Specialised medical care at district hospitals has not been thoroughly defined. Respiratory care data from 2008 in Barbanza and Cee hospitals (Galicia, Spain), were analysed to evaluate different approaches, as they are both similar. Barbanza hospital has a chest diseases clinic run by specialist doctors from the reference hospital three days per week, while Cee hospital is operated by the staff on site. In both cases hospitalisation is the responsibility of the Internal Medicine department. Data was provided by the administrative departments of each hospital and the regional government.
Average CDM4 stays were similar for both district hospitals; however, they were lower than in the reference hospital. Charlson scores and re-admissions a month after discharge were similar in both. Barbanza's hospital carried out more functional explorations, both at the centre (957 spirometries vs. 21; P<.0001) and at the reference hospital (214 volume/diffusion tests vs. 99; P<.001). CPAP treatments were more prevalent in the Barbanza area (3.9 vs. 2/1000 habitants; P<.0001). No differences were found in oxygen therapy and home mechanical ventilation. Mortality due to respiratory disease in 2007 was similar in both regions.
Data suggests that in a district hospital scheme supported by chest disease consultants and outpatient clinics gives easier access to specialised, comprehensive and probably, higher quality care than district hospitals without them.
No está bien definida el tipo de asistencia especializada que deben dar los hospitales comarcales. Para evaluar diferentes opciones, se analizó retrospectivamente la atención neumológica en el año 2008 en dos áreas comarcales de Galicia: Barbanza y Cee, con características poblacionales similares. El hospital de Barbanza dispone de consulta de neumología atendida por especialistas del hospital de referencia 3 días/semana, mientras que en Cee la atienden internistas del propio centro. En ambos casos, la hospitalización está a cargo del servicio de Medicina Interna. Los datos fueron proporcionados por los servicios administrativos de los hospitales y autonómicos.
Las estancias medias para el agrupador CDM4 fueron similares en los dos comarcales, pero inferiores a las de los centros de referencia. No hubo diferencias en comorbilidad (Charlson) ni en reingresos al mes de alta. Se realizaron más exploraciones funcionales en pacientes del Barbanza, tanto en el propio centro (957 espirometrías vs. 21; p<0,0001) como en el hospital de referencia (214 determinaciones de volúmen/difusión vs. 99; p<0,001). La prevalencia de tratamientos con CPAP fue más elevada en el área de Barbanza (3,9 vs. 2/1.000 habitantes; p<0,0001). No encontramos diferencias en la prevalencia de oxigenoterapia ni en ventilación mecánica domiciliaria. La mortalidad por patología respiratoria el año 2007 fue similar en las dos áreas.
Estos datos sugieren que en un modelo de hospital comarcal con neumólogos consultores, la consulta ambulatoria facilita el acceso a una asistencia más especializada, más completa y, probablemente, de más calidad, que los comarcales sin este tipo de consultoría.
The geographical location and the cultural expectations in the context of health are important factors in the perception of the quality of health-care services. On the other hand, aging and chronic processes, especially respiratory ones, mean that rural populations are especially sensitive to health-care limitations. District hospitals are able to overcome the territorial imbalance and reduce the difficulties in accessing the health-care system of those towns that are far from metropolitan areas at a reasonable cost.1 With limited services, these centers should resolve their needs for specialized attention in coordination with reference hospitals.2 However, as in other communities, in the Servizo Galego de Saúde (Galician Health-Care Administration - Sergas) there is no defined model relating the district centers with reference hospitals. Thus, while some have a pulmonologist on staff, other hospitals are visited by specialists that travel out from the reference hospital, while at others it is the patients who are sent to the reference centers for consultations with specialists.
There are no data to support which is the ideal system, therefore this present study compares the models of coordination of the district hospitals that do not have a pulmonologist on staff with the aim of objectively identifying elements in order to design applicable options.3
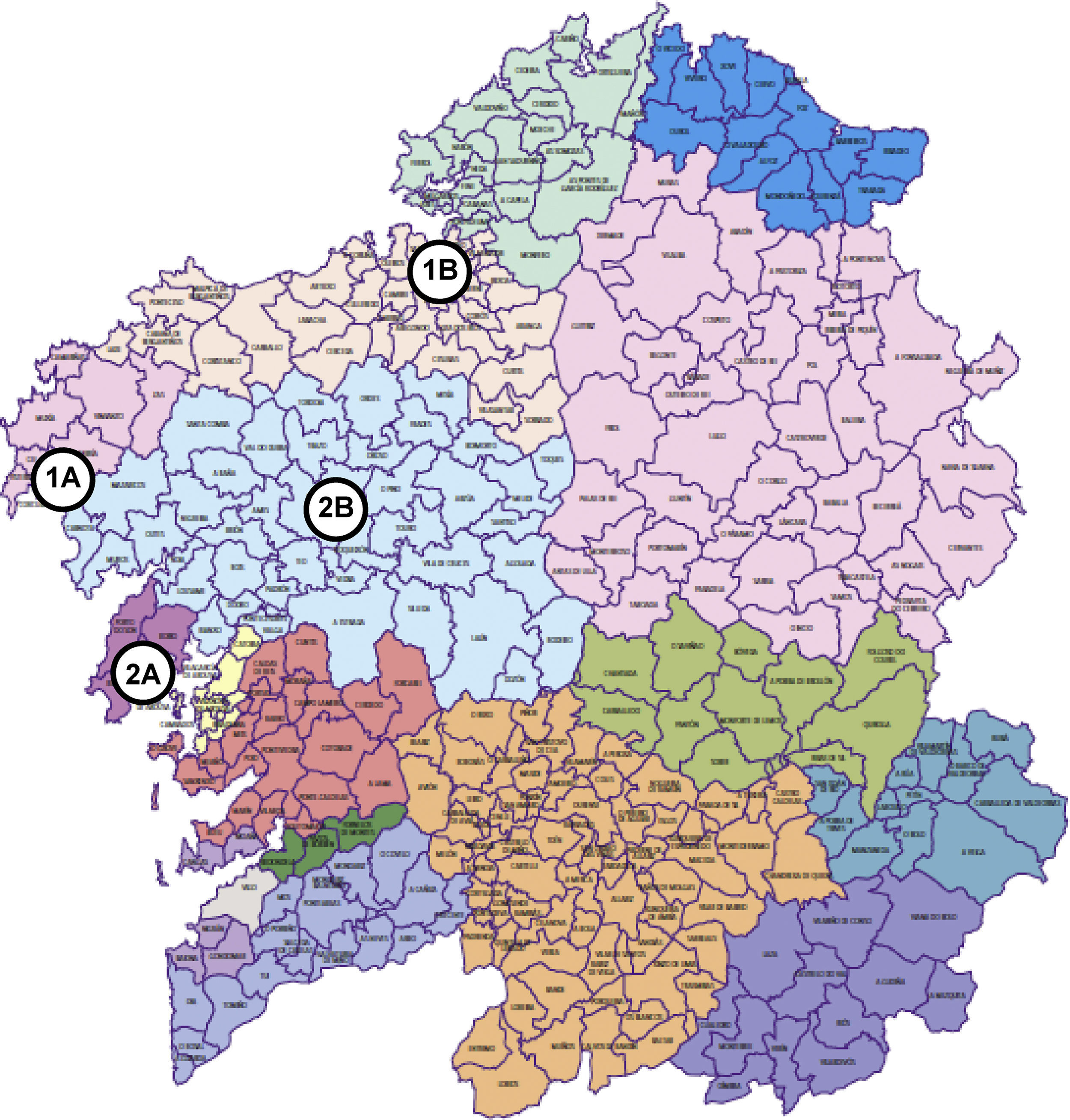
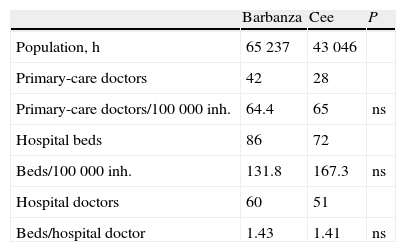
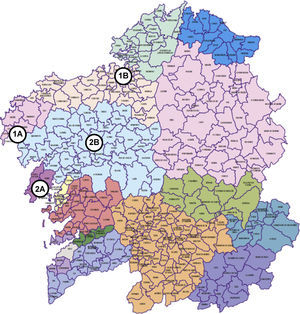
Material and MethodsMaterialThe health-care areas being studied correspond to the district hospitals of Barbanza and Cee (Fig. 1), situated in the towns of Ribeira and Cee, respectively, in the province of A Coruña in north-west Spain. The area of Barbanza occupies four coastal municipalities, with a population of 65,237 inhabitants (2% of the Galician population) and 10 primary-care centers staffed by 42 physicians (Table 1). The district hospital has 60 doctors (none of which is a pulmonologist), 86 beds and has helical computed tomography (CT) equipment available. It has a pulmonology examination room equipped with a spirometer (Pony FX Cosmed) and possibilities for blood gas analysis, where a pulmonologist who travels from the reference hospital, the University of Santiago Hospital Complex (CHUS, its acronym in Spanish), sees patients 10 days per month. Patients who are referred for consultation are remitted by a physician of the area (Emergency, Primary Care or a hospital doctor). In the event that more complex or invasive tests are needed, these are done in the Pulmonology Department at CHUS (70 km from Ribeira).
Population and availability of health-care in the district areas of Barbanza and Cee.
| Barbanza | Cee | P | |
| Population, h | 65237 | 43046 | |
| Primary-care doctors | 42 | 28 | |
| Primary-care doctors/100000 inh. | 64.4 | 65 | ns |
| Hospital beds | 86 | 72 | |
| Beds/100000 inh. | 131.8 | 167.3 | ns |
| Hospital doctors | 60 | 51 | |
| Beds/hospital doctor | 1.43 | 1.41 | ns |
inh.: inhabitants; ns: not significant.
The health-care area of Cee includes seven coastal municipalities (42843 inhabitants, 1.6% of the population of Galicia). It has 14 primary-care centers with 28 physicians (Table 1). The district hospital is Virxe da Xunqueira, in the town of Cee, with 72 beds. It has a helical CT and a spirometer (Spirolab II MIR) available, and 51 doctors on staff. There are no pulmonologists, nor is there a specific pulmonology examination room in the center. Internal Medicine specialists or Primary care physicians of the area have interconsultations with the Pulmonology Department at the University of A Coruña Hospital Complex (CHUAC, in Spanish) (100 km from Cee) referring their patients as appointments are given.
MethodsThe health-care administration information from 2008 was facilitated by the Departments of Admission and Management of the hospitals and the Codification Department of Sergas, independently and without the interference of the authors of this present study, except for the statistical analysis. Hospitalization data were obtained for respiratory disease, activities and techniques carried out in the outpatient consultations in both district hospitals, and the derivations to the reference hospitals. The number of hospital discharges was compiled, as well as the mean hospital stay for all the patients admitted for major diagnostic category 4 (MDC 4) and for the diagnosis-related group (DRG), as well as comorbidities and re-hospitalizations within 30 days. The comorbidities were quantified by the Charlson index.4 The information on the prescriptions for oxygen therapy, home breathing devices for continuous positive airway pressure (CPAP), ventilators and aerosol therapy was supplied by the company that was awarded the concession for providing these services in the province of A Coruña (Oximesa SL).
Statistical AnalysisThe normal distribution of the data was verified by means of the Kolmogorov-Smirnov test. The independent proportions were compared with the Z method. The Gaussian distribution data were expressed as mean±standard deviation. For comparisons, the Student's t test was used, applying the Levene test to verify the homogeneity of variances. For the comparison of categorical variables, the chi-squared test was used. The Epidat 3.1 program was utilized, as was the Statistical Package for Social Sciences (SPSS, Chicago, IL, USA), version 15.0 in Spanish.5
ResultsTable 1 shows the characteristics of the areas of Barbanza and Cee. There are no differences in the number of general medicine physicians /100000 inhabitants, hospital beds /100000 inhabitants, or in the ratio of beds / hospital doctors. In the hospital of Barbanza, there were 483 initial pulmonology consultations, with a successive/initial consultation ratio of de 2.69 and mean time elapsed of 40 days. Although the hospital in Cee has no data available on the pulmonary pathologies treated in the outpatient consultations, the generic reference for internal medicine was 907 initial consultations, with a successive/initial ratio of 1.91 with a time elapsed of 75.7 days. In Barbanza, 957 spirometries were performed and 21 were done in Cee (P<.0001).
The interconsultations with the reference centers were: from Barbanza to CHUS 156, and from Cee to CHUAC 161, with a successive/initial ratio of 2.96 and 2.79, respectively (P=ns). In the reference hospitals, 187 spirometries were performed on patients from Barbanza and 376 on patients from Cee. The most complex tests (volumes and diffusion) were 214 and 99, respectively (P<.001). In CHUAC, 43 bronchoscopies were carried out in Cee patients, 21 of these with indications of neoplasm. Nineteen patients from Barbanza underwent bronchoscopy due to the suspicion of a tumor (we do not know the total number of bronchoscopies done for other indications).
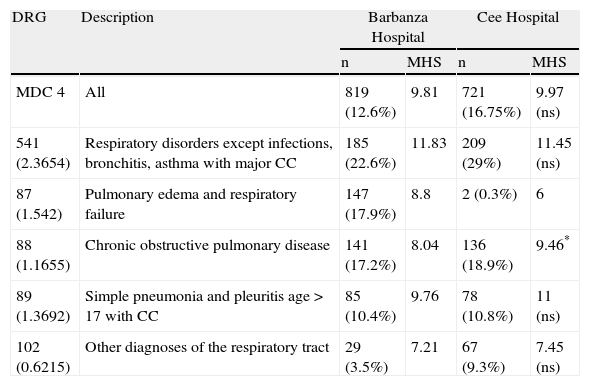
Table 2 details the discharges of patients with diagnoses cataloged as MDC4, grouped by DRG, in the hospitals of Barbanza and Cee in 2008. There is no difference in the mean hospital stay of the total number of cases, although there is in those included in DRG 88 (defined as chronic obstructive pulmonary disease), which was 8.04 days in Barbanza and 9.46 in Cee (P=.006). No significant differences were found either in the number of re-hospitalizations within one month of discharge in the two districts (7.2% [59/819] in Barbanza, compared to 9.15% [66/721] in Cee) or in comorbidities (Charlson index 2.227±1.642 in Barbanza vs 2.246±1.533 in Cee).
Patients discharged with MDC 4 and the five most frequent DRGs in the hospital of Barbanza and Cee in 2008.
| DRG | Description | Barbanza Hospital | Cee Hospital | ||
| n | MHS | n | MHS | ||
| MDC 4 | All | 819 (12.6%) | 9.81 | 721 (16.75%) | 9.97 (ns) |
| 541 (2.3654) | Respiratory disorders except infections, bronchitis, asthma with major CC | 185 (22.6%) | 11.83 | 209 (29%) | 11.45 (ns) |
| 87 (1.542) | Pulmonary edema and respiratory failure | 147 (17.9%) | 8.8 | 2 (0.3%) | 6 |
| 88 (1.1655) | Chronic obstructive pulmonary disease | 141 (17.2%) | 8.04 | 136 (18.9%) | 9.46* |
| 89 (1.3692) | Simple pneumonia and pleuritis age>17 with CC | 85 (10.4%) | 9.76 | 78 (10.8%) | 11 (ns) |
| 102 (0.6215) | Other diagnoses of the respiratory tract | 29 (3.5%) | 7.21 | 67 (9.3%) | 7.45 (ns) |
MDC 4: major diagnostic category 4 (respiratory tract); MHS: mean hospital stay, in days; DRG: diagnosis-related group; n: number of cases (%: per 1000 inhabitants; %: percentage of the total number of discharges); ns: not significant; *: P=.006.
The mean hospital stays of the MDC4 were 9.81 days in Barbanza and 10.39 in its reference hospital, CHUS (P<.0001). The greatest difference was in DRG 87 (pulmonary edema and respiratory insufficiency) with hospitalizations of 8.8 and 9.72 days, respectively (P=.01). In the Cee hospital and its reference center CHUAC, the means stays of MDC4 were 9.97 and 11.96 days, respectively (P<.00001), with a greater difference for DRG 541 (simple pneumonia and other respiratory disorders) of 11.45 days in Cee and 13.67 in CHUAC (P=.0005). The number of discharges with MDC4 at the reference hospitals that originated from the district hospitals was insufficient for statistical analysis.
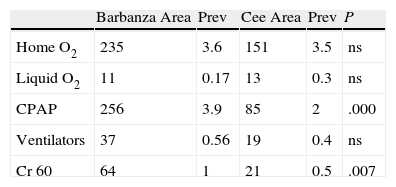
Table 3 demonstrates the distribution of the prescriptions of oxygen therapy and other respiratory devices in the district areas. The prevalence of CPAP was significantly greater in Barbanza than in Cee (3.9 vs 2/1.000, P<.0001). No differences were found in the prevalence of either oxygen therapy or ventilators, although there were differences found in the prescription of high-flow aerosol therapy. Mortality in 2007 due to respiratory disease in the two district areas did not show differences in the total mortality of the population or in those under the age of 65 (Table 4).
Distribution, by Health-Care Areas, of the different forms of oxygen support and ventilators.
| Barbanza Area | Prev | Cee Area | Prev | P | |
| Home O2 | 235 | 3.6 | 151 | 3.5 | ns |
| Liquid O2 | 11 | 0.17 | 13 | 0.3 | ns |
| CPAP | 256 | 3.9 | 85 | 2 | .000 |
| Ventilators | 37 | 0.56 | 19 | 0.4 | ns |
| Cr 60 | 64 | 1 | 21 | 0.5 | .007 |
CPAP: continuous positive airway pressure; Cr 60: high-flow aerosol therapy; inh: inhabitants; ns: not significant; Prev: prevalence/1000 inhabitants; Ventilators: bi-level and volumetric positive airway pressure.
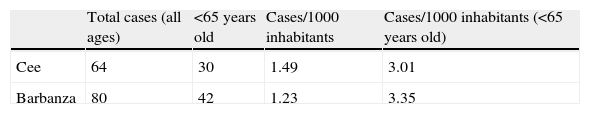
Mortality due to respiratory disease in the areas of Cee and Barbanza in 2007.
| Total cases (all ages) | <65 years old | Cases/1000 inhabitants | Cases/1000 inhabitants (<65 years old) | |
| Cee | 64 | 30 | 1.49 | 3.01 |
| Barbanza | 80 | 42 | 1.23 | 3.35 |
Source: Rexistro de Mortalidade de Galicia, Dirección Xeral de Saúde Pública e Planificación (Galician Death Registry).
The relationship between district and reference hospitals is similar to what is established between the Primary Care level and Specialized Care. The policy of derivations is variable6 for age, patient morbidity, cultural and geographic factors of the population, the overload of patients and the fluidity of the professional inter-relationship in the hospitals. The Spanish General Health-Care Law (Ley General de Sanidad 14/1986) states that health care services are to be provided to the entire population in conditions of effective equality, which implies eliminating the difficulties to access specialized medicine, especially in pathologies like respiratory ones that, in addition to having a high prevalence, carry with them severe and unstable situations.2 Despite this, there is no agreement about which model should be followed in managing the relationship amongst the district hospitals and the reference specialists. In fact, even under one same administration, as is the case of Galicia, there are different organizational methods coexisting. In this situation, we have compared two models dealing with pneumological pathologies in two district hospitals and their reference centers. They are situated in the same province, in coastal populations with similar socioeconomic characteristics and they both started almost simultaneously with an analogous organizational algorithm. Their technological equipment, proportion of hospital beds per inhabitant and per physician are also similar. As for the consultations for pneumopathies, the difference lies in the fact that Barbanza hospital has a pneumological consultation in situ where pulmonologists from the reference hospital see patients, while in Cee patients with said pathologies are seen by the internal medicine specialists of the center,who have the option of sending the patients for referral to the reference hospital for pulmonary interconsultation.
The participation of the consulting pulmonologists in Barbanza has an immediate implication in the mean time elapsed for consultation: 40 days. Although we do not have available these data for the respiratory patients of Cee, it is likely that this center follows the tendency of the general internal medicine consultation, meaning, longer than for the pulmonology patients of Barbanza. The time delay in seeing patients for a certain type of disease depends on its frequency and on the appointment availabilities in a center. Keeping in mind the high prevalence of pneumopathies, it is understandable to think that, even though it is shorter, the delay in Barbanza is not ideal. However, it must be considered that the outpatient consultations of the district hospitals treat heterogeneous processes and that not all patients require the same priority.7 In any case, if the situation so requires, the health-care system has channels giving preference to other health-care levels.
Spirometry is essential for the correct management of pulmonary diseases8 and is a standard of quality health care.9 It is indispensable for the early diagnosis and treatment according to severity level of COPD and bronchial asthma. These diseases consume many resources,10 especially in their moderate-severe stages, which in the case of COPD represents 4.4% of the population.11 On the other hand, although the number of spirometries done in the CHUAC in patients from that district was higher than the CHUS in patients from Barbanza, these latter patients underwent functional studies that included more clinical parameters. The number of patients referred to CHUAC was greater, but in a non-significant range. As for bronchoscopies, the data are insufficient to be able to reach conclusions, but the limited number of cases over the period of a year is an argument that does not support them being done in a district center. Thus, the follow-up of the respiratory pathologies in Barbanza, with a greater number of spirometries and other respiratory diseases, follows the recommended guidelines for the management of patients with very prevalent chronic processes,12 while giving referrals for complex pneumopathies that require the expertise of a specialist.
Home oxygen and ventilation treatments represent an important expenditure for the health-care system and are an indirect indicator of the load of the advanced disease. Oxygen therapy is prescribed following well-defined guidelines by both general medicine physicians and specialists, which can explain why the prevalence is similar in both areas. The same is true for home ventilation, prescribed by pulmonologists. We do not have enough information to explain the differences in aerosol therapy. Regarding CPAP therapy, it is indicated after having identified and diagnosed patients with sleep apnea-hypopnea syndrome (SAHS), which is a very prevalent process in male adults13 and in recent years was seen to be one of the most frequent reasons for consultation in a district hospital.7 In addition, it is usually associated with other chronic diseases, such as metabolic syndrome, arterial hypertension, ischemic cardiopathy and COPD, all of which increase health-care costs and add more morbidity and complexity to be studied.14 The greater prevalence of patients with CPAP in the area of Barbanza indicates that in this hospital there is a greater index of suspicion, detection and treatment of SAHS, a fact that carries health-care and cost-effectiveness implications.15
The case-mix of hospitalization is a criteria for evaluating the quality of the care and, with some limitations,16 is an indicator for comparing the activity between hospitals. The mean hospital stays for the respiratory patients grouped in MDC-4 did not show differences between the two districts. Nor were any significant differences found in the comorbidities or re-hospitalizations within the month after discharge. Although the mean hospital stay for COPD exacerbations (DRG 88) was greater in Cee, we believe that this data should be interpreted with reservations. As it is information generated by different codifiers in different centers, we cannot be sure that strictly homogenous criteria had been used. In fact, the discharges of patients with COPD can be classified in three different DRGs (541, 87, and 88). If not, it would be difficult to explain why in Barbanza DRG 87 represents 17.9% of admittances, while in Cee it is only 0.3%. In any event, it cannot be affirmed that the presence of a pulmonologist in the outpatient consultation influences hospitalization. The stays were longer in the university reference hospitals. This fact, already indicated in other studies17,18 can be explained by the redundancy and multiplicity of the health-care circuits in large hospitals that also receive more complex cases.
It should be contemplated whether this activity could be developed through telemedicine. This formula, more developed in specialties such as dermatology, does not require the specialist to go from place to place. In pulmonology, there is some experience with this in lung cancer, and it has been confirmed to influence in the reduction of delay before surgery.19 Although it has undoubtable value in certain aspects, given the varied nature of respiratory pathologies and their high frequency in consultations, it would seem more adequate for the specialist to have direct contact with the patients and physicians of the center itself.
Obviously, one must take into account the cost of consultations. The design of this present study does not enable us to calculate the costs vs benefits of hiring a part-time pulmonologist. According to our estimations, it would not seem to be very onerous as the cost of the special 10-day program, foreseeable for the population of these two district hospitals,20 would cost 25960 € per year, a much lower cost than having a specialist on staff and one which would be bearable for the budget of a district hospital. But it must be emphasized that in the model of a hospital without a pulmonologist, part of the treatment cost is then transferred to the patients and their companions who then need to travel to the reference hospital. On the other hand, in the option of a hospital with a pulmonologist, the shorter delays and more qualified care are unquantified elements that surely minimize costs.
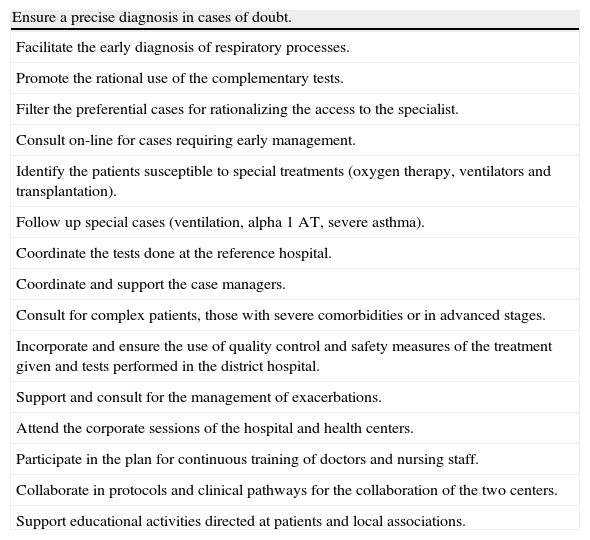
So, the greater number of lung function tests in order to ensure the management of prevalent diseases such as COPD and asthma, and the great number of patients diagnosed with SAHS, indicate that the health care provided in the outpatient consultations with consulting pulmonologists who are hired part time, is more complete that in hospitals that lack this type of resource. An aspect that is difficult to measure, but one which should not be overlooked as it is an added value for the model with consulting pulmonologist, is that of being able to regulate and prioritize the tests that are done in the reference hospital, such as bronchoscopies, pleural biopsies or other techniques. But in addition, the contribution of the pulmonologist should not be merely limited to attending patients in the consultation and coordinating tests. We believe that his/her involvement in other activities would have an undoubtable impact on hospitalizations21 and other aspects of care in the hospital and the area (Table 5).
Functions of a consulting pneumologist in a district hospital.
| Ensure a precise diagnosis in cases of doubt. |
| Facilitate the early diagnosis of respiratory processes. |
| Promote the rational use of the complementary tests. |
| Filter the preferential cases for rationalizing the access to the specialist. |
| Consult on-line for cases requiring early management. |
| Identify the patients susceptible to special treatments (oxygen therapy, ventilators and transplantation). |
| Follow up special cases (ventilation, alpha 1 AT, severe asthma). |
| Coordinate the tests done at the reference hospital. |
| Coordinate and support the case managers. |
| Consult for complex patients, those with severe comorbidities or in advanced stages. |
| Incorporate and ensure the use of quality control and safety measures of the treatment given and tests performed in the district hospital. |
| Support and consult for the management of exacerbations. |
| Attend the corporate sessions of the hospital and health centers. |
| Participate in the plan for continuous training of doctors and nursing staff. |
| Collaborate in protocols and clinical pathways for the collaboration of the two centers. |
| Support educational activities directed at patients and local associations. |
This study has some limitations. It lacks information on the costs of care, more detailed health-care data and it is retrospective (although this latter factor ensures that the evaluation has been done with no interference by the authors). Furthermore, other organizational options could be more adequate for different populations.22 With these exceptions, in centers with the characteristics that have been analyzed in the present article, the participation in outpatient consultations of pulmonologists who travel there from the reference hospital provides advantages in outpatient care, which is more complete, more specialized and, probably, of better quality in than in the district hospitals that do not have this type of consultation, without influencing hospitalization. In order to analyze this aspect, a new study would be needed to evaluate the cost-effectiveness of the pulmonologist working in hospitalization compared with the internal medicine specialist.
FundingThe authors declare having received no funding in the process of preparing this article.
Conflict of interestThe authors declare having no conflict of interests.
The authors would like to acknowledge José Ángel Novo Platas and Olga Sánchez Meizoso from the administrative departments of the University of Santiago Hospital Complex and the University of A Coruña Hospital Complex.
Please cite this article as: Verea-Hernando H, et al. Coordinación de la asistencia entre un hospital comarcal y su centro de referencia: evaluación de dos modelos de atención neumológica. Arch Bronconeumol. 2011;47:290–5.