Historically, it has been assumed that Intermediate Respiratory Care Units (IRCU) were efficient, because they saved costs by reducing the number of admissions to intensive care units (ICU), and effective, because they specialized in respiratory diseases.
MethodsThe number of IRCU admissions and mortality rate, historically and in 2016, were evaluated. For 2016, the grouped Related Diagnostic Groups (DRGs) were also described, and the savings achieved under all budgetary headings by avoiding UCI stays were calculated. A multivariate analysis was performed to associate costs with mean weights and complexity, and multiple logistic regression was performed on all patients admitted from 2004 to 2017 to describe the variables associated with mortality in our unit.
ResultsAn IRCU generates savings of €500,000/year by reducing length of ICU stay. Analysis of the 2016 cohort shows that costs correlate with mean weight and mortality, and consequently complexity. The multivariate logistic regression analysis of the 2004–2017 cohort found respiratory frequency, leukopenia, anemia, hyperkalemia, and acidosis to be the variables best associated with mortality. The area under the curve for the logistic model was 0.75.
ConclusionThe IRCU analyzed in our study was efficient in terms of ‘avoided costs’ and savings associated with complexity. Our results suggest that IRCUs have a lower mortality rate than other similar units, and are therefore a safe environment for patients.
Históricamente se ha asumido que las unidades de cuidados intermedios respiratorios (UCIR) eran estructuras eficientes por los costes evitados atribuibles a la reducción de los ingresos en las unidades de cuidados intensivos (UCI) y eficaces por la especialización neumológica.
MétodosSe evaluó el número de ingresos y mortalidad en la unidad, histórica y en el año 2016. Ese año además se describieron los grupos relacionados de diagnóstico (GRD) agrupados y el coste evitado por estancia en UCI en relación con todos los capítulos presupuestarios. Se realizó un análisis multivariante para asociar costes a pesos medios y complejidad y se realizó una regresión logística múltiple sobre la totalidad de enfermos ingresados de 2004 a 2017 para describir las variables asociadas a la mortalidad en nuestra unidad.
ResultadosLa UCIR evita un coste al hospital de 500.000€/año al reducir días de estancia en las UCI. El análisis sobre la cohorte de 2016 describe que los costes se asocian al peso medio y mortalidad, y por tanto, a la complejidad. El análisis de regresión logística multivariante sobre la cohorte de 2004–2017 describe la frecuencia respiratoria, la leucopenia, la anemia, la hiperpotasemia y la acidosis como las variables que mejor se asocian con la mortalidad. El área bajo la curva para el modelo logístico fue de 0,75.
ConclusiónLa UCIR analizada ha demostrado ser eficiente en términos de «coste evitado» y ahorro ligado a la complejidad. Nuestros resultados sugieren que las UCIR son un entorno seguro para los pacientes al tener una mortalidad menor que otras unidades similares.
An intermediate respiratory care unit (IRCU) is defined as an area for the monitoring and management of patients with acute respiratory failure requiring non-invasive ventilation (NIV)1 and/or high flow oxygen therapy as part of their treatment. These units can care for patients who do not require or will not benefit from admission to a normal ICU, but who are too complex to be appropriately treated in a conventional hospital ward.2 Up to 40% of patients admitted to an ICU do not require intubation, only 40% of cases of acute respiratory failure require invasive mechanical ventilation (IMV), and up to 60% of the time on IMV is dedicated to withdrawal or weaning,1 facts which might suggest that inappropriate use is being made of ICU resources. In Europe, only 9% of IRCUs are physically situated within the general ICU, although that rate is increasing globally.3 Most units are currently either integrated within the respiratory medicine area (59%), or are set up in a separate unit (25%).4,5
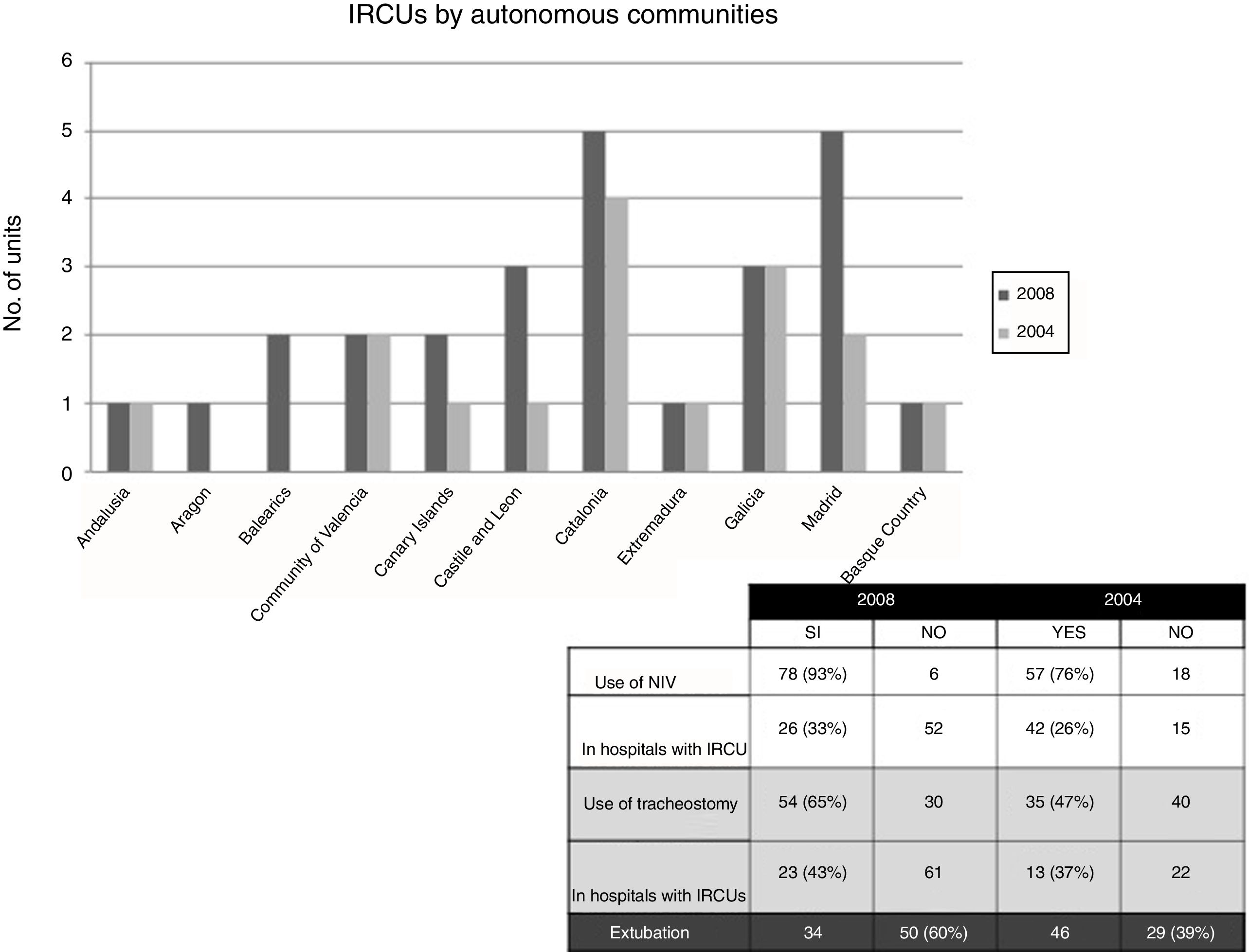
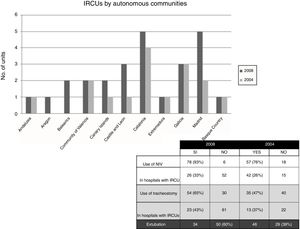
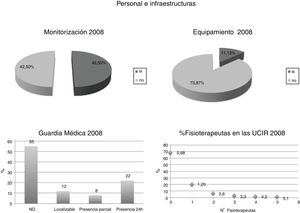
In the specific case of Spain, the extent to which IRCUs have been implemented was first defined in 2 surveys conducted by the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR) in 20046 and 2008.7 These surveys found, in the first place, that the number of these units in the different autonomous communities had increased by approximately 10%, and that 78% of these units were set up as part of the respiratory medicine department.
Secondly, these surveys also showed an increase in the use of NIV and IMV via tracheostomy in these units, in which the average number of beds remained stable at 4 per unit (Fig. 1).
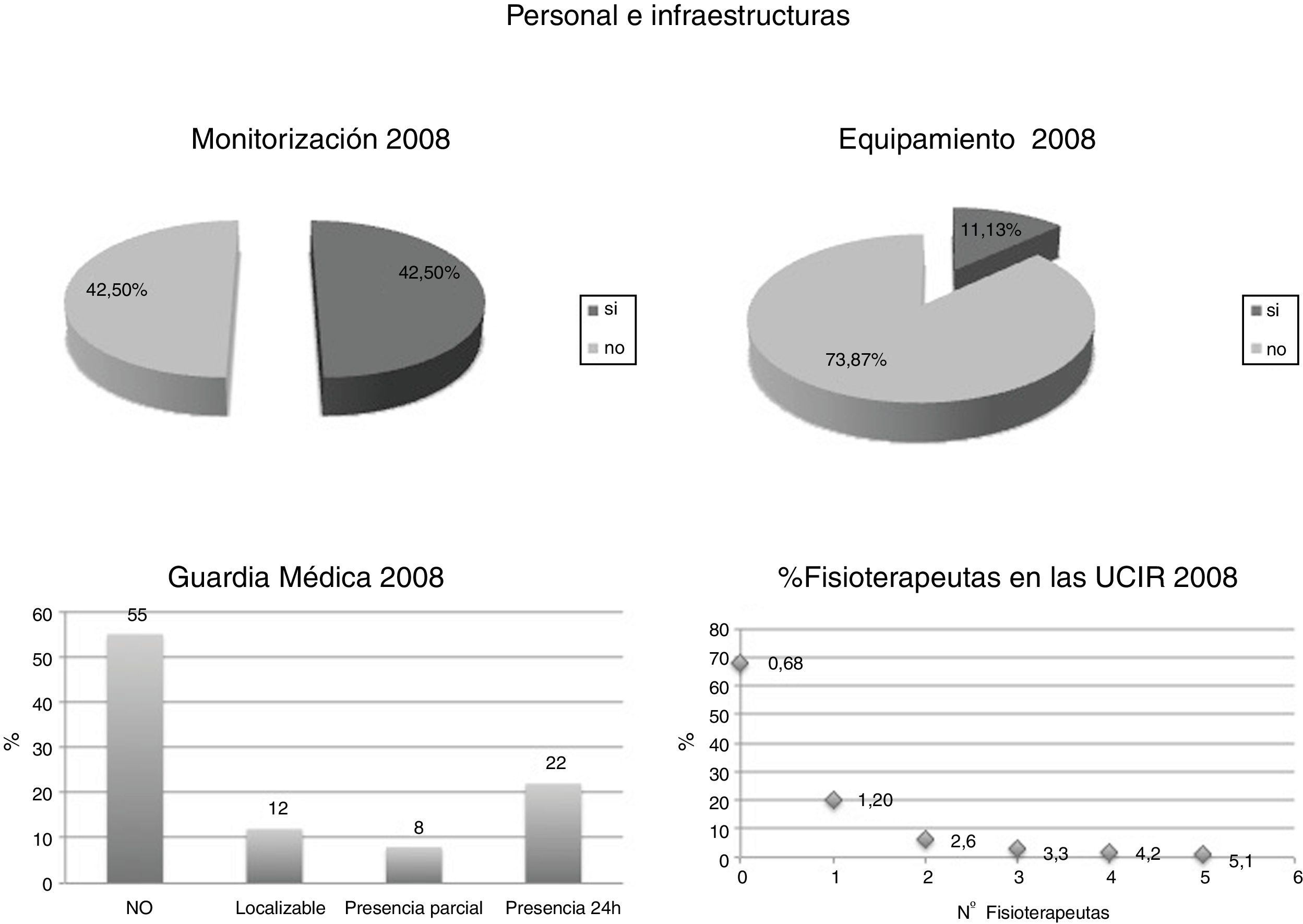
An analysis of the characteristics of the units that had been created in the intervening 4 years showed that 64% of the new IRCUs did not have internal medicine residents, 68% did not have their own physical therapist, and up to 55% did not have any on-call rosters in place. In 2008, half of the IRCUs lacked monitoring protocols and 87% did not have the recommended equipment at their disposal. Thus, the increase in the number of units was not accompanied by an improvement in human resources or materials (Fig. 2).
The implementation of IRCUs is still not universal in our setting, and in the absence of high complexity intermediate care units, many patients who might not need full ICU care continue to be managed in these units. This increases health care spending and limits the use of appropriate resources in each case. The objective of this study was to perform a cost analysis of an IRCU set up within a general hospital, to determine the annual expenditure associated with complexity and potential efficiency in terms of avoided cost. To this end, we analyzed the costs attributable to 2016 and estimated the cost if the patients had been admitted to the ICU of our hospital. Additionally, as secondary objectives, we analyzed the factors most closely associated with expenditure to determine their impact on the final cost, and the mortality rate of the unit in that year and since it was set up, in order to isolate predictors of mortality in the unit.
Materials and MethodsThe study and analysis of patient data were approved by the Ethics Committee of the Hospital Universitario Fundación Jiménez Díaz (HUFJD).
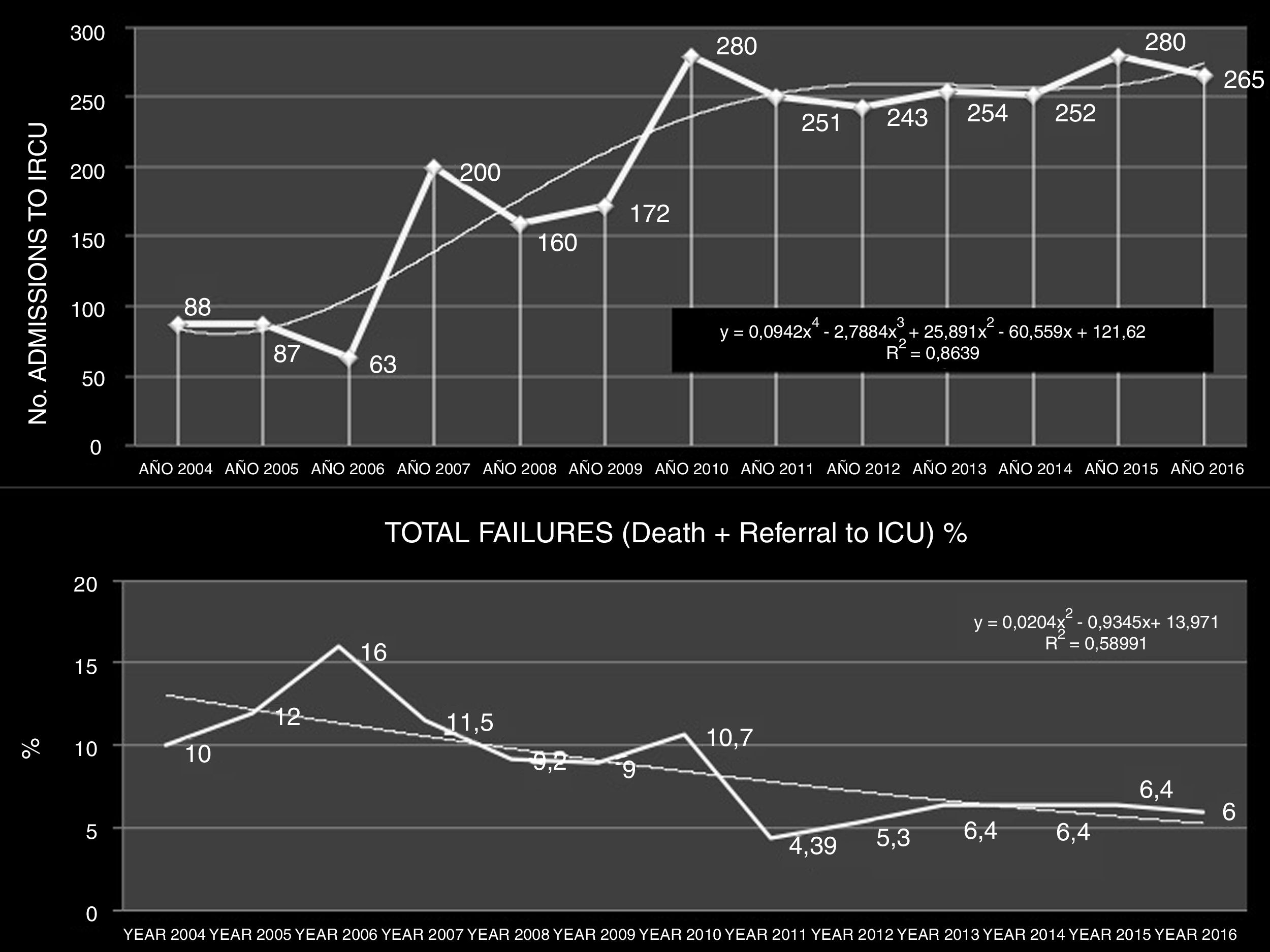
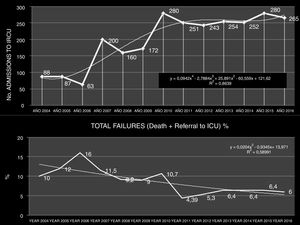
Unit CharacteristicsThe IRCU of the HUFJD analyzed in this study is a 5-bed unit that can be extended to accommodate 8 beds in periods of greater demand. Fig. 3 shows the unit admission numbers and failures (including death and referral to the ICU) since the year 2004.
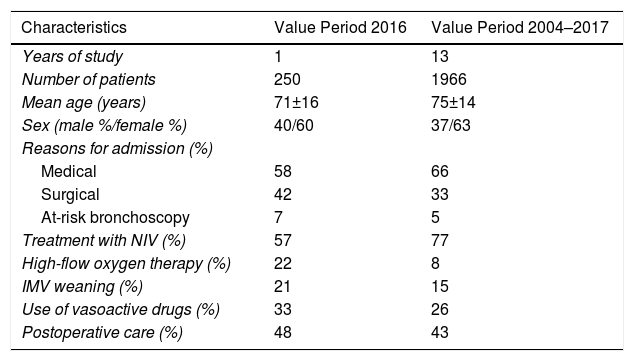
Analysis of the Costs of the Intermediate Respiratory Care Unit of the 2016 CohortA total of 250 patients were admitted to the unit in 2016. Their overall characteristics appear in Table 1. We calculated personnel costs, taking into account all existing staff on all shifts and the labor agreement currently in force.8 We accessed all data on the direct costs of all the corresponding items, categorized as healthcare materials and patient consumables (drugs and radiology, electricity), instruments, linen and clothing, and others (medicinal gases, power, cleaning, maintenance, office supplies, food, etc.).
General Profile of the 2016 Cohort and the Global 2004–2017 Cohort.
| Characteristics | Value Period 2016 | Value Period 2004–2017 |
|---|---|---|
| Years of study | 1 | 13 |
| Number of patients | 250 | 1966 |
| Mean age (years) | 71±16 | 75±14 |
| Sex (male %/female %) | 40/60 | 37/63 |
| Reasons for admission (%) | ||
| Medical | 58 | 66 |
| Surgical | 42 | 33 |
| At-risk bronchoscopy | 7 | 5 |
| Treatment with NIV (%) | 57 | 77 |
| High-flow oxygen therapy (%) | 22 | 8 |
| IMV weaning (%) | 21 | 15 |
| Use of vasoactive drugs (%) | 33 | 26 |
| Postoperative care (%) | 48 | 43 |
IMV: invasive mechanical ventilation (tracheostomy weaning); NIV: non-invasive ventilation.
The consumption of pharmaceuticals was categorized according to use, measured in single doses. Equipment that was fully amortized, and therefore had no depreciable value, was not included in the inventory.
The medical histories of the 250 patients admitted in 2016 were reviewed and all clinical laboratory tests and all radiological tests carried out in that year were taken into account.
To analyze costs avoided by the IRCU, we calculated the annual mean length of stay in the unit, and attributed to this period the theoretical bed cost per day estimated for ICU tier 1, according to the classification of the Ministry of Health, which distinguishes 3 tiers of ICU complexity.9 The avoided cost was taken as the difference between the real cost calculated for the IRCU (Table 2) and the estimated cost for the ICU.
The possible relationship between each of the variables (weight, length of stay, level of disease, and mortality levels) and costs were analyzed statistically using linear regression models.
Predictors of Mortality in the Intermediate Respiratory Care Unit in the 2004–2017 CohortThe possible relationship between each of the variables (Diagnosis Related Groups [DRG], length of stay, disease level, and mortality level) and mortality was analyzed using Poisson regression models. This model reflects IRCU mortality from 2004 to 2017. This procedure was used to analyze relative risk (RR), standard error, 95% confidence interval, and the p value of each variable, to determine if any was related to mortality. A univariate logistic regression model was then performed using data collected on admission. ROC curves and Youden's J statistic were used to obtain the cut-off point that best predicted mortality for each of the variables. A binary classification was defined for each parameter as a function of the cut-off points and the selected parameters (p<0.05) to run the multivariable logistic regression model. The “forward stepwise” method was used to build the multivariate model. Only statistical significance, and not clinical relevance, was taken into account for the construction of the model. The area under the curve (AUC), sensitivity, and specificity were calculated using a ROC curve corresponding to the multivariate model, which reports on the predictive capacity of this model. The internal validation of the model was determined using the bootstrap method, and goodness-of-fit using the Hosmer–Lemeshow test.
ResultsUnit CharacteristicsA total of 250 patients were admitted in 2016, with a total of 1390 days of stay. The mean DRG in the year 2016 for the IRCU was 3.59±2.59. Mean stay was 5.62 days. The severity level was 3.44±0.58, and the mortality rate was 3.36±0.77 (both assessed on a scale of 1–4).10Fig. 3 shows the increase in the number of admissions over time between 2004 and 2017 and the stability achieved in mortality figures for the same period. Table 1 summarizes the characteristics of the 2016 cohort.
Analysis of the Costs of the Intermediate Respiratory Care Unit of the 2016 CohortAdditional material includes data on the equipment and infrastructure of the unit (Appendix B, Table 1, additional material), current criteria for admission (Appendix B, Table 2, additional material) and general characteristics of patients classified by DRG (Appendix B, Table 3, additional material).
Appendix B, Tables 4–8 of the additional material show IRCU costs in 2016 for the headings human resources, consumption, and pharmaceutical and radiology costs, respectively.
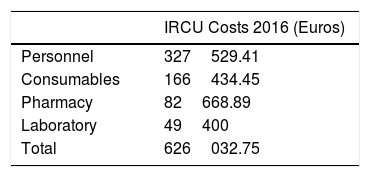
The total annual cost of the IRCU in 2016, calculated as the sum of the described categories, amounted to €626,032.75 (Table 2).
The IRCU saved the hospital 1390 days of ICU stays, with a theoretical value between €969066.30 (Tier 3: €697.17/day) and €1119450.40 (Tier 1: €805.36/day, used in the present study). Taking into account the actual cost of the IRCU (Table 2), the real avoided annual cost is estimated at between $343033.55 and €493417.65/year.
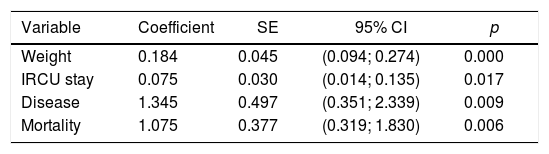
The analysis of the variables that were most closely associated with costs was made separately using univariate models in which each variable was analyzed independently compared to the cost factor (Table 3); it was observed that all variables of the model, mean weight, mean stay, disease level, and mortality level were associated with costs. Subsequently, when all variables were entered as a whole, an overall multivariate model was obtained that detected the variables that had a stronger association with costs (Table 4), with the result that mean weight and complexity were the variables most strongly associated with costs.
Univariate Analyses.
| Variable | Coefficient | SE | 95% CI | p |
|---|---|---|---|---|
| Weight | 0.184 | 0.045 | (0.094; 0.274) | 0.000 |
| IRCU stay | 0.075 | 0.030 | (0.014; 0.135) | 0.017 |
| Disease | 1.345 | 0.497 | (0.351; 2.339) | 0.009 |
| Mortality | 1.075 | 0.377 | (0.319; 1.830) | 0.006 |
Results of the univariate linear regression models created to analyze which variables are independently associated with costs and which are not. The costs variable has been transformed into logarithms, because it presents a strong positive asymmetry, customary in many distributions of economic data. As a general rule, a log transformation is used to operate linear regressions with this type of data, in order to provide a symmetrical distribution close to normal. Because the data were aggregated, the regression models have been estimated taking as weights the number of episodes of each DRG. We see that all variables are statistically significant (p<0.05), suggesting that all variables are associated with costs.
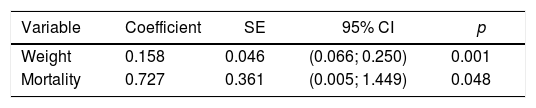
Multivariate Analyses.
| Variable | Coefficient | SE | 95% CI | p |
|---|---|---|---|---|
| Weight | 0.158 | 0.046 | (0.066; 0.250) | 0.001 |
| Mortality | 0.727 | 0.361 | (0.005; 1.449) | 0.048 |
Multivariate model which is achieved when all variables are used in combination. The variables most strongly linked to costs are average weight and mortality.
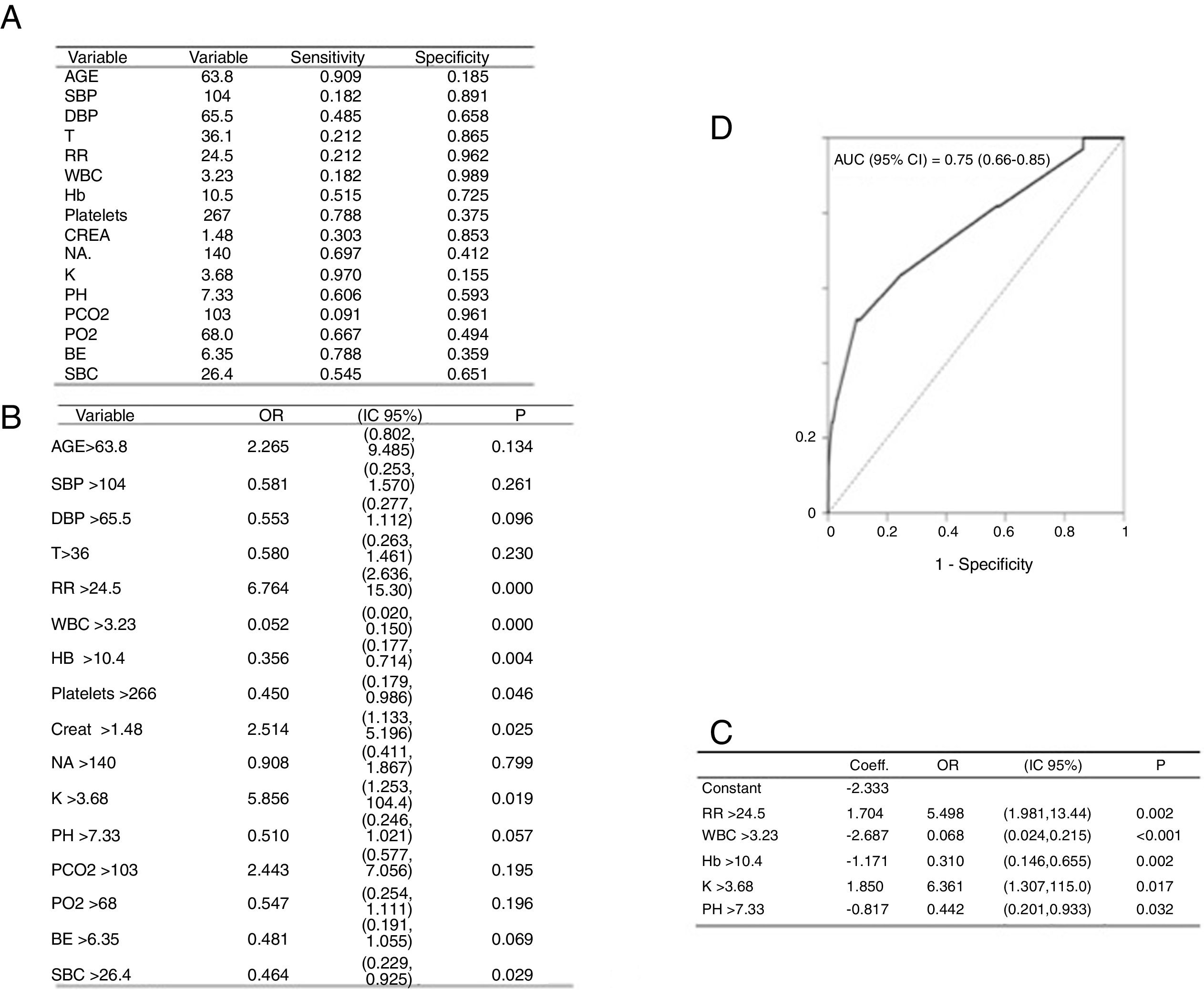
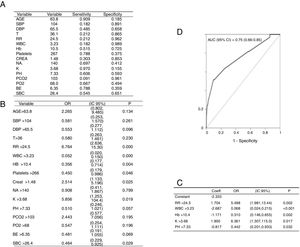
The 2004–2017 cohort is described in Table 1. The Poisson regression model collects IRCU mortality in the period from 2004 to 2017 (Table 5), showing that none of the variables analyzed is individually associated with mortality. The variables are described in Table 6. The univariate logistic regression model with the data collected at admission is shown in Fig. 4A and B. The multivariable logistic regression model is shown in Fig. 4C. AUC, sensitivity, and specificity were calculated using a ROC curve (Fig. 4D). The bootstrap internal validation indicated an optimism of 0.016, which reflects the robustness of the model, and goodness-of-fit using the Hosmer–Lemeshow test was satisfactory, finally showing that respiration rate (RR), leukocyte count (WBC), hemoglobin (Hb) value, potassium (K), and pH are the variables that, combined, discriminate best between classes (Fig. 4C). The area under the curve for the logistic model was 0.75 (Fig. 4D).
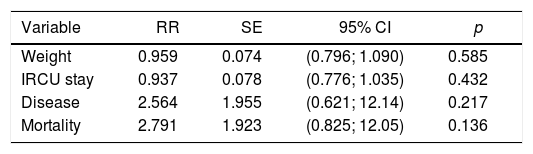
Relationship Between Each of the Variables (Weight, Length of Stay, Disease Level, and Mortality Level) and Deaths.
| Variable | RR | SE | 95% CI | p |
|---|---|---|---|---|
| Weight | 0.959 | 0.074 | (0.796; 1.090) | 0.585 |
| IRCU stay | 0.937 | 0.078 | (0.776; 1.035) | 0.432 |
| Disease | 2.564 | 1.955 | (0.621; 12.14) | 0.217 |
| Mortality | 2.791 | 1.923 | (0.825; 12.05) | 0.136 |
In no case do the variables appear to be associated with the number of deaths.
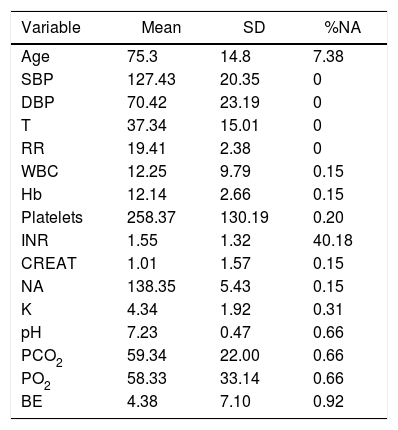
Description of Variables of the 2004–2017 Cohort.
| Variable | Mean | SD | %NA |
|---|---|---|---|
| Age | 75.3 | 14.8 | 7.38 |
| SBP | 127.43 | 20.35 | 0 |
| DBP | 70.42 | 23.19 | 0 |
| T | 37.34 | 15.01 | 0 |
| RR | 19.41 | 2.38 | 0 |
| WBC | 12.25 | 9.79 | 0.15 |
| Hb | 12.14 | 2.66 | 0.15 |
| Platelets | 258.37 | 130.19 | 0.20 |
| INR | 1.55 | 1.32 | 40.18 |
| CREAT | 1.01 | 1.57 | 0.15 |
| NA | 138.35 | 5.43 | 0.15 |
| K | 4.34 | 1.92 | 0.31 |
| pH | 7.23 | 0.47 | 0.66 |
| PCO2 | 59.34 | 22.00 | 0.66 |
| PO2 | 58.33 | 33.14 | 0.66 |
| BE | 4.38 | 7.10 | 0.92 |
INR: international normalized ratio.
% NA (Not Available) indicates the values that are not available for each variable. Clinical variables included respiratory rate (RR), temperature (T), systolic blood pressure (SBP), and diastolic blood pressure (DBP). The laboratory findings included hemoglobin (Hb), platelets, leukocytes (WBC), blood glucose (GLU), potassium (K), sodium (NA), and creatinine (CREAT). Arterial blood gases were also recorded at the time of hospital admission (FiO2 21%) with partial pressure of oxygen (PO2), partial pressure of carbon dioxide (PCO2), PH, bicarbonate (SBC), and excess base (EB). Patient clinical history data were also used, including age and mortality or individual survival at IRCU discharge.
(A) Outcomes with qualitative predictors: Cut-off points obtained with ROC curves (Youden criterion). (B) Univariate logistic regression models, cut-off variables. (C) Multivariate logistic regression models, model coefficients. (D) The area under the curve indicates that the model has an acceptable discrimination capacity. Bootstrap validation provides a loss of predictive capacity somewhat less than 1.6%, so the model seems quite reliable.
The cost analysis of the IRCU under study suggest that this type of unit generates economic savings that can be considerable, mainly in terms of avoided costs, while maintaining a low mortality rate.
The IRCU manages highly complex patients, whose main mode of treatment is NIV, IMV via tracheostomy, or high flow oxygen therapy. Costs are avoided by the fact that this type of IRCU averts prolonged or unnecessary ICU stays.
This analysis is based on the concept of “avoided costs”, i.e., savings that are implicit to the appropriate use of different levels of hospital care and management. In 2016, the overall stay of the 250 patients admitted to the IRCU amounted to 1390 days. Due to their complexity, in the absence of an IRCU, those patients would have been admitted to the ICU.
On the other hand, if the ICU resources had not been available, some of these patients would have been treated in a conventional hospital ward. Hospital wards provide care to patients of medium complexity at a level of care clearly inferior to that offered by the IRCU. These patients, therefore, would not receive the level of support that they require.
We do not know the exact cost of a day of stay in the ICU of our hospital. For this reason, we used as a reference the Ministry of Health report, which sets the average associated cost per day of stay in the ICU of public hospitals in Madrid at €805.36 for tier 1 hospitals,11,12 which would apply to our center. Therefore, the analysis of avoided cost is an estimate, and should be taken as a limitation of this study.
According to the data collected, we can conclude that the IRCU saved the hospital a cost of 1390 days of ICU stay, with a theoretical value of €805.36/day. Taking into account the cost of the IRCU itself, the final annual cost avoided would be close to €493417.65/year. The concept of avoided cost should not only be viewed from an economic angle. Consideration should be given to the added value of the potentially improved capacity for ICU admissions and all that this implies in the organization of highly complex medical and surgical activity. This represents an additional benefit that we have not quantified, although it has been described in other studies.13–16
The multivariate models indicate that costs are associated primarily with mean DRG and mortality: in brief, the complexity of the patient. Therefore, we believe that the comparative analysis proposed would not be valid if the average complexity of patients seen in the IRCU were as low as the DRG levels that could be managed in a conventional hospital ward. In short, this study confirms that a high complexity IRCU avoids a greater number of ICU stays and is associated with greater cost savings.
Very few studies have addressed the theoretical efficiency associated with the availability of an IRCU in the care process. A systematic review of the literature identified only 3 studies with economic analyses, all of which reported on respiratory intermediate care units. In one of these studies, the authors concluded that data were insufficient to determine whether IRCUs “are a cost-effective alternative technology to the traditional institution with only ICU and general ward beds”.17 In another more recent prospective study, Bertolini et al.18 reported that in the management of highly complex chronic obstructive pulmonary disease exacerbations, the total cost per patient was lower in a respiratory IRCU than in an ICU. Finally, Byrick et al.19 raised concerns about the increasing numbers of less complex patients being admitted to the ICU and short stays with low nursing workload that occurred when an IRCU in a Canadian hospital was closed for budgetary reasons. These findings were indicative of an inefficient use of staff and resources, and the IRCU subsequently had to be reopened.
The DRG of the IRCU analyzed in our study is very high compared with that of the general respiratory medicine wards of the same hospital (DRG-IRCU 3.5 vs DRG-RMD ward 1.12), and lower than that of the conventional ICU (DRG-IRCU 3.5 vs DRG-ICU 5.8).20 The lowest DRG values recorded in our cohort correspond primarily to patients who were admitted due to the need for continuous monitoring of their vital signs. The average length of stay, quantified at 5.63 days, is very competitive, despite being influenced by patients being referred from the ICU due to slow or complex weaning. These patients account for 16% of the total number of patients admitted and have an average DRG value of between 4 and 5, which represents 19.35% of the overall stay in the unit. In the absence of an IRCU, these patients would have remained in the ICU, and it is precisely this change of setting that is associated with cost savings for the hospital, with no increase in mortality.
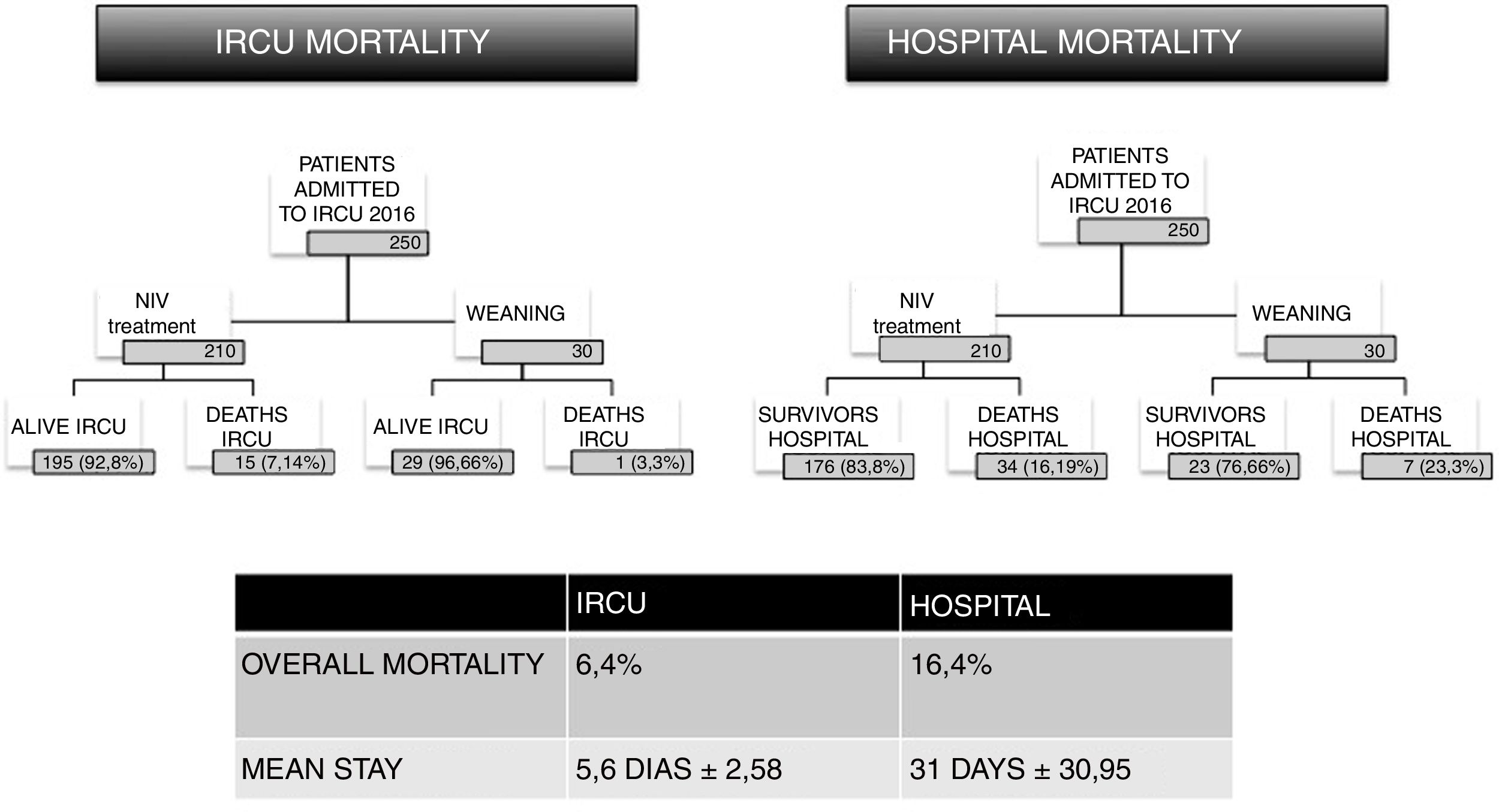
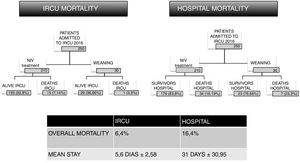
In the analysis of any clinical unit, favorable economic data must be accompanied by robust indicators of quality of care. In this study, we also analyzed IRCU mortality. In 2016, 16 of the 250 admitted patients died. These patients had an average severity score of 3.625, according to the 1–4 severity scale (Appendix B, Table 4, additional material) and a probability of death due to complexity of 3.8125 (1–4 mortality scale). The mortality rate for the unit has remained stable since 2009, at an average of 6.4%. This figure is in line with other studies21 that have shown that the existence of an IRCU decreases hospital mortality.22 Data from patients treated with NIV and from those requiring IMV via tracheostomy were analyzed separately, and equally optimistic rates were obtained. A European study published in 2016 describes a mortality rate associated with IMV of 30%,23 while in the IRCU analyzed here, only 15 deaths out of 210 patients (7.14%) occurred for this reason. With regard to tracheostomies and IMV weaning, mortality in this group of patients, according to the latest multicenter study from 2015, was 30%–38%,24 compared to 3.3% (1 of 30 patients) in our IRCU.
Patients are not discharged home from the IRCU, however, and after stabilization and completion of IMV weaning, they return to their original wards, where delayed mortality may occur (Fig. 5). In the cohort of 250 patients analyzed in 2016, follow-up after the IRCU stay revealed that an additional 41 subjects died, implying an overall global mortality of 16%, which is also lower than the European average. When the mortality of each group is analyzed separately, the use of NIV was associated with 34 deaths in 210 subjects, i.e., 16.19% (in Europe, the rate is 30%23); for the 30 cases of weaning after tracheostomy, 7 deaths were recorded (all of them in hospital wards after discharge from the IRCU), i.e., 23%, also below the European average of 30%–38%.24 With respect to predictors of mortality on admission, the Poisson regression found no association among the variables analyzed in this study. A multivariate logistic regression analysis was performed on the 19 clinical variables at admission that reflect a greater mortality in patients with hematologic alterations, tachypnea, and acidosis. These data are consistent with those reported previously in other studies.25
ConclusionAn IRCU, such as the one analyzed in this study, avoids ICU admission and, as such, generates considerable savings in critical respiratory care. As a result, hospital resources can be better distributed. If the IRCU offers highly complex care, then savings are even more significant. Our study also shows that an IRCU is a safe environment that achieves low mortality rates, despite the complexity of admitted patients.
FundingThis study has not received specific support from public sector agencies, or commercial or non-profit organizations.
Conflict of InterestsThe authors state that they have no conflict of interests.
We thank all the members of the Respiratory Medicine Department of the Hospital Fundación Jiménez Díaz IIS for their ongoing support, the management and directors of the Fundación Jiménez Díaz for their help in the preparation of this article, and the Director of Healthcare Assessment, Dr Augustín Albarracín Sierra. We also thank the ESADE Business and Law School for their training in management, and Jose Fernández Arias for his commendable data collection efforts.
In memoriam: Dr Charo Melchor Iñiguez, who we admire and remember with affection.
Please cite this article as: Heili Frades S, Carballosa de Miguel MP, Naya Prieto A, Galdeano Lozano M, Mate García X, Mahillo Fernández I, et al. Análisis de costes y mortalidad de una unidad de cuidados intermedios respiratorios. ¿Es realmente eficiente y segura? Arch Bronconeumol. 2019;55:634–641.