Lymphangiomatosis is an uncommon systemic disease characterized by a marked proliferation and dilatation of the lymphatic vessels.1 It can appear as either localized or diffuse affectation, in which case it is known as diffuse pulmonary lymphangiomatosis (DPL). It may affect newborns and young adults. Although it is a benign disease of unknown etiology and pathogeny, it presents a high rate of relapse and a poor prognosis.
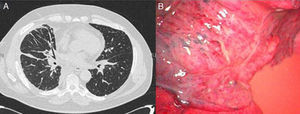
We present the clinical case of a 55-year-old male patient, ex-smoker with a history of hypertension, dyslipidemia and COPD with bronchodilator treatment. He came to the emergency unit due to dyspnea with minimal exertion that had been evolving over the period of a month. The basic analytical data were normal; chest radiograph revealed basal bronchiectasis, and spirometry presented an obstructive pattern. On computed tomography (CT), multiple mediastinal lymphadenopathies were observed as well as perihilar interstitial affectation (Fig. 1A) and pericardial effusion. Bronchoscopy revealed diffuse thickening of the bronchial mucosa and widening of the main and bronchial carinas. The mediastinal affectation was studied using mediastinoscopy, where anthracotic-looking lymphadenopathies and fatty nodules were observed; their biopsies presented lymphorrhea. The study of the liquid drained from the mediastinum confirmed that it was chylous with no malignant cellularity; the microscopic study of the lymphadenopathies was not conclusive. Afterwards, a lympho-gammagraphy was performed, where adequate lymphatic migration was seen without signs of leakage at the level of the thoracic duct. Given the lack of diagnosis and persistence of the dyspnea, pulmonary and mediastinal biopsies were taken by means of video-assisted thoracoscopy. The anatomopathologic study revealed proliferation of dilated capillary vessels in the pleura and septa and mediastinal adipose tissue with proliferation of anastomosed lymphatic vessels and lymphoid accumulations, leading to the definitive diagnosis of DPL. After successive episodes of dyspnea with minimal exertion secondary to pleural effusion (chylothorax), surgical treatment was indicated. Video-assisted thoracoscopy showed evidence of the characteristic proliferation and dilation of the lymphatic vessels and lymphorrhea in the lung parenchyma and mediastinum (Fig. 1B). Ligation of the thoracic duct and pleurodesis was carried out. Post-operative evolution was favorable, and the patient was discharged 10 days later.
DPL is an uncommon lymphatic alteration that appears in children and young adults, while it is quite exceptional in patients over the age of 40.1 The most frequent symptom is dyspnea. It may be erroneously diagnosed as asthma responding to bronchodilator treatment, which was the reason for the late diagnosis in our case, previously diagnosed with COPD with bronchodilator treatment. It is associated with pleural effusions, other lymphatic abnormalities and in 75% of cases with bone alterations. The coexistence of chylothorax and lytic bone lesions may direct the diagnosis.1 The definitive diagnosis should be histological, as the evidence on radiological images coincide with other alterations of the lymphatic system,2 and mediastinal affectation is rare. In the case of recurring chylothorax, drainage and pleurodesis are indicated, with the option of thoracic duct ligation3 to prevent complications such as malnutrition, pulmonary fibrosis and deteriorated respiratory function. In our case, we opted for ligation using a video-assisted thoracoscopic approach, which has not previously been reported in the literature in this pathology. Other treatments described are: radiotherapy, which causes sclerosis and fibrosis of the dilated lymphatic vessels, with good results4; INTalpha2b5; and bilateral lung trasplantation.6 It is a progressive disease with a high rate of relapse and poor prognosis, and the main cause of death is lung function deterioration secondary to infection or pleuropericardial effusion.
The case presented is especially unusual due to the age at which it debuted, which is the highest seen in the literature. It is also uncommon due to its clinical expression, with mediastinal lymphadenopathies and pleuroparenchymal affectation from its onset, unlike the majority of the published cases. Minimally invasive surgery was used for the diagnosis as well as for the treatment with positive results, and it has been shown to be an effective technique with minimal morbidity and mortality. Despite the poor prognosis of the disease, 5 years after the treatment the patient has not presented new episodes of pleuropericardial effusions, nor has he required hospitalization for other symptoms, currently presenting only exertional dyspnea.
Dr. J. López, Pulmonology Department, for his collaboration and help.
Please cite this article as: Caballero Y, et al. Linfangiomatosis pulmonar difusa con afectación mediastínica. Arch Bronconeumol. 2011;47:474–5.