Exercise-induced laryngeal obstruction (EILO) indicates an inappropriate, transient, reversible narrowing of the larynx in response to exercise.1 EILO is an important cause of a variety of respiratory symptoms that frequently mimic asthma and/or dysfunctional breathing, with a prevalence in general populations of older children and adolescents between 7% and 16%.1 Although the European Respiratory Society and the European Laryngological Society established the basis for the current diagnosis and management of EILO on 2017, most aspects of this condition are still not fully understood.1 Diagnosis of EILO requires a high degree of clinical suspicion and confirmation by visualization of the larynx during exercise by the gold standard test, known as continuous laryngoscopy during exercise (CLE). CLE is a complex diagnostic test that requires the participation of pneumologists and otolaryngologist to record the movements of the larynx during an exercise test. This complexity is a major barrier due to the limited access to the test for the general population.2 In addition, the subsequent management and treatment require a multidisciplinary team to ensure a proper approach.3 Particularly in Spain, there are very few reports of this disease4 and, to the best of our knowledge, there is no multidisciplinary team dedicated to EILO throughout the country. In 2021, we established a multi-disciplinary EILO team consisting of specialists in otorhinolaryngology, pulmonary medicine, rehabilitation medicine, speech language pathologist, physiotherapy and pediatric medicine in our tertiary hospital. The main objective of this study is to describe the initial results on the diagnosis and treatment of EILO in a cohort of patients referred to our multidisciplinary team.
The protocol (ID 2024-11454) was initiated by clinical suspicion raised by the pulmonologist or pediatrician. Subsequently, the otolaryngologist scheduled a fiber optic laryngoscopy at rest. After confirming a correct larynx evaluation at rest, the patient was scheduled for CLE.1 Patients signed the informed consent before CLE. The patients underwent a CLE on a cycle ergometer following an incremental protocol, which consists on a progressively increasing load (watts) every minute until the patient reaches exhaustion, and maximum values. It was performed on a cycle ergometer (Ergoline Ergometrix 900, Uberprüfung, Germany), with the patient monitored using a 12-lead electrocardiogram, oxygen saturation measured with a pulse oximeter (Wirstox2, Model 3150, Nonin, Plymouth, USA), and a gas analyzer (Medisoft Ergocard® CPX clinical, Ergometrix). Objective variables such as oxygen consumption (VO2), minute ventilation (VE), respiratory quotient, heart rate, blood pressure, and oxygen saturation were recorded, along with subjective variables obtained using the Borg scale (visual analog scale) to assess the level of dyspnea and leg discomfort perceived by the patient (before and after exercise). Laryngeal exploration was conducted using video nasopharyngoscopy introduced through the effort mask, following prior intranasal application of 2% lidocaine, which allows to visualize the airway during the test. Before starting the exercise, resting values were recorded, baseline spirometry was performed, and the maximum inspiratory capacity value was measured. Informed consent was obtained beforehand. With the laryngoscopy, we visualized the upper airway in order to look for abnormal adduction or collapse in both glottic and supraglottic space. Once the diagnosis of EILO was confirmed,5 the patient was referred to the rehabilitation department, where the speech pathologist initiated individualized treatment. The treatment program comprised five 45-minute face-to-face sessions supervised by a speech therapist. Before beginning therapy, an interview took place involving the patient and one family member (in the case of minors) along with the therapist. We aimed to understand the specific situations in which the obstruction occurred, including the type of physical activity, its intensity, frequency, duration, and the strategies of the patients response to the obstruction. Additionally, it was valuable to identify if laryngeal obstruction occurred in contexts unrelated to physical exercise. The therapist's examination involved both an interview and a functional assessment of posture at rest and in motion, as well as an evaluation of breathing (including type, mode, and respiratory rate). During the initial sessions, patients were instructed in biphasic inspiration and expiration lengthening, focusing on 1/4 cycles. The recommendation was to begin practicing these techniques at rest, gradually increasing exercise intensity. In the second session, the focus shifted to postural and breathing modifications, along with the introduction of laryngeal relaxation techniques. By the third session, we commenced, inspiratory muscle training (IMT) using the Orygen Insp Valve (Forumed SL, Girona, Spain) for cases of glottic EILO. Subsequent sessions were dedicated to consolidating these techniques and determining the most effective way to generalize the appropriate breathing pattern for each patient.
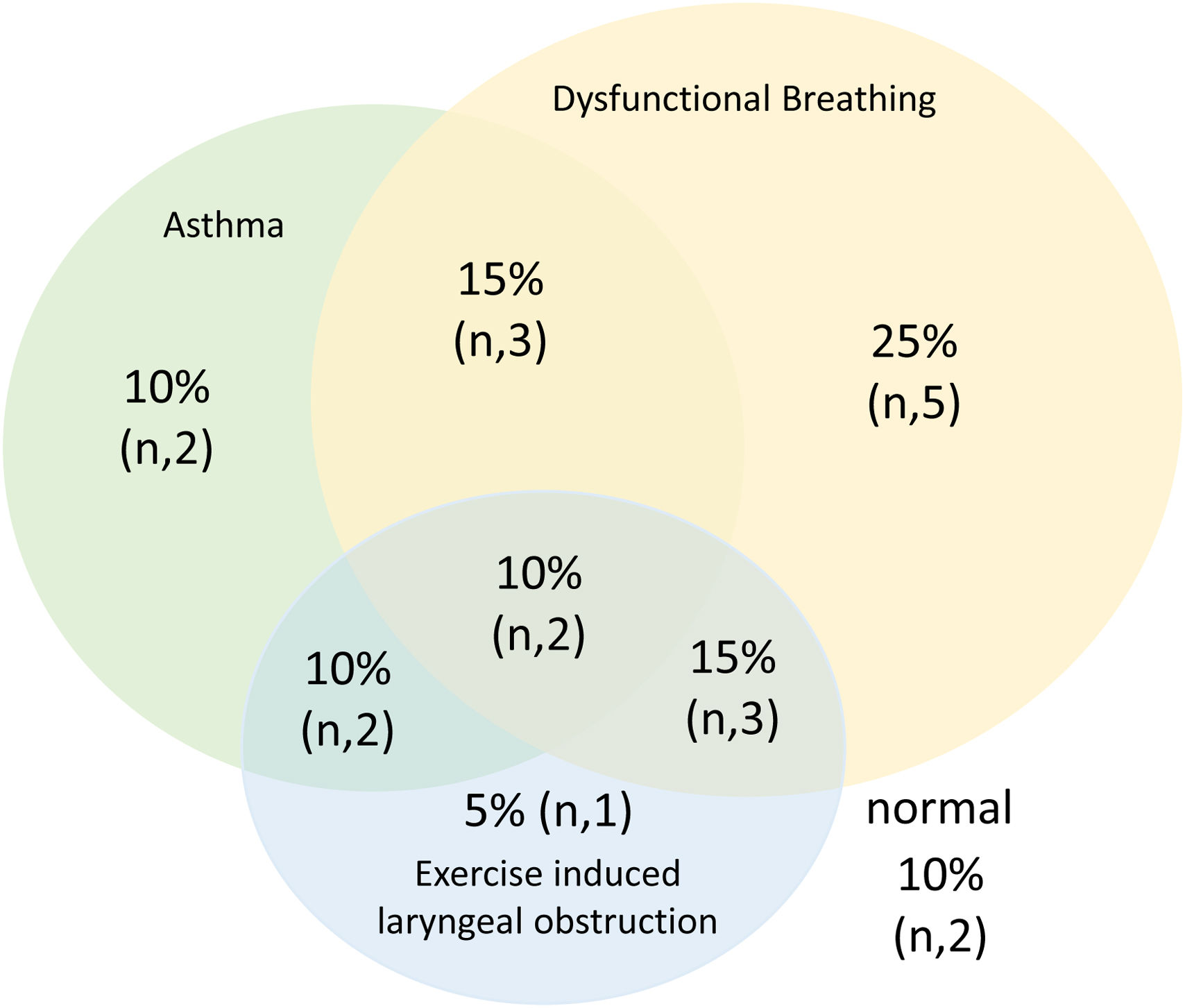
Twenty CLE tests were performed in patients with suspected EILO from January 2022 to February 2024. Table 1 describes the clinical characteristics of the patients. Eight patients (40%) were under 15 years old; only six patients (30%) were older than 45 years old. Nine patients (45%) were referred from multidisciplinary asthma unit and three patients (15%) from outpatient respiratory clinics. All patients were referred due to inspiratory symptoms mainly at high- intensity level of exercise, with or without a combination of other symptoms including throat tightness (85%), dizziness (10%), upper chest tightness (15%), noisy breathing (5%), stridor (5%), hoarseness (5%), cough (30%) changes of the voice (5%) and panic reaction (15%). On CLE, eight (40%) patients had EILO (4 of which presented glottic obstruction and the other four presented supraglottic obstruction, one of that patient was combined with a glottic obstruction) and thirteen (65%) patients showed dysfunctional breathing.6 We did not find any complication during CLE. Fig. 1 shows the prevalence and coexistence of asthma, EILO, and dysfunctional breathing patterns. Of the five patients who started treatment, an average of five therapy sessions were required before discharge. Four patients reported more frequent and complete physical activity participation immediately post-therapy as well as reduced inhaler use in asthmatic patients.
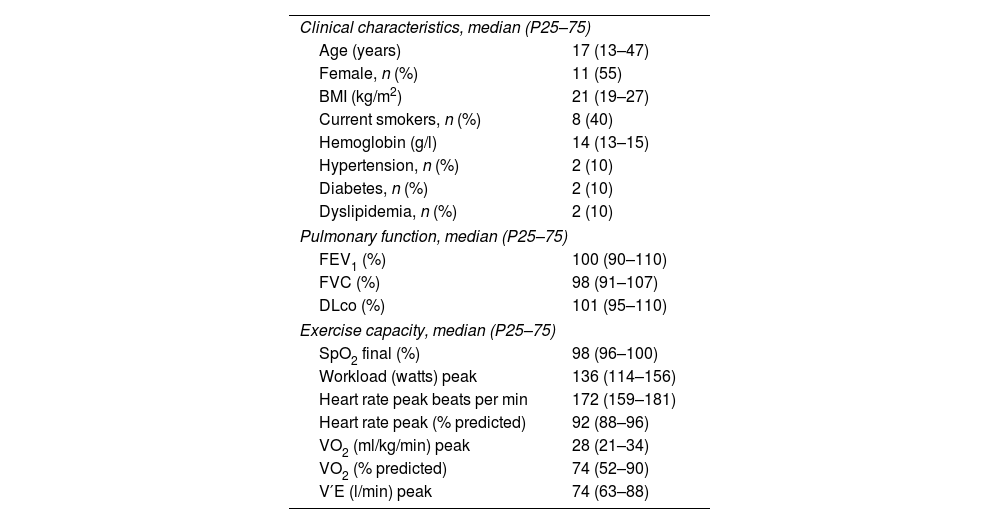
General Characteristics of the Study Population (n=20).
| Clinical characteristics, median (P25–75) | |
| Age (years) | 17 (13–47) |
| Female, n (%) | 11 (55) |
| BMI (kg/m2) | 21 (19–27) |
| Current smokers, n (%) | 8 (40) |
| Hemoglobin (g/l) | 14 (13–15) |
| Hypertension, n (%) | 2 (10) |
| Diabetes, n (%) | 2 (10) |
| Dyslipidemia, n (%) | 2 (10) |
| Pulmonary function, median (P25–75) | |
| FEV1 (%) | 100 (90–110) |
| FVC (%) | 98 (91–107) |
| DLco (%) | 101 (95–110) |
| Exercise capacity, median (P25–75) | |
| SpO2 final (%) | 98 (96–100) |
| Workload (watts) peak | 136 (114–156) |
| Heart rate peak beats per min | 172 (159–181) |
| Heart rate peak (% predicted) | 92 (88–96) |
| VO2 (ml/kg/min) peak | 28 (21–34) |
| VO2 (% predicted) | 74 (52–90) |
| V′E (l/min) peak | 74 (63–88) |
BMI: body mass index; FEV1: forced expiratory volume during first second; FVC: forced vital capacity; DLco: diffusing capacity for carbon monoxide; SpO2: arterial oxygen saturation measured by pulse oximetry; VO2: oxygen uptake; Max: maximum; V’E: minute ventilation.
According to our understanding, this is the first report of the approach to diagnosis and management of EILO implemented by a multidisciplinary team in Spain. The diagnosis of EILO is difficult to make based on clinical assessment because many potential confounding factors may be present.2 In this line, our results are similar to other series particularly in children and young adults under assessment by CLE.7 However, it has been recognized that self-reported symptoms are poor predictors of EILO, in which a high index of suspicion remains the key factor for diagnosis.1 There are some symptom questionnaires that attempt to detect EILO8 in the context of inspiratory breathing difficulties in typical athletic children or young adults but none of them are validated in Spanish so far. Current analyses indicate that the multidisciplinary approach is the best option to achieve an adequate response to treatment. Our results, with up to 80% of patients experiencing symptom improvement, are similar to the few previous reports.9,10 Although the analyses have limitations due to its small size and retrospective nature, the work sets the scene for future multidisciplinary teams approaches for patients with suspected EILO. Pulmonologists are usually the first line providers, and they must be an essential part of these teams to detect symptoms and clinical presentation and to rule out other respiratory conditions, especially asthma.2
In conclusion, the diagnosis of EILO is frequently delayed by the belief to be a rare disease and the nonspecific clinical presentation. Also, access to CLE test for diagnosis is limited to expert centers. Early diagnosis and specific treatment based on speech therapy and rescue breathing exercises decrease symptoms.
FundingNo funding was used for this study.
Conflict of InterestThere are no conflicts of interest to report.
Due to the nature of the approach and services involved in the diagnosis and management of these patients we exceptionally included 10 authors.