in an additional 17.8%, although there was no genetic confirmation of the diagnosis at the time of the preoperative evalation.3 Patients with Ehlers–Danlos syndrome were even less common.
ConclusionsThe most common type of pectus excavatum is cup-shaped, symmetrical, to the right of the midline, and involves the lower sternum. However, other phenotypes like the long trench, which extends much further in the cranial direction, were observed with significant frequency. Although photographs enable its shape to be examined, definition of the deformity is more reliable by CT scan.
Conflict of InterestsThe authors declare that they have no conflict of interests.
The authors would like to thank Erin McGuire for her work on the statistical analysis, and Trisha Arnel for administrative support.
Please cite this article as: Kelly Jr. RE, et al. Dismorfología de las deformidades de la pared torácica: distribución de frecuencias de los sub-tipos de pectus excavatum típico y subtipos poco comunes. Arch Bronconeumol. 2013; 49:196-200.
Presented on July 19–22, 2011 at the Congress of the British Association of Paediatric Surgeons in Belfast (Northern Ireland).