As cancer survival improves, the appearance of multiple tumors in a single patient is becoming more common. The aim of this study was to analyze long-term evolution, focusing particularly on disease recurrence and second primary tumors, in patients with lung cancer (LC) and ≥3 years overall survival.
Materials and methodsRetrospective study of 1769 patients with LC. A total of 218 (136 treated with surgery and 82 with other treatments), followed up for between 5 and 23 years were enrolled. LC progress and intercurrent diseases were recorded.
ResultsA total of 65 patients presented tumor relapse, of which 60.9% occurred in the first 3 years; 26 patients developed secondary primary tumors (84.6% after 5 years) and 24 developed 2 or more second extrapulmonary tumors (66.6% after 5 years), most of which were smoking-related. The incidence of second primaries was greater than the expected incidence of cancer in the general population matched for age and sex.
ConclusionThe multiple carcinogenic effect of smoking persists and manifests in various organs, more than 5 years after the diagnosis of LC, even in patients with long survival. After 5 years, a second tumor is more likely than a relapse of the primary disease, and the lung is the most common site of development of a second tumor.
Al mejorar la supervivencia del cáncer, la presencia de tumores múltiples en un paciente es cada vez más frecuente. El objetivo del estudio ha sido analizar la evolución a largo plazo, especialmente las posibles recidivas y segundos tumores primarios, en pacientes con cáncer de pulmón (CP) y supervivencia ≥3 años.
Material y métodosEstudio retrospectivo de 1.769 pacientes con CP. Se incluyen 218 (136 tratados con cirugía y 82 con otros tratamientos) con supervivencia global ≥3 años, de cualquier estirpe y seguidos durante un período entre 5 y 23 años. Se registró la evolución del CP y las enfermedades intercurrentes.
ResultadosUn total de 65 presentaron recidiva del tumor, de los cuales el 60,9% apareció en los 3 primeros años; 26 desarrollaron segundos primarios pulmonares (84,6% después de 5 años) y 24, 2 o más segundos extrapulmonares (66,6% después de 5 años), la mayoría relacionados con el tabaco. La incidencia de segundos primarios fue superior a la incidencia esperable de cáncer en población general de similar edad y género.
ConclusiónEl efecto carcinogénico múltiple del tabaco persiste y se manifiesta en diversos órganos después de pasados 5 años tras el diagnóstico de CP, incluso en pacientes que han tenido una larga supervivencia. Después de 5 años, un segundo tumor es más probable que una recidiva del primero y el pulmón es el órgano con mayor probabilidad de desarrollar un segundo tumor.
Of all malignant neoplasms, lung cancer (LC) causes the greatest number of deaths worldwide. Prognosis is poor, with 5-year survival rates of between 10% and 20% in most countries.1,2 For many years, the possibility of long-term survival was limited almost exclusively to patients who were candidates for complete surgical resection.3 However, in the last 25 years, new chemotherapy (CT) regimens combined with various thoracic radiotherapy (TRT) programs have been introduced, increasing favorable responses in patients with advanced locoregional disease, some of whom have achieved long-term survival.4–6 More recently, new drugs aimed at specific molecular targets have been developed for the treatment of selected LC subgroups with certain molecular and genetic features. These compounds have provided favorable and enduring outcomes in some stage IV patients,7 although there is still very little data available on 5-year life expectancy.
Late disease recurrence and second primary tumors (SPT) are relatively common among the small proportion of patients who achieve prolonged survival. Reports have been published on this topic in resected patients,8–12 but few have focused on the evolution of long-term LC survivors who did not receive surgery.13–15
In this study, we analyzed the evolution of our LC patients with ≥3 years’ survival, in order to determine the rate of recurrence and second tumors, and the times to these events.
Patients and MethodsThis was a retrospective study, in which we reviewed the clinical records of 1769 patients with LC diagnosed between 1991 and 2009 (both inclusive): 310 underwent resection with or without neoadjuvant or adjuvant treatment; 1009 received CT, TRT, or combined CT and TRT, and 450 received palliative care only.
In total, 218 patients with a cytohistological diagnosis of LC and overall survival ≥3 years (12.3% of those examined) were included, irrespective of treatment received. The following data recorded at the time of diagnosis were collected: age, sex, smoking habit, histologic type, TNM stage (IASCL 2009 classification), and treatment modality. In the follow-up period, patients with a diagnosis of LC were examined at least 3 times a year during the first 2 years and once a year after the third year. Patients who had received CT or TRT were seen more frequently during the first 2 years. Patients diagnosed before the end of 2009 were included, and the study was closed in December 2014, so the minimum follow-up period for survivors was 5 years. Intercurrent diseases occurring during this period were recorded, and in many cases the incidence of extrapulmonary cancers was retrieved from the records and electronic documentation held in other departments and specialist units, and from biopsy reports relating to other organs.
To differentiate between recurrence of the primary tumor and second primary pulmonary tumor (SPPT), we used the criteria of Martini and Melamed, with the interval proposed by Detterbeck,16,17 defining second primary tumor as: (1) different histologic type; (b) different lung site, in the absence of mediastinal node involvement; or (c) time to occurrence >4 years.17
The rate of recurrence and pulmonary and extrapulmonary SPTs are expressed in number of cases/100 person-years, for which the sum of the follow-up times until the last contact with each patient was computed. To evaluate their magnitude, these rates were compared with incidence rates of LC in the general population in our setting,18,19 thus providing an estimated relative risk. With regard to SPT rates, comparisons were made with figures from any Spanish region for which protocolized cancer population registries are available20 (to date, no such registries are available in our region). In view of the small number of women in our series, all comparisons were made with male populations only.
Statistical analysis: means were compared using the Student t-test. For comparison of percentages, the χ2 test was used.
Ethics committee approval: although this was an observational study, authorization was requested and obtained from the Ethics Committee of our hospital.
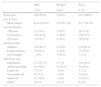
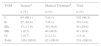
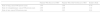
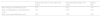
ResultsDemographic characteristics, smoking habit and histologic type of the 218 patients included with survival ≥3 years are shown in Table 1. Table 2 shows the distribution of TNM stages by therapeutic strategy: (1) surgery or (2) other treatment, namely: 20 patients received CT only, 3 received TRT only, 55 received a combination of CT and TRT, and 4 received palliative care only. The great majority of the surgical patients (n=136) were in stages I and II, in contrast to those who received medical treatment (n=84) – the latter group had more advanced tumors (Table 2).
General Characteristics of Lung Cancer Patients with Survival ≥3 Years.
| Men | Women | Total | |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Total cases | 204 (93.5) | 14 (6.5) | 218 (100.0) |
| Age in years | |||
| Mean (range) | 62.4 (39–85) | 57.6 (42–78) | 62.1 (39–85) |
| Age distribution | |||
| <50 years | 21 (10.3) | 5 (35.7) | 26 (11.9) |
| 51–69 years | 109 (53.4) | 7 (50.0) | 116 (53.2) |
| ≥70 years | 74 (36.3) | 2 (14.3) | 76 (34.9) |
| Smoking habit | |||
| Smokers | 130 (60.7) | 4 (28.6) | 134 (61.4) |
| Former smokers | 74 (39.3) | 3 (21.4) | 77 (35.4) |
| Non-smokers | – (0.0) | 7 (60.0) | 7 (3.2) |
| Histologic type | |||
| Epidermoid | 117 (57.3) | 1 (7.1) | 118 (54.1) |
| Adenocarcinoma | 38 (18.6) | 12 (85.8) | 50 (22.9) |
| Large cell | 7 (3.4) | – (0.0) | 7 (3.2) |
| Non-small cella | 15 (7.3) | – (0.0) | 15 (6.9) |
| Small cell | 22 (10.8) | – (0.0) | 22 (10.1) |
| Otherb | 5 (2.4) | 1 (7.1) | 5 (2.3) |
TNM Staging by Therapeutic Modality Applied.
The follow-up time of patients was between 5 and 23 years, except for those who died before the 5-year time point. Patient evolution was classified as shown in Table 3: (a) 63 were survivors with no evidence of recurrence or second cancers; (b) 24 had died for reasons other than recurrence or second cancer; (c) 65 had recurrence (local or distant) or progression of their first tumor, of whom 61 had died and 4 had survived; (d) 26 developed an SPPT, of whom 15 had died, and (e) 24 developed 1 or more SPTs outside the lung, of whom 18 had died. Finally, for 16 (7.3% of the 218), vital status could be determined, but insufficient data were available on their medical condition, due to failure to attend the planned visit or moving to another community or country.
Evolution, Recurrences and Incidence of Second Tumors.
| Deaths n % | Survivors at Last Visitan (%) | |
|---|---|---|
| Surviving with no evidence of recurrence or second primary tumor | – | 63 (75.0) |
| Died due to non-cancer death with no evidence of recurrence or second primary tumor | 24 (20.3) | – |
| Patients with recurrence or progression of primary tumor (local or distant) | 61 (51.7) | 4 (4.8) |
| Patients with a second primary lung tumor 1st and 2nd same histologic type 1st and 2nd different histologic types | 15 (12.7) 7 (5.9) 8 (6.8) | 11 (13.1) 4 (4.8) 7 (8.3) |
| Patients with second primary tumor in an extrapulmonary site | 18 (15.2) | 6 (7.1) |
| Total number of patients with documented follow-up | 118 (100.0) | 84 (100.0) |
| Patients with insufficient follow-up datab | 14 – | 2 – |
| Total | 132 | 86 |
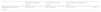
The mean interval and range from LC diagnosis until recurrence or appearance of a second pulmonary or extrapulmonary tumor are listed in Table 4. These intervals were divided into 3 groups: (a) <3 years; (b) 3–5 years; and (c) >5 years. Most recurrences (60.9%) were detected during the first 3 years, and only 7.8% appeared after 5 years. In contrast, the appearance of second tumors was much more common after 5 years in both pulmonary (84.6%) and extrapulmonary (66.6%) sites. In the case of second pulmonary tumors, in 11 cases the histologic types of the first and second tumors were the same; in these, the different site of the second tumor, the lack of mediastinal lymph node involvement, and the time until occurrence suggested that the lesion was a second primary tumor, rather than the alternative diagnosis of recurrence of the first. In the other 14 cases, the histologic types were different in the first and second tumors.
Interval Between Diagnosis of Primary Tumor and Recurrence or Appearance of a Second Primary Tumor.
| Recurrence of Primary Tumor | Second Primary Lung Tumor | Second Primary Extrapulmonary Tumor | p | |
|---|---|---|---|---|
| Mean interval (range) in months | 36.1 (12–90) | 86.7 (19–180) | 75.1 (24–234) | <0.01 |
| n (%) | n (%) | n (%) | ||
|---|---|---|---|---|
| Interval <3 years | 39 (60.9) | 1 (1.8) | 4 (16.6) | <0.001 |
| Interval between 3 and 5 years | 20 (31.3) | 3 (13.6) | 4 (16.6) | <0.001 |
| Interval >5 year | 5 (7.8) | 22 (84.6) | 16 (66.6) | <0.001 |
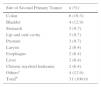
Table 5 shows the sites of the second extrapulmonary tumors: the most common were the colon (6 cases) and the bladder (4 cases).
Incidence of (a) SPP, (b) extrapulmonary cancer, or (c) any cancer in the group of men, expressed by number of cases/100 person-years, was analyzed according to the type of the first LC. The SPP rates were: (a) 1.29 person-years in adenocarcinomas; (b) 1.7 in epidermoid cancers; (c) 3.19 in small cell disease; and (d) 1.15 in the group of “other types” (Table 6). These rates were also analyzed according to whether patient received or did not receive TRT for treatment of their first tumor, with or without additional treatment. As can be seen, there are practically no differences between the groups in this regard (Table 7). Finally, the rates of second cancers observed in men were compared with the incidence in the general population aged 40 years or more of the same sex in our geographical region18,19 and the rates published in protocolized registries in other provinces in Spain20 (Table 8). The overall relative risk of cancer (or a second cancer, in our patients) was almost 3 times higher than in the general population of a similar age, although the greatest component of the increase in risk was due to the increase in LC risk (relative risk greater than 7).
Incidence of Second Lung Cancer and Other Cancers, by Histologic Type of the First.
| Epidermoid | Adenocarcinoma | Small Cell | Othera | |
|---|---|---|---|---|
| Rate of lung cancer/100 person-years | 1.70 | 1.29 | 3.19 | 1.15 |
| Rate of extrapulmonary cancer/100 person-years | 2.07 | 2.07 | 1.27 | 0.57 |
| Rate of any cancer/100 person-years | 3.77 | 3.36 | 4.46 | 1.72 |
Calculation of Rates and Estimation of Relative Risk of Lung and Other Cancers. Relative Risk of Second Cancer, by Thoracic Radiotherapy Treatment.
| Patients Who Received TRT | Patients Who Did Not Receive TRT | Relative Risk | |
|---|---|---|---|
| Rate of lung cancer/100 person-years | 1.49 | 1.88 | 0.79 |
| Rate of extrapulmonary cancer/100 person-years | 2.09 | 2.06 | 1.01 |
| Rate of any cancer/100 person-years | 3.58 | 3.93 | 0.91 |
TRT: thoracic radiotherapy.
Calculation of Rates and Estimation of Relative Risk of Lung and Other Cancers. Estimated Relative Risk of Cancer Compared to the General Population.
Population aging in the Western world and the availability of improved treatments has contributed to a situation in which it is not uncommon to see multiple cancers in a single patient.14,15 In lung cancer, most studies with long-term follow-up were performed in patients initially treated at early stages, and these patients have shown increased incidences of second cancers compared to cancer rates observed in the general population.8–12 Since incidence depends on the duration of the follow-up, it is more appropriate to express the incidence rate in terms of 100 person-years, which takes into account not only the number of patients, but also the overall length of follow-up.
In this study, we analyzed the evolution of our LC patients who had survived more than 3 years, irrespective of histologic type or treatment received, over a very long follow-up period.
Overall survival after LC is poor,2,3 and in our unselected case series, only 12.3% survived more than 3 years. The chances of recurrence or second primary cancers in these patients is very high. Thus, 65 (32.2%) of our 202 patients with documented follow-up presented local or distant disease recurrence. Kelsy et al.11 found that mean times to local or distant recurrence in patients who were resected in early stages of the disease were 14.1 and 12.5 months, respectively. We observed a longer time to recurrence (36 months) because we only included patients who had survived 3 years or more. However, in addition to this mean value, it is also interesting, from a clinical point of view, to study the events over wide intervals. Thus, in our experience, while most recurrences occurred during the first 3 years (60.9%), they remained relatively common up to the 5-year time point (31.3% of recurrences were detected between 3 and 5 years). After 5 years, the probability of recurrence falls: we only detected 5 in our series (7.8%). This distribution of recurrence by interval is quite close to that reported for a series of patients with non-small cell lung cancer, resected in stage I,8 even though our patients differed in many aspects (different stages, types, and treatments).
With respect to SPT in LC patients, the incidence of SPPT in resected patients has attracted particular attention, with studies, practically all retrospective, reporting rates of 1–2 cases/100 person-years.9,14 Although the rate in one prospective study was reported to be 4/100, lower rates were found in another prospective analysis in patients resected with disease stages II and III.20 Other authors14 have studied the incidence of SPT (both pulmonary and extrapulmonary) in patients with small cell lung cancer with >2 years survival post-diagnosis: they reported rates of 2–13/100 person-years and high relative risks compared to the expected rates in the general population.13 Our experience was similar to that of other groups,8,13–18 in that SPPTs were the most common second primary tumors, with rates of 1.79/100 person-years, accounting for almost half of all SPTs. When these rates were classified according to the initial primary tumor type, we found that most occurred after small-cell lung cancer. While very few reports have been published in this area, our finding coincides with the results of Johnson et al.14
As the rate of LC among men in our population is high,17,18 we compared the SPPT rate with rate of LC in the general population of men older than 40 years in our area and found a relative risk of 7.19. The incidence of other cancers was also greater than recorded in the general population of other Spanish regions, although the relative risk was lower (1.9). While we did not identify publications analyzing this aspect in case studies of LC patients from Spain, Kawahara et al.13 reported a Japanese series of small-cell lung cancer patients, in which they detected a relative risk of 3.6 SPT and 7 SPPT compared to the general population. It would be interesting to know if our results from a largely male group of LC cases could be extrapolated to women, in whom tumor types follow a different distribution. However, until very recently, the incidence of LC in women in our setting was very low, so this question could not be fully analyzed.
With regard to the interval, SPPTs can appear at any time, but generally do so 3 or 4 years after the first primary tumor. Aziz et al.12 found a mean interval of 46 months in patients resected for early stage disease; Keller21 reported 36 or 43 months in patients resected in stages II and IIIA, depending on the adjuvant treatment modality; Jeremic et al.,22 found that after 5 years, the SPPT rate increased from 1.1 to 2.2/100 person-years in early stage patients treated with radiotherapy only, although second extrapulmonary tumors occurred more commonly during the first 5-year period. In small-cell lung cancer treated with CT and TRT, most SPPTs are also detected after 4 or 5 years.13 In contrast, Duchateau et al.,15 in non-small cell lung cancer patients at various stages treated with various strategies (surgery, CT or TRT), found that 80% of SPTs (pulmonary or extrapulmonary) appeared within the first year. Nevertheless, the follow-up period in that study was short, and all patients were included, many of whom had short overall survival. Our cases, all of whom survived 3 or more years, were followed up for much longer periods (5–23 years) and give a broader picture. Accordingly, we found a much greater mean interval to recurrence or SPT (86 months) and the great majority of SPPTs (84.6%) appeared more than 5 years after the first tumor. We believe that the differences reported in the literature are due to differences in patient characteristics (histologic types, stages, and treatment modalities) and study methodology, but most SPPTs occur after the 4th or 5th year, in contrast to primary tumor recurrence, which occurs mainly during the first 3 years. These intervals coincide with the guidelines offered by Detterbeck et al.17 for distinguishing between primary tumor recurrences and SPPT in cases which may be unclear.
Several retrospective studies have attempted to explain the reasons for this high rate of second primary cancers. Kawahara et al.13 and Johnson et al.14 believe that persistent smoking and thoracic radiotherapy to the first tumor may be a contributing factor. However, Jeremic et al.22 conclude that while the rate of second primary cancers in patients with early-stage non-small cell lung cancer treated with radiotherapy is higher, it does not differ substantially from that of patients with the same disease stages treated with surgery alone. We compared the rates of pulmonary and extrapulmonary SPT in 2 groups of patients, 1 treated with TRT and 1 not treated with TRT, and found no differences (Table 7). As TRT was not the only treatment administered, we cannot draw definitive conclusions on its influence, but our results do not pinpoint a significant role for radiotherapy in the incidence of SPPT. To confirm this issue, large prospective studies would be needed in patients treated with TRT alone, followed up for more than 10 years, after which time the carcinogenic effects of radiation may be revealed.14
In any case, the greater incidence of SPT in patients with LC who did not receive radiotherapy would still need to be explained. The most plausible hypothesis for this phenomenon was proposed over 50 years ago by Slaughter et al.23 to explain the development of multiple primary tumors in oral cancers. Their “field cancerization” or “condemned mucosa” theory was subsequently applied to other organs, such as the head and neck, lung, esophagus, etc., and refers to the generalized damage caused to the mucosa in different sites in the form of precancerous lesions susceptible to degenerating into cancer. This concept is particularly applicable to the effects of smoking on the upper airways and the bronchi, and has been recently taken up again by Braahuis et al.24 These authors, using molecular techniques to analyze a series of precancerous lesions, observed cells in the tumor-free margins of head and neck cancers with genetic alterations linking them with the cells of the resected tumor. As regards LC, this concept offers not only a plausible explanation of the high frequency of SPPT but also of the common association between LC and head and neck cancer, perceived some time ago.25 In our patients, all of whom were smokers or former smokers, several of the SPTs involved the larynx, the esophagus, and the oral cavity, and like other authors, we also found high numbers of SPTs in the colon, the bladder, and the stomach (Table 5): smoking has been established as a causative factor in all these entities.26
Despite the long follow-up period recorded in our patients, the retrospective nature of this study rules out a comprehensive survey of second cancers. To achieve this, a long prospective study designed to carry out an exhaustive search for new tumors would be necessary, and would most likely uncover even greater relative risks. In our study, the estimation of the relative risk was indirect, and we were obliged to consult the registries of other regions in Spain, if only to compare the incidence of second cancers in general. However, we believe that inter-regional differences in Spain are not significant enough to substantially alter our final estimations.
ConclusionIn LC patients with long-term survival beyond the period for possible recurrence, the carcinogenic effects of smoking on multiple organs persist long after the 5-year time point. The most susceptible organ for developing a second tumor is the lung, and after 5 years, a second primary tumor is more likely than a recurrence of the first tumor.
Conflict of InterestsThe authors declare that they do not have any conflict of interests.
Please cite this article as: Sánchez de Cos Escuín J, Rodríguez López DP, Utrabo Delgado I, Gallego Domínguez R, Sojo González MA, Hernández Valle M. Recidivas y segundos tumores en el cáncer de pulmón de larga supervivencia. Arch Bronconeumol. 2016;52:183–188.