Journal Information
Vol. 61. Issue 1.
Pages 44-46 (January 2025)
Share
Download PDF
More article options
Vol. 61. Issue 1.
Pages 44-46 (January 2025)
Scientific Letter
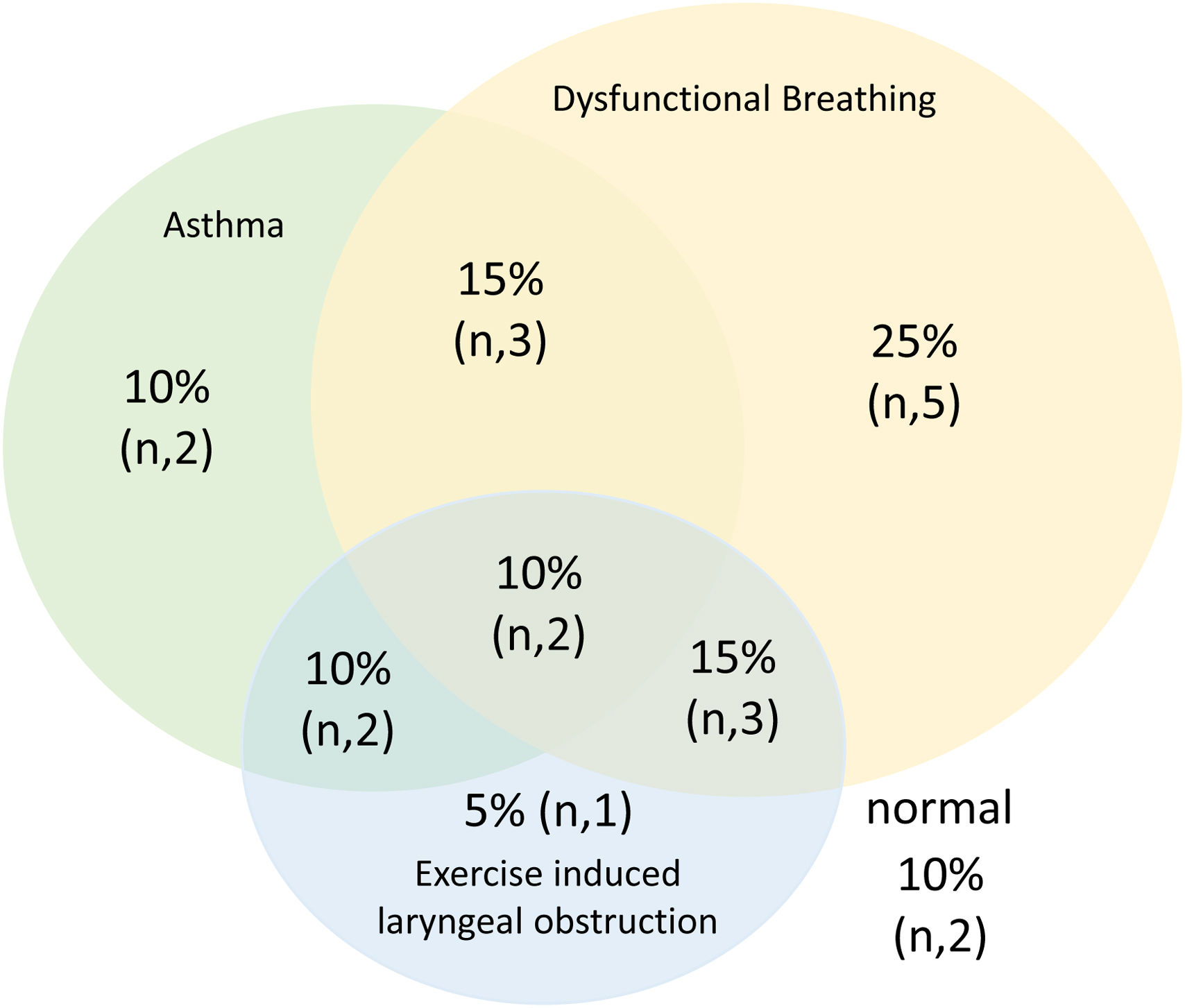
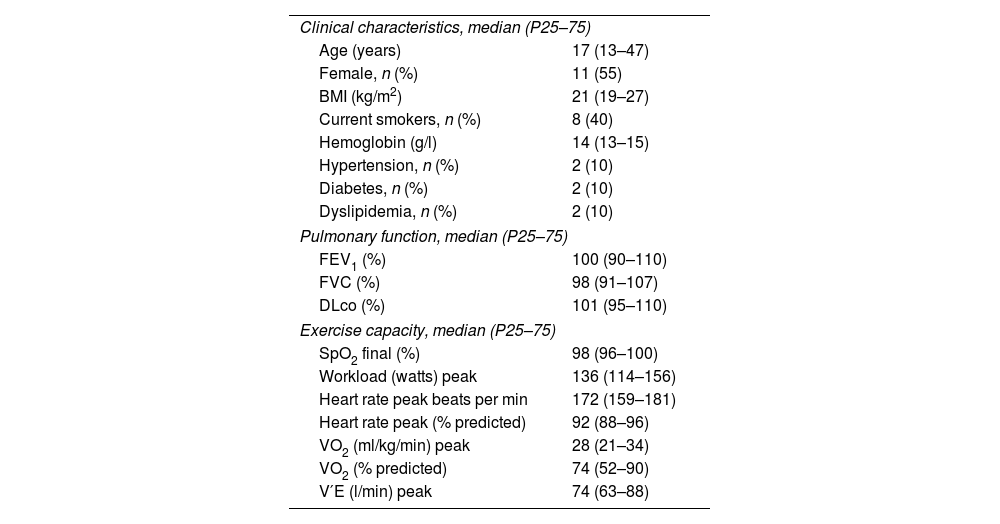
Diagnosis and Management of Exercise-induced Laryngeal Obstruction (EILO): Initial Results of a Multidisciplinary Team
Visits
1409
Diego A. Rodríguez-Chiaradíaa,b,c,d,
, Anna Rodó-Pina,b,c, Clara Espinaf,b,c, María Araceli Caballero-Rabascog,c, Pilar Ausine,b,c, Antonio Sancho Muñoze,b,c, Julia Precklerh,i, Mireia Admetllóe,b, Ester Marco Navarroh,i, Jacinto García-Lorenzof,b,c
Corresponding author
a Cardiopulmonary Exercise Testing Laboratory, Pulmonology Department, Hospital del Mar-Barcelona, Spain
b Hospital del Mar Research Institute, Barcelona, Spain
c Department of Medicine and Life Sciences (MELIS), Universitat Pompeu Fabra (UPF), Barcelona, Spain
d Centro de Investigación en Red de Enfermedades Respiratorias, (CIBERES), Instituto de Salud Carlos III (ISCIII), Barcelona, Spain
e Specialized Asthma Unit, Pulmonology Department, Hospital del Mar, Barcelona, Spain
f Otorhinolaryngology Department, Hospital del Mar, Barcelona, Spain
g Pediatric Allergy and Pulmonology Unit, Pediatric Service, Hospital del Mar, Barcelona, Spain
h Department of Physical Medicine and Rehabilitation, Hospital del Mar, Hospital de l’Esperança, Barcelona, Spain
i Rehabilitation Research Group, Hospital del Mar Research Institute, Barcelona, Spain
Ver másThis item has received
Article information
These are the options to access the full texts of the publication Archivos de Bronconeumología