Occupational asthma (OA) is the most common work-related disease in industrialised countries. In 2008, only 556 cases of OA had been diagnosed in Spain, which is quite far from even the most conservative estimates. In this context, the aim of this paper is to estimate the number of asthma cases attributable to the work setting in Spain in 2008 as well as the related health care costs for the same year.
MethodsThe number of cases of OA was calculated from estimates of attributable risk given by previous studies. The cost estimation focused on direct health-care costs and it was based both on data from the National Health System's (NHS) analytical accounting and from secondary sources.
ResultsThe number of prevalent cases of work-related asthma in Spain during 2008 ranges between 168713 and 204705 cases based on symptomatic diagnosis, entailing an associated cost from 318.1 to 355.8 million Euros. These figures fall to a range between 82635 and 100264 cases when bronchial hyperreactivity is included as a diagnostic criterion, at a cost of 155.8–174.3 million Euros. Slightly more than 18 million Euros represent the health-care costs of those cases requiring specialised care.
ConclusionsEstimations of OA are very relevant to adequately prevent this disease. The treatment of OA, which involves a significant cost, is being financed by the NHS, although it should be covered by Social Security.
El asma laboral es la enfermedad respiratoria profesional más frecuente en países industrializados. En 2008 se reconocieron en España 556 casos de asma profesional, lo que contrasta incluso con las estimaciones más conservadoras. El objetivo es estimar el número de casos de asma atribuibles al trabajo en España en 2008, así como el coste de su atención sanitaria el mismo año.
MétodosEl número de casos de asma derivados del trabajo se calculó partiendo de las estimaciones de riesgo atribuible obtenidas en la literatura científica. La estimación de los costes se centró en los costes sanitarios directos, y se basó en el empleo de datos procedentes tanto de la contabilidad analítica del Sistema Nacional de Salud (SNS) como de fuentes secundarias.
ResultadosEl número de casos prevalentes de asma en España en 2008 atribuido a exposiciones laborales oscilaría entre 168.713 y 204.705 casos cuando el diagnóstico es sintomático, con un coste asociado entre 318,1 y 355,8 millones de euros. Estas cifras descenderían a entre 82.635 y 100.264 casos al añadir la hiperreactividad bronquial como criterio diagnóstico, con un coste de entre 155,8 y 174,3 millones de euros. Algo más de 18 millones corresponden al tratamiento sanitario de los casos que requieren atención especializada.
ConclusionesEstimar la magnitud del asma laboral constituye un elemento muy relevante para activar su adecuada prevención. El SNS asume unos costes significativos relativos a su tratamiento, que en todo caso deberían ser financiados por el sistema de Seguridad Social.
Exposure to various agents at work can induce asthma or aggravate pre-existing asthma The term “occupational asthma” (OA) refers to asthma that has been induced in the workplace. One of the most prevalent chronic diseases, asthma produces high morbidity, elevated costs from extensive use of health resources and significant deterioration in the quality of life of the patients.1 OA is an important health problem from both the personal and company viewpoints. It is the most frequent respiratory disease of occupational origin in industrialised countries. Approximately 250 specific work-related exposures have been linked to this disease.2–4
In recent years, occupation asthma has been estimated using various methods: studies based on the general population; data from medical practice; medical-legal programmes, with control and surveillance; transversal and longitudinal studies on high-risk workplaces; and prospective studies.
Community-based studies4–7 have produced estimations of attributable risk (AR) from exposure in the workplace (proportion of asthma linked to occupational exposure) that range from 2% to 20% (mean, 13.5%). The main limitation of these population studies is the lack of confirmation of OA through objective means. In addition, there may be classification errors because acute exposure can occur from spills of irritating substances in workplaces not considered among the high-risk industries. However, the studies based on the general population have the advantage of including individuals who have left the workplace after developing asthma.
Medical practice is another source of useful information about OA frequency,8–12 although there is considerable variation among countries and the mean of AR to work obtained for asthma is 11%, with an interval of 2%–33%.
The mean (interval) of AR to work for asthma obtained with surveillance or control systems is 5% (2%–17%), also with considerable inter-country variation. With the exception of Surveillance of Work-Related and Occupational Respiratory Disease (SWORD)13,14 and the Sentinel Event Notification System for Occupational Risk (SENSOR) programme in 6 states in the United States,15 the majority of the projects of this type have been short-lived.
As can be seen, the evidence on the percent of asthma that can be attributed to work-related causes is extensive and varied. A study in the American Thoracic Society2 reviewed all the studies published up to 2010 and estimated that 15% of the asthma cases were caused by work exposure. Nurminen and Karjalainen16 reviewed American and European studies (including a broad study carried out in Finland) and estimated that occupational agents caused or contributed to death from asthma in 18%.
Asthma prevalence in Spain is estimated at 4.9%, when the diagnosis is symptom-based, and 2.4% when bronchial hyperreactivity is added as a diagnostic criterion.17–20 In 2008, there were 556 asthma cases recognised as job-related, 341 in men and 215 in women.21 These figures differ greatly, even with the most conservative estimations of asthma attributed to occupational exposure described previously. As a result, a great part of the cost of their medical attention is transferred to the health system.
In this context, the aim of our study was to estimate the number of asthma cases attributable to work in Spain in 2008 and, likewise, to estimate their health attention costs in the same year.
Material and MethodsThe number of work-related asthma cases was calculated from the AR estimations from previously published studies. Once these estimates had been reviewed, the figures for attributable fraction selected were applied to the number of prevalent cases in Spain and to the databases with clinical information on the different healthcare levels in our national health system (NHS). This was done to obtain estimates on the prevalence of OA and the number of cases treated due to this health problem, respectively.
The cost calculation centred on direct health costs, performing 2 types of analyses for this estimation. Firstly, we estimated the cost with respect to the patients who had received some type of specialised care (SC). To do so, the data from NHS analytical accounting were used as the cost of hospital admissions and of specialised outpatient care (SOC), corresponding to the cases attended in public centres.22,23 Given that the NHS information system does not provide cost data corresponding to primary care (PC) and to pharmaceutical care (PHC) given to asthma cases, data from secondary sources were used to estimate these 2 components of the total cost.24
We accessed the statistical data of the NHS Information through the NHS Interactive Consult (available at: http://pestadistico.msc.es/PEMSC25/) and from the NHS information depository, after applying to do so and having a digital signature certificate (available at: https://repositorio.msc.es/risns/). The databases consulted were the hospital discharge records (MCDB-H; CMBD-H in Spanish)22 and the discharge records for specialised outpatient care (MCDB-SOC; CMBD-AAE in Spanish).23 The variable studied were as follows:
- -
Year: 2008.
- -
Hospital locations: all the autonomous communities.
- -
Age: ≥20years old.
- -
Sex: Male and female.
- -
CIE-9-MC diagnosis: CIE-9 493.0.
- -
Cases in the MCDB-H: discharges from admissions to public hospitals. Only the total number of valid discharges was considered in the calculation. From all the records processed, we excluded cases with discharge dates outside the year or nonexistent, duplicate records and records corresponding to possible cases seen without hospital admission (identical admission and discharge date, except if this was due to death, referral or voluntary discharge).
- -
Cases in the MCDB-SOC: cases seen (contacts, sessions, and visits, by care area). We considered only all valid cases. From all the records processed, we excluded cases with discharge dates outside the year or nonexistent, as well as duplicate records.
- -
Mean stay: average stay (from all the cases selected).
- -
Mean cost: mean cost estimated from the cases seen in a representative sample of NHS hospitals for the corresponding year.
- -
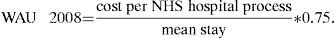
Weighted activity unit (WAU): assessment of the cost of SOC, adapting what is known as the “weighted healthcare unit” (WHU; UPA in Spanish)25 by production methods, incorporating the cost generated in areas of partial hospitalisation (day hospitals and home care) and surgery without being admitted (outpatient surgery) to hospital-produced cost.
- -
Weighted activity unit 2008 (WAU 2008): cost corresponding to SOC in 2008. To calculate it, a new variable was created using the formula:
In the second place, we calculated the global health expenses. Given that only poorly controlled PC patients generally generate SC expenses and only a small percent of asthma sufferers are hospitalised, these overall health expenses for the group of OA patients was calculated based on the figures for total expenses per patient with asthma obtained by Inoriza et al.26 and Martínez-Moragón et al.1 The first of these studies shows direct cost figures per patient for a total of 6 asthma-related clinical risk groups, expressed in 2006 Euros. Based on these figures, we estimated the total cost as the weighted sum per number of patients in each group. Finally, the resulting amount was updated to 2008, taking the consumer price index (CPI) as a reference for 2007 (4.2%) and 2008 (1.4%). After these calculations, the mean cost per asthma patient would be €1738 in 2008. Turning to the work of Martínez-Moragón et al., it consisted of a prospective, observational cohort study for adult patients with asthma, a group representative of the group of the Spanish asthmatic population. The estimations of this study yielded a mean cost of €1533 for 2007 (with a confidence interval of 95% [CI 95%] between €1133 and €1946). This figure was updated to 2008 Euros, obtaining a cost per patient of €1554 (CI 95%: €1149–€1973).
These costs were applied to the number of prevalent cases of work-related asthma in Spain in 2008 to obtain the total direct health expenses. Two prevalence rates were used for the calculation. The first was 4.9% (CI 95%: 4.2%–5.5%), estimated from the diagnosis based on clinical criteria (symptoms suggesting asthma); the second was 2.4% (CI 95%: 0.6%–4.2%), based on including bronchial hyperreactivity as a diagnostic criterion.17–20 The active population in Spain in 2008 was 22954100 (9832600 women), according to the 2008 Active Population Survey by the National Institute of Statistics.
ResultsThe number of prevalent asthma cases in Spain in 2008 attributed to occupational exposure is presented in Table 1. The estimates range from 56238 to 204705 cases, if a 4.9% prevalence is applied (when the diagnosis is symptomatic) and from 27545 to 100264 cases considering a 2.4% prevalence (adding bronchial hyperreactivity as a diagnostic criterion). Taking the latest scientific evidence on the proportion of cases attributable to occupational exposure (American Thoracic Society2; Nurminen and Karjalainen16), the figures that best reflect current reality lie between 168713 and 204705 prevalent cases (based on an asthma prevalence of 4.9% in Spain), and between 82635 and 100264 cases (based on a general prevalence of 2.4%).
Number of Prevalent Asthma Cases in Spain in 2008 Attributable to Occupational Exposure According to Published Attributable Risk Estimates.
| Estimates of Attributable Risk (Interval) for Asthma due to Occupational Exposure | No. of Prevalent Cases | Cases Attributed to Occupational Exposure | |
| AR (%) | |||
| Prevalence 4.9% (symptomatic diagnosis) | |||
| Population studies | 13.5 (2–20) | 1124751 | 151841 (22495–224950) |
| Medical practice data | 11 (2–33) | 1124751 | 123723 (22495–371168) |
| Surveillance or registry systems | 5 (2–17) | 1124751 | 56238 (22495–191208) |
| American Thoracic Committee, 2010 | 15 | 1124751 | 168713 |
| Nurminen and Karjalainen, 2001 | 18.2 | 1124751 | 204705 |
| Nurminen and Karjalainen, males | 17.8 | 642954 | 114446 |
| Nurminen and Karjalainen, females | 18.4 | 481797 | 88651 |
| Prevalence 2.4% (with bronchial hyperreactivity) | |||
| Population studies | 13.5 (2–20) | 550898 | 74371 (11018–110180) |
| Medical practice data | 11 (2–33) | 550898 | 60599 (11018–181796) |
| Surveillance of control systems | 5 (2–17) | 550898 | 27545 (11018–93653) |
| American Thoracic Committee, 2010 | 15 | 550898 | 82635 |
| Nurminen and Karjalainen, 2001 | 18.2 | 550898 | 100264 |
| Nurminen and Karjalainen, men | 17.8 | 314916 | 56055 |
| Nurminen and Karjalainen, women | 18.4 | 235982 | 43421 |
AR: attributable risk.
With respect to hospitalisation, 0.2% of hospital stays for men 20years of age or older and 0.6% in the case of women 20years or older were due to asthma in Spain in 2008. That year, 17087 hospitalisations for asthma were produced in individuals 20years of age or older (4424 men and 12663 women). The patients with asthma seen in SOC were 4229 (1428 men and 2801 women), and figures always for people 20years of age or older (Table 2).
Hospital Admissions and Outpatient Specialised Care Consultations due to Asthma in Spain in 2008 and Number of Cases Attributable to Occupational Exposure.
| Percent of Asthma Attributed to Occupational Exposure | PHC (%) | No. of Hospital Admissions (H) | H Cases Attributed to Occupational Exposure | No. in Specialised Outpatient Care (SOC) | SOC Cases Attributed to Occupational Exposure |
| Population studies | 13.5 (2–20) | 17087 | 2307 (342–3417) | 4229 | 571 (85–846) |
| Medical practice data | 11 (2–33) | 17087 | 1880 (342–5639) | 4229 | 465 (85–1396) |
| Surveillance or control systems | 5 (2–17) | 17087 | 854 (342–2905) | 4229 | 211 (85–719) |
| American Thoracic Committee | 15 | 17087 | 2563 | 4229 | 634 |
| Nurminen and Karjalainen, 2001 | 18.2 | 17087 | 3116 | 4229 | 770 |
| Nurminen and Karjalainen, men | 1.8 | 4424 | 787 | 1428 | 254 |
| Nurminen and Karjalainen, women | 18.4 | 12663 | 2329 | 2801 | 516 |
The number of hospital admissions and the number of SOC consultations are presented in Table 2. In addition, you can see the number of the cases attributable to occupational exposure in Spain in 2008, after applying the estimates published. The estimates for work-related hospital admissions vary between 342 cases (lower estimate from population studies, medical practice and surveillance or control systems) and 5639 cases (higher estimate derived from medical practice). Applying the estimate obtained by Nurminen and Karjalainen, work-related asthma admissions would be 3116, of which 2329 correspond to female cases. Of the patients with asthma seen in SOC, 85–1396 cases can be attributed to work. The estimate obtained from applying the figures of Nurminen and Karjalainen offer an intermediate level of 770 cases (516 for women and 254 for men).
In Table 3, we present the cost of SC (in-hospital and specialised outpatient) of the asthma cases attributed to occupational exposure, in individuals of 20years of age or older, by sex, seen by the NHS in Spain in 2008. For these calculations, we used the number of work-related cases obtained after applying the estimates that Nurminen and Karjalainen detailed by sex. Likewise, Table 3 shows the mean length of hospital stay, cost per hospital process and SOC cost.
Specialised Care Cost (In-hospital and Specialised Outpatient) of the Asthma Cases Attributed to Occupational Exposure. Spain, 2008.
| Men | Women | Total for Both | |
| Hospital admissions attributeda | 787 | 2329 | 3116 |
| Mean hospital stay length | 6.12days | 7.51days | 6.81days |
| Cost per hospital process | €2800.46 | €2879.38 | €2858.95 |
| Total hospital cost | €2203962.02 | €6706076.02 | €8908488.20 |
| SOC cases attributeda | 254 | 516 | 770 |
| WAU 2008 cost | €343.13 | €287.66 | €314.67 |
| Total SOC cost | €87155.02 | €148432.56 | €242295.90 |
SOC: specialised outpatient care; WAU 2008: weighted activity unit 2008.
Women constitute the greatest number of admissions and the number of days that they spend in the hospital is also slightly higher (7.5days against 6.1). This causes a small difference in the mean cost per hospital process between men and women. The difference is more relevant in the cases seen in areas of partial hospitalisation (day hospital and at-home) and with those treated with surgery without admission (outpatient surgery), whose cost is greater in the case of men (€343 against €288 for women).
The expenses of the public health system generated by hospital admissions due to work-related asthma amounted to almost 9 million Euros in 2008. The expenses for this concept are not the same for men and for women, with the cost of hospital stays due to these cases being 3 times higher for women than that corresponding to men.
The SOC costs reach, overall, €242296. The cost for men is, in this case, a bit more than half the cost estimated for women (Table 3).
The health cost for asthma SC is the result of adding the hospital admission cost plus the value of the hospital activity generated in partial hospitalisation areas (day hospital and at-home) and surgery without admission (outpatient surgery), which we have called costs from SOC cases. That is, the SC cost of the asthma cases studied is the sum of rows 4 and 7 in Table 3. This figure amounts to €9150784. In addition, you can see the breakdown by sex in Table 4.
Direct Health Costs for Work-related Asthma That Requires Specialised Care. Spain, Euros (2008).
| Specialised Care Costa | Primary Care Costb | Pharmaceutical Care Costc | Health Cost by Disease | |
| Men | 2291117.04 | 1152431.87 | 1090571.71 | 4534120.62 |
| Women | 6854508.58 | 3447817.82 | 3262746.08 | 13565072.48 |
| Total | 9150784.10 | 4602844.40 | 4355773.23 | 18109401.73 |
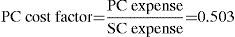
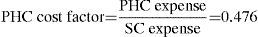
Once the SC cost was known, cost factors (relative weights) were applied for the PC and PHC calculated previously, to estimate the PC cost for health and the PHC cost for the diseases under study. These calculations are presented in Table 4, along with the total cost of health care linked to treating these cases.
We estimated that the work-related asthma cases studied, in individuals 20years of age or older who received SC, cost the NHS in 2008 a bit over 18 million Euros. Of this amount, 13.5 million corresponded to treatment for women and 4.5 million to that for men (Table 4).
Finally, Table 5 shows the health expenses corresponding to the work-related prevalent asthma cases in Spain in 2008, applying the figures for mean health cost of the asthmatic patient. Considering the prevalence found when diagnosis is based on bronchial hyperreactivity and symptoms, direct health costs range from 155.8 to 174.3 million Euros. If the diagnosis is based on disease symptoms, the health expenses rise to between 318.1 and 355.8 million Euros. Table 5 likewise presents the breakdown by sex for these figures.
Direct Health Costs of Work-related Prevalent Asthma in Spain in 2008.
| Source of Health Costs | ||
| Martínez-Moragón et al. (2009)1 | Inoriza et al. (2010)26 | |
| Mean cost (in Euros) | €1554 | €1738 |
| Prevalence 4.9% | Prevalence 2.4% | Prevalence 4.9% | Prevalence 2.4% | |
| Cases attributed to occupational exposure | ||||
| Men | 114446 | 56055 | 114446 | 56055 |
| Women | 88651 | 43421 | 88651 | 43421 |
| Total | 204705 | 100264 | 204705 | 100264 |
| Total cost (in Euros) | ||||
| Men | 177849084 | 87109470 | 198907148 | 97423590 |
| Women | 137763654 | 67476234 | 154075438 | 75465698 |
| Total | 318111570 | 155810256 | 355777290 | 174258832 |
The estimated figures for work-related asthma cases contrast sharply even with the most conservative estimates. This makes the prevention of OA much more difficult in our country, given that one of the key elements for prevention is the identification itself as a work-related illness. If these cases do not count in the official statistics on work-related damages, it is difficult to include them in the plans and programmes for prevention of occupational risk. Correctly identifying OA is crucial for its prevention. In effect, it is an illness that is preventable, treatable and potentially curable through the combination of an individual strategy based on treatment of the cases, plus another population strategy by means of different public health measures. Among these is the prevention of exposure to various agents in the workplace. It is important to identify and act on allergens existing in the workplace, because the benefits are not limited to the work environment. The general population is equally exposed to these substances.
The objective of this study was to add another element that promotes the growth of work-related asthma: the cost involved in its health care. We have estimated that work-related asthma in Spain, in people 20years of age or older, would have cost between 155.8 and 174.3 million Euros (and between 318.1 and 355.8 million Euros, considering diagnosis through bronchial hyperreactivity and symptoms alone, respectively). Somewhat more than 18 million would correspond to health treatment for the cases that need SC. It must be remembered, nevertheless, that the cost factors calculated based on the work of Pastor and Gisbert24 that are used to estimate PC and PHC costs are extrapolating to the entire country figures that refer to a reduced population, such as that of the Bajo Ampurdán, and that might not correspond exactly with the mean for the Spanish population. Furthermore, these cost factors would really correspond to the group of the population seen for asthma cases, and not only to the patients who receive SC. This might be introducing a bias in the calculations. At any rate, it is necessary to consider that this study estimates only the direct health costs of OA occupational; it ignores the amount of the indirect costs (mainly derived from work productivity lost or diminished by patients and informal caretakers) and intangible costs (referring to the pain and suffering that both the asthmatic and their families undergo). A recent study27 shows that, in the mid-1990s, from all the direct and indirect costs related to asthma, the latter represented approximately 58%. Nevertheless, this proportion would have undergone a notable drop, to 42% in 2004.
The Social Security system's lack of sensitivity to recognise occupational diseases is acknowledged. Studies carried out in our own country demonstrate this under-recognition.28,29 The main reasons behind such under-declaration are that many occupational illnesses are considered to be common, the scientific difficulty itself of classifying a disease as occupational,30 the lack of knowledge on the part of health professionals of work-related risk factors,31 the lack of interest shown by health care in prevention and the conflicts between employers and workers in recognising that an illness is work-related.32
To surmount these difficulties and estimate the percent of cases that can be attributed to occupational exposure, we used the most recently published AR. These constitute an estimated percent of mortality or morbidity of a disease that is attributed to specific work conditions. Technically, it is not easy to estimate which percent of the total cases are due to work; the differences in the methods used can also explain (at least partially) the variability in the figures. Furthermore, the discrepancies in the estimates can arise not only from different political or ideological positions, but also (and quite fundamentally) from differences in the prevalence of industrial processes and sources of exposure in the workplace. It is important to base the calculations on real data and to describe clearly the suppositions and methods used to make the estimates, as well as to explain any possible uncertainties or biases present in the evaluations.33 Using attributable fractions from studies carried out in other countries can be considered the first limitation of our study, although it is common to other jobs.33–35 In our case, we tried to minimise the errors by calculating the mean of the estimates to describe the number of work-related cases; however, in the end we used those of Nurminen and Karjalainen16 for cost calculation because of their quality, rigor and greater completeness. Even so, we have to point out that these estimates take into account only the situations for which there is sufficient scientific evidence. That is why, at any rate, the figures derived from this study would act as a lower limit to the number of work-related asthma cases.
With respect to health expenses, which we know, the magnitude of the economic impact of the set of occupational diseases in Spain has been estimated in only 2 published studies: one by the European Agency for Safety and Health at Work36 and another by García et al.29 The first is based on a survey of the Member States in which Spain estimated the amount of direct and indirect costs as a bit more than 3% of the GDP. The second study opted for taking the direct cost data from a North American and for only 4 groups of diseases, estimating that the total cost of the occupational diseases was nearly 4.7% of the GDP. The strength of our study is that we performed the calculations based on Spanish data on health resource consumption and its derived costs, as well as the NHS accounting data.
By estimating only direct health costs, our figures offer a downward estimate of the total cost that these work-related asthma cases generate. Even so, it is a significant amount of money, especially that corresponding to the prevalent asthma cases. As can be seen, the mean total cost of the asthmatic patient is lower than the mean hospital cost. This is because, in general, only poorly controlled patients generate hospital expenses and only a small percent of asthma sufferers are hospitalised. This also explains the difference between the amount obtained on the health expense of the asthma prevalent and those linked to the cases that require hospitalisation.
The limitations of this section of our study involve the coverage of the primary SC cost used, and the use of secondary information sources to calculate the PC and PHC costs. With respect to the primary data, the information system coverage is 100%, in both the case of hospital admissions and in that of surgical activity, but only 46.7% in the day hospital medical activity, based on the statistics for sanitary establishments with in-house schemes.37 This limitation again leads us to underestimate the SC cost for these diseases; it is necessary to add the SC that is produced when calculating the expenses of its PC and PHC, based on that cost. As we explained in the Methods section, given the total lack of primary information sources on the components of the direct costs, the most normal procedure is to combine primary and secondary sources. It should be pointed out that the difficulties involved in accessing relevant information in this environment are not exclusive to Spain. Other countries also find themselves in a similar situation.38
From everything that has been presented, important conclusions can be reached, which have 2 main consequences. The first is that the companies responsible for occupational exposure that cause the illness do not need to pay the real cost of such exposure, which will be taken on by the taxes of all the citizens.33 Neither do they feel concerned about the need to activate measures for its prevention, nor do the work authorities demand the pertinent modifications in the work environment of them. And the second consequence is that a Health Services financial overload is produced.
Estimating the magnitude of OA constitutes a very relevant element for activating its appropriate prevention. If it were recognised as an occupational illness, it would be included in the Strategies for Safety and Health in the Workplace, in the NHS strategies and in companies’ specific prevention plans. On the other hand, the NHS is taking on significant costs related to its treatment, which at any rate should be financed by the Social Security system.
FundingThis study was carried out with funding provided by the Francisco Largo Caballero foundation (2010).
Conflict of InterestThe authors have no conflict of interests to declare.
Please cite this article as: García Gómez M, et al. Costes sanitarios directos del asma de origen laboral en España: una estimación para el año 2008. Arch Bronconeumol. 2012;48:355–61.