Waldenström's macroglobulinemia (WM) is a lymphoid malignancy characterized by infiltration, mainly of the bone marrow and lymph nodes, by small mature lymphocytes showing plasmacytoid differentiation, associated with an IgM monoclonal band, and in general, a low degree of aggressiveness. We present the first case reported in the Spanish literature of interstitial lung disease presenting as MW and we review the literature.
La macroglobulinemia de Waldenström (MW) es una neoplasia linfoide caracterizada por una infiltración principalmente de la médula ósea y del ganglio linfático por linfocitos pequeños maduros o con diferenciación plasmocitoide, con banda monoclonal IgM asociada, y en general un bajo grado de agresividad. Presentamos el primer caso publicado en la literatura española de enfermedad pulmonar intersticial difusa como forma de presentación de una MW y realizamos una revisión de la literatura.
Wäldestrom's macroglobulinemia (WM) is a lymphoid malignancy characterized by infiltration of the bone marrow, lymph nodes or other tissues by small mature lymphocytes showing plasmacytoid differentiation. It is associated with the presence of an IgM monoclonal band and generally has a low degree of aggressiveness. The incidence of pulmonary manifestations is low, and it is even rarer for pulmonary disease to constitute the onset of the disease. We present the first case reported in the Spanish literature of interstitial lung disease as the initial presentation of WM and a review of the literature.
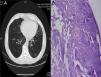
Clinical CharacteristicsA 73-year-old male ex-smoker was referred to our hospital with chronic cough. Pulmonary auscultation revealed bilateral basal fine end inspiratory crepitations. No lymphadenopathy or hepatosplenomegaly was observed. The chest X-ray showed mild diffuse opacity on both lower fields. High-resolution computed tomography (CT) showed interstitial involvement with mainly peripheral thickening of the interlobular septa of the left lung, associated with bilateral, patchy areas of ground glass opacities, mainly in the peripheral regions (Fig. 1A).
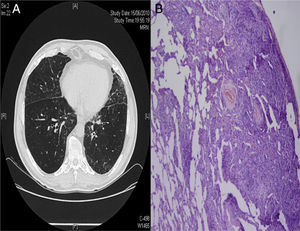
(A) High-resolution computed tomography showing interstitial involvement, characterized by mainly peripheral interlobular septal thickening associated with areas of ground glass opacities. (B) Lung parenchyma with an area of patchy lymphocytic infiltration, alternating with an area of lung parenchyma with no significant histological changes.
Clinical laboratory tests reported an ESR of 88mm with normal or negative blood panel, glucose, urea, creatinine, transaminases, lactate dehydrogenase (LDH), antinuclear antibodies (ANA), anti-DNA, extractable nuclear antigen (ENA), monoclonal IgM of 3450mg/dl, and negative urine Bence–Jones protein.
A lung biopsy was performed by video-assisted thoracoscopy (Fig. 1B), revealing areas of pulmonary parenchyma with no significant histological changes, alternating with lymphoid infiltration due to small lymphocytes with plasmacytoid differentiation in some areas. The immunohistochemical phenotype was CD20+, CD79a+, CD23−, cyclin D1−, EBER−, CD15 and CD30−. MiB proliferation index was low and predominantly distributed in the subpleural and peribronchial regions, with the presence of histiocytes. Accordingly, this examination was compatible with a diagnosis of lymphoplasmacytic lymphoma. A bone marrow test was performed, showing infiltration by lymphoplasmacytoid cells, with the following immunophenotypes: CD19+, CD45+ strong, CD5−, CD23−, CD20+, CD22+, CD79b+, FMC7+ weak, CD25+, CD38+ variable, and IgM+ and monoclonal cytoplasmic kappa light chains.
In view of these results, a diagnosis of non-Hodgkin lymphoplasmacytic lymphoma with pulmonary and bone marrow involvement was made and rituximab treatment was initiated. In the subsequent check-ups, the cough resolved and IgM levels fell. Most of the lesions on CT resolved, and only some areas of interlobular septal thickening persisted, mainly in the peripheral bases.
DiscussionLymphoproliferative lesions affecting the lung are rare. Among these, primary lymphomas, defined as clonal lymphoid proliferation isolated from the lung, are even more uncommon, representing an estimated 1% of all lymphomas and 0.5% of all lung tumors. Pleuropulmonary involvement in WM is infrequent and the most typical respiratory symptoms are dyspnea and cough. In the early case descriptions, only pneumonia and pleural effusion were identified as pulmonary manifestations of WM,1 but later reviews have shown that the spectrum of respiratory involvement is wider. Interstitial pulmonary involvement, as such, is exceptional and may be underreported.
After performing a search of the literature in the PubMed and Medline databases, we only found 7 articles2–8 describing cases in which the disease presented as a pulmonary event (Table 1). Among these, we did not find any cases similar to the one discussed here, which presented initially as diffuse interstitial lung disease.
Case Study of Pulmonary Involvement as First Manifestation of Waldenström's Macroglobulinemia.
| Author (year) | Ref. | No. of cases | Respiratory symptoms | Radiological findings | Diagnostic method |
| Hull (1982) | 2 | 1 | Dyspnea, cough | Infiltration | BMB, TBB |
| Bruno (1968) | 3 | 1 | Dyspnea | Mass, pleural effusion | TBB, OLB |
| Winterbauer (1974) | 4 | 2 | Dyspnea, cough or asymptomatic | Infiltration | BMB, autopsy |
| Moeschlin (1966) | 5 | 1 | Dyspnea, cough | Infiltration | OLB |
| Strunge (1969) | 6 | 1 | Dyspnea, hemoptysis | Infiltration, mass, pleural effusion | Autopsy |
| Fadil (1998) | 7 | 1 | Dyspnea, cough | Infiltration, mass, pleural effusion | BMB, TBB |
| Butí (1984) | 8 | 1 | Dyspnea on effort | Infiltration, pleural effusion | Pleural biopsy |
| Case described | 1 | Cough | Interstitial lung disease | VTLB |
BMB: bone marrow biopsy. TBB: transbronchial biopsy. OLB: open lung biopsy. VTLB: video-assisted thorascopic lung biopsy.
Although there are studies that support bronchoscopy (transbronchial biopsy and bronchoalveolar lavage)9 as methods for the diagnosis of lymphoproliferative disorders of the lung, others claim that the efficacy of these methods is poor,10 with diagnostic yields of between 15% and 30%. These results suggest that surgical biopsy may be the procedure of choice for the diagnosis of lymphoma in potentially operable patients. In our case, given the good clinical status of the patient and as a minimally invasive approach using video-assisted thoracoscopy via a single port could be used, we opted for surgical biopsy. The pathological findings suggested a differential diagnosis of lymphoid interstitial pneumonia, lymph node hyperplasia or even hypersensitivity pneumonitis.
In this patient, the laboratory finding of monoclonal gammopathy suggested a diagnostic hypothesis of a lymphoproliferative process. This was subsequently confirmed with the histological testing. In WM, the lymphoid infiltration may have a histological component of plasmacytoid lymphocytes or small mature lymphocytes. For this reason, immunohistochemistry or flow cytometric immunophenotyping is essential for differentiating this entity from other lymphoproliferative processes, such as lymphocytic lymphoma or follicular lymphoma (grade I) that also involve the proliferation and accumulation of small lymphocytes.
Finally, the test results and a review of the literature confirmed a non-low grade Hodgkin's lymphoma with plasmacytoid differentiation, compatible with a diagnosis of WM.
Please cite this article as: Consuegra A, Marcos PJ, Vázquez R, Pombo J, Debén G, Verea-Hernando H. Enfermedad pulmonar intersticial difusa como primera manifestación de macroglobulinemia de Waldenström: descripción de un caso y revisión de la literatura. Arch Bronconeumol. 2014;50:151–153.