To estimate the prevalence of tuberculous infection (TI) in the health-care workers of a hospital over the course of a 20-year period and analyze the associated risk factors.
Subjects and methodsA cross-sectional, descriptive study of the workers of a general hospital from 1988 until 2007, using a tuberculin test (TT) and questionnaire.
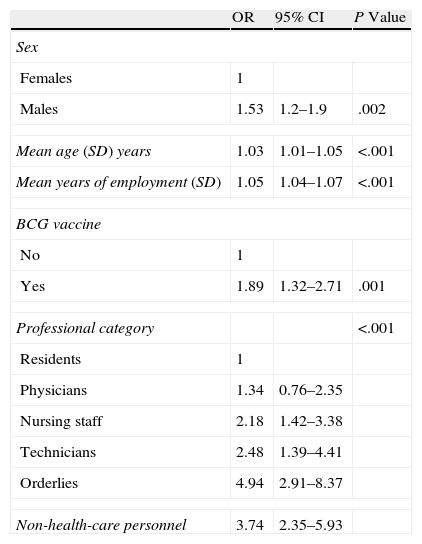
ResultsTwo thousand one hundred seventy-nine workers were studied (mean age 32.4 years (SD 8.4)). 24.5% worked in areas at risk for tuberculosis (TB). 8.1% (174) were vaccinated with BCG. The prevalence of positive baseline TT was 25.7% (95% confidence interval: 23.8%–27.4%). There was a greater percentage of positive TT in the 1988–1992 period (44.2%) and a smaller percentage (15.8%) in the 2003–2007 period (P<.0001). The prevalence of TI was 1.53 times greater in males and 1.89 in those vaccinated with BCG. When compared with resident physicians, the prevalence of TI was greater in the rest of the professional categories, while increasing 1.03 times per year that age increases and 1.05 times per year of professional activity.
ConclusionsThe data provide relevant information about the evolution of TI in hospital professionals over the course of a 20-year period. The prevalence decreased during the study period, probably due to a decrease in the incidence of TB in the reference community and to improved prevention measures and nosocomial control.
Estimar la prevalencia de infección tuberculosa (IT) en los trabajadores de un hospital a lo largo de un período de 20 años y analizar los factores de riesgo asociados.
Sujetos y métodosEstudio descriptivo transversal de los trabajadores de un hospital general desde el año 1988 hasta 2007, mediante prueba de tuberculina (PT) y cuestionario.
ResultadosSe han estudiado 2.179 trabajadores (edad media, 32,4 años (DE: 8,4)). El 24,5% trabajaban en áreas de riesgo de tuberculosis (TB). El 8,1% (174) estaban vacunados con BCG. La prevalencia de PT positiva basal fue del 25,7% (intervalo de confianza del 95%: 23,8–27,4%). Destaca el mayor porcentaje de PT positivas en el período 1988–1992 (44,2%) y un porcentaje menor (15,8%) en el período 2003–2007 (p<0,0001). La prevalencia de IT fue 1,53 veces superior en varones y 1,89 en vacunados con BCG. En comparación con los MIR, la prevalencia de IT fue superior en el resto de categorías profesionales y se incrementó 1,03 veces por cada año de incremento de edad y 1,05 veces por cada año de actividad profesional.
ConclusionesLos datos aportan información relevante sobre la evolución de la IT en los trabajadores del hospital a lo largo de un período de 20 años. La prevalencia disminuyó a lo largo del período estudiado probablemente debido a una disminución de la incidencia de TB en la comunidad de referencia y a una mejora de las medidas de prevención y control nosocomial.
Exposure to patients with active tuberculosis (TB) is considered an occupational risk for health-care professionals. The risk of TB transmission in health-care employees fundamentally depends on the type of care provided, the incidence of TB in the community and the implementation and compliance with TB prevention and control programs in health-care centers.1–3 These prevention programs should include periodical medical examinations of susceptible workers (with an initial risk evaluation and periodic follow-up), the use of adequate isolation measures and the diagnosis and early treatment of TB patients. There are studies that confirm that, in centers where control measures have been applied, the risk for contracting TB in health-care personnel is very similar to that of the community where they reside.4,5
In a recent review of studies on TB infection in health-care workers in countries with a low incidence of TB, the authors concluded that there is still a high risk for TB in the collectives that perform their occupational duties in certain risk areas.6 One of the causes for the increased risk of TB in health-care professionals in countries with a low incidence may be the delay in diagnosis.7,8 On the other hand, it may also be due to the higher number of immigrant health-care professionals coming from countries with a high prevalence of TB infection.
In Spain, there are few data available related with the magnitude of both infection as well as tuberculosis disease in health-care staff. The majority of the studies have been done in other countries where the epidemiological situation does not coincide with the Spanish situation.
The traditional screening test used in protocols of health-care personnel with occupational exposure to TB is the tuberculin test (TT).2 Recently, new tests are being introduced that are based on the detection of interferon gamma (IFN-γ) released as a response to the in vitro stimulation of the sensitized T cells in the peripheral blood with specific Mycobacterium tuberculosis antigens.9,10 In a previous study done in our center, we reached good agreement between the two IFN-γ tests (T-SPOT.TB and QFN-G-IT) for the diagnosis of TB infection in health-care personnel. In addition, both IFN-γ techniques were not affected by vaccination with BCG and they were more associated with occupational exposure than TT, possibly being more useful for detecting recent infection.11
The objective of this study was to estimate the prevalence of TB infection in the staff of a hospital over a 20-year period and to analyze the risk factors associated with this infection.
Patients and MethodsStudy DesignCross-sectional descriptive study from 1988 to 2007 (20 years), with a retrospective analysis of the information.
Study LocationThe study took place at the Hospital Germans Trias i Pujol (HGTiP), a general medical-surgical, third-level hospital with 600 beds and close to 3000 health-care professionals. It provides care for a population of 200000 inhabitants and it is the reference hospital for more than 700000 people. In 2009, it generated more than 27000 hospitalizations and 110000 emergency room visits. The number of patients admitted with TB varied throughout the period studied, ranging from 150 in the first few years to approximately 50 annually later years. The incidence of TB in the reference community has also varied in the study period, with an incidence of 45/100000 inhabitants in the year 1990 to an incidence of 20.6/100000 inhabitants in the year 2006.12,13 In our hospital, starting in the year 1994 and coinciding with the new CDC guidelines on the prevention and control of the nosocomial transmission of TB,14 a series of measures were reinforced. These measures included, among others, the improvement of the ventilation systems in certain rooms for the isolation of TB patients, the improvement in the patient-care circuits in the ER and the promoted use of proper respiratory protection.
Study PopulationHospital staff who volunteered for the health test in the Preventative Medicine Department (PMD) during the study period.
MethodologySince 1988, there is a TB watch program in the hospital for health-care staff. At the first health examination done in our department (either at the initial visit at the start of employment or at any moment during employment), workers with no previous history of TB or without previous positive TT undergo TT (administration of 2UT of PPD-RT23 tuberculin according to the Mantoux technique, with a reading 48–72h later). If the TT is negative and there is occupational risk for exposure, this test is done annually in workers from risk areas, or at a maximum of every 2 years. In the case that it is done for the first time and the result is negative, a second TT is repeated 7–10 days later in order to study the “booster effect”. All the workers of our study with positive TT had chest radiography in order to rule out TB and evaluate the indication of treatment for TB infection. In all cases, the subjects filled out a questionnaire including sociodemographic characteristics (age, sex), occupational risk factors, history of exposure to TB and history of vaccination with BCG (with vaccine document and/or search for the vaccination scar).
Study VariablesPositive TT: induration ≥5mm, and in those vaccinated with BCG ≥15mm (in accordance SEPAR guidelines3).
Depending on the risk for exposure to TB, we have differentiated: high-risk areas15 (emergency, pulmonology, internal medicine, HIV day hospital, microbiology, bronchoscopy and pathological anatomy) and low-risk areas (other services and/or units).
The professional categories were: physicians, resident physicians, nursing staff, lab technicians, orderlies, administrative staff and other non-health-care staff (maintenance, kitchen staff and administration).
Other variables analyzed were: years of occupational activity, vaccination with BCG, TT induration (mm), history of previous TT, presence of booster and chest radiography results.
Statistical AnalysisWe calculated the prevalence of positive baseline TT and the 95% confidence interval (95% CI). For the study of the variables related with the result of the positive baseline TT, the Chi-squared and the Student's t tests were used. We used a multivariate logistic regression model for the positive TT result variable, including in the model the independent variables with a level of significance in the univariate analysis equal or less than 0.20. Both the odds ratio (OR) and the 95% CI were calculated for each variable. The validation of the final model was done by means of the Hosmer–Lemeshow test (P>.05). For all the analyses, a bilateral significance level P<.05 was considered significant. The analysis was done using the SPPS version 14.0 statistical package.
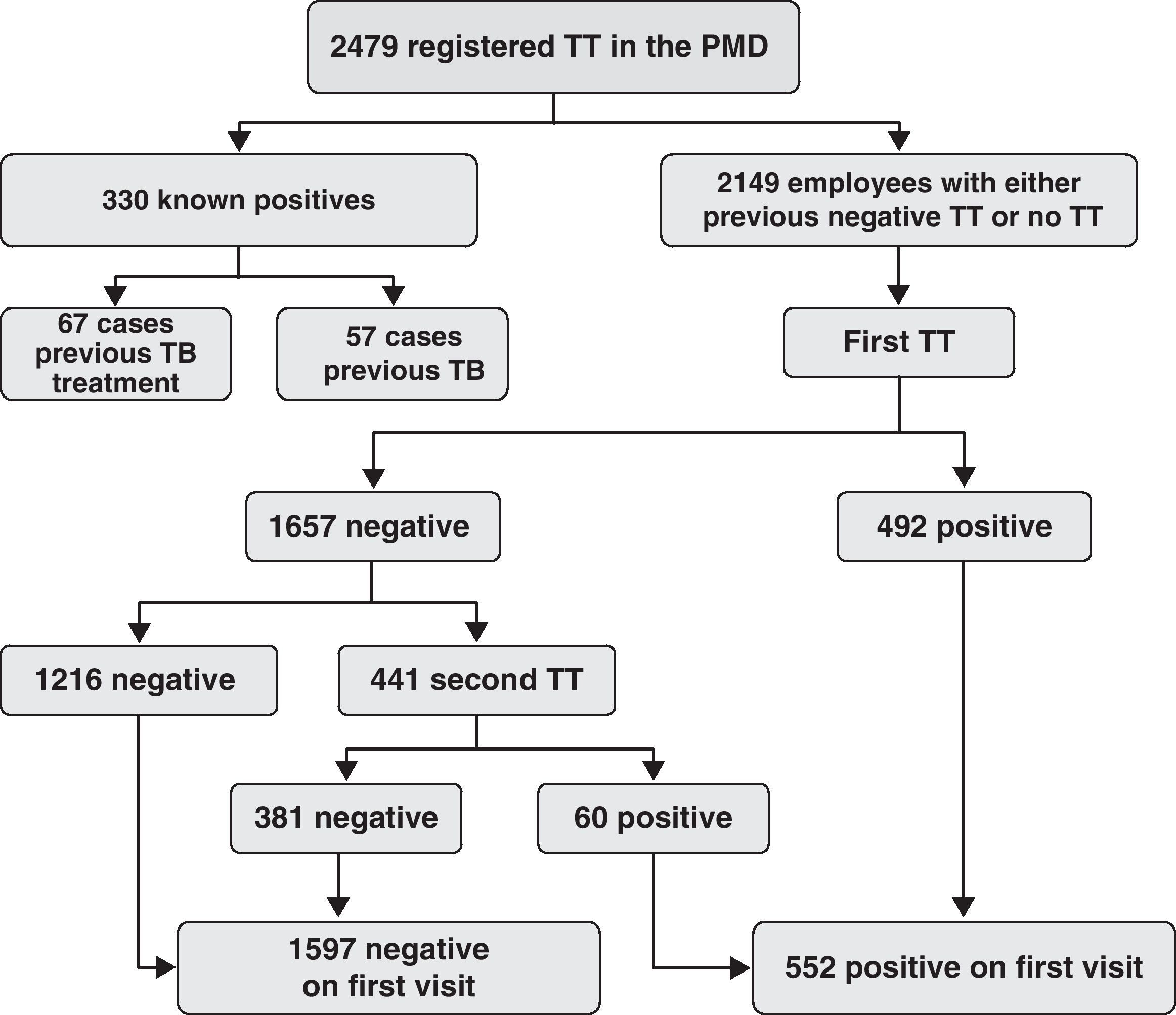
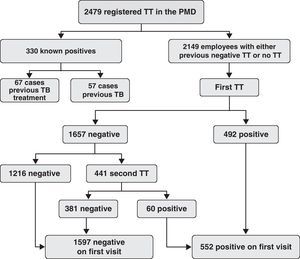
ResultsDescription of the Study PopulationIn the PMD, 2479 workers were registered: 330 (13.3%) had a history of previous positive TT (with 57 [2.3%] cases of previous TB and 67 [2.7%] cases of TB infection). The remaining 2149 (86.7%) workers had a tuberculin test (Fig. 1).
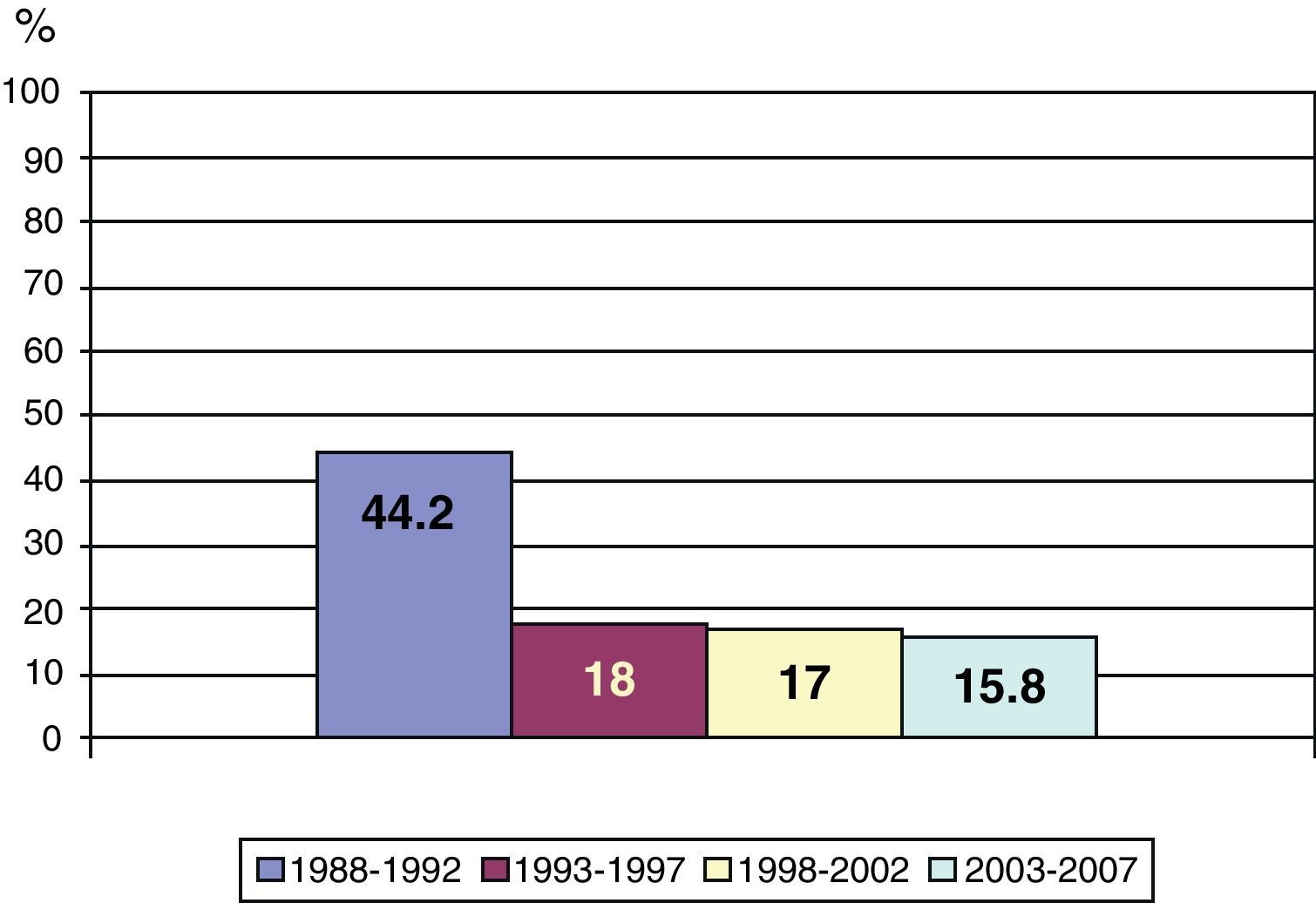
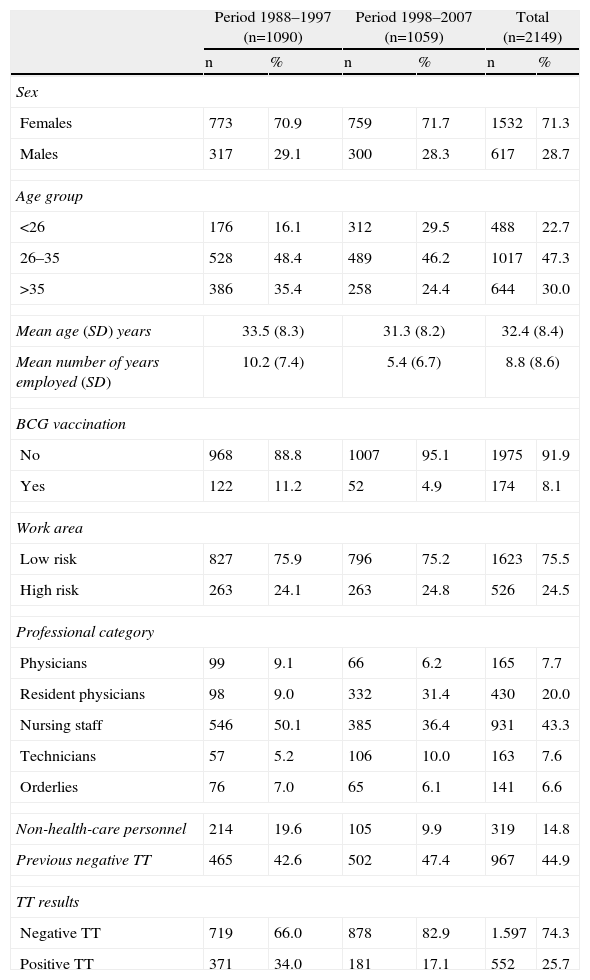
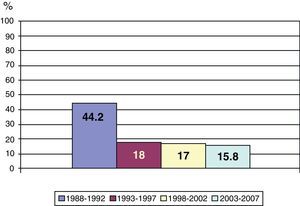
The characteristics of the population studied are presented in Table 1. Mean age was 32.4 (SD: 8.4), and there was a predominance of females (71.3%). The most frequent occupational category was nursing staff (43.3%) followed by residents (20.0%), while 14.8% were non-health-care personnel. 24.5% of the subjects carried out their activity in areas at risk for TB. Mean number of years of employment was 8.8 (SD: 8.6). 8.1% (174) had been vaccinated with BCG. The overall prevalence of positive baseline TT was 25.7% (95% CI: 23.8%–27.4%). No cases of TB were detected with this screening method; chest radiography was normal in 522 workers (94.5%), and in 30 (5.5%) we observed residual lesions suggestive of previous TB. We detected a “booster effect” in 60 workers (10.8% of the positive TT) with a mean age of 34.2 years (SD: 8.2) and with a history of BCG vaccination of 10%. The prevalence of positive baseline TT by year is shown in Fig. 2. There was a higher percentage of positive TT from 1988 to 1992 (44.2%) and a lower percentage (15.8%) in the 2003–2007 period (P<.0001). Among the staff from high-risk areas who underwent periodical TT, the rate of incidence was 3.8 per 100 persons-year (95% CI: 3.7–4.0), varying from 46.8 in the year 1990 to 1.08 in the year 2007.
Characteristics of the Employees With TT Done in the Preventive Medicine Department (n=2149), Total and According to Study Period.
| Period 1988–1997 (n=1090) | Period 1998–2007 (n=1059) | Total (n=2149) | ||||
| n | % | n | % | n | % | |
| Sex | ||||||
| Females | 773 | 70.9 | 759 | 71.7 | 1532 | 71.3 |
| Males | 317 | 29.1 | 300 | 28.3 | 617 | 28.7 |
| Age group | ||||||
| <26 | 176 | 16.1 | 312 | 29.5 | 488 | 22.7 |
| 26–35 | 528 | 48.4 | 489 | 46.2 | 1017 | 47.3 |
| >35 | 386 | 35.4 | 258 | 24.4 | 644 | 30.0 |
| Mean age (SD) years | 33.5 (8.3) | 31.3 (8.2) | 32.4 (8.4) | |||
| Mean number of years employed (SD) | 10.2 (7.4) | 5.4 (6.7) | 8.8 (8.6) | |||
| BCG vaccination | ||||||
| No | 968 | 88.8 | 1007 | 95.1 | 1975 | 91.9 |
| Yes | 122 | 11.2 | 52 | 4.9 | 174 | 8.1 |
| Work area | ||||||
| Low risk | 827 | 75.9 | 796 | 75.2 | 1623 | 75.5 |
| High risk | 263 | 24.1 | 263 | 24.8 | 526 | 24.5 |
| Professional category | ||||||
| Physicians | 99 | 9.1 | 66 | 6.2 | 165 | 7.7 |
| Resident physicians | 98 | 9.0 | 332 | 31.4 | 430 | 20.0 |
| Nursing staff | 546 | 50.1 | 385 | 36.4 | 931 | 43.3 |
| Technicians | 57 | 5.2 | 106 | 10.0 | 163 | 7.6 |
| Orderlies | 76 | 7.0 | 65 | 6.1 | 141 | 6.6 |
| Non-health-care personnel | 214 | 19.6 | 105 | 9.9 | 319 | 14.8 |
| Previous negative TT | 465 | 42.6 | 502 | 47.4 | 967 | 44.9 |
| TT results | ||||||
| Negative TT | 719 | 66.0 | 878 | 82.9 | 1.597 | 74.3 |
| Positive TT | 371 | 34.0 | 181 | 17.1 | 552 | 25.7 |
SD: standard deviation; TT: tuberculin test.
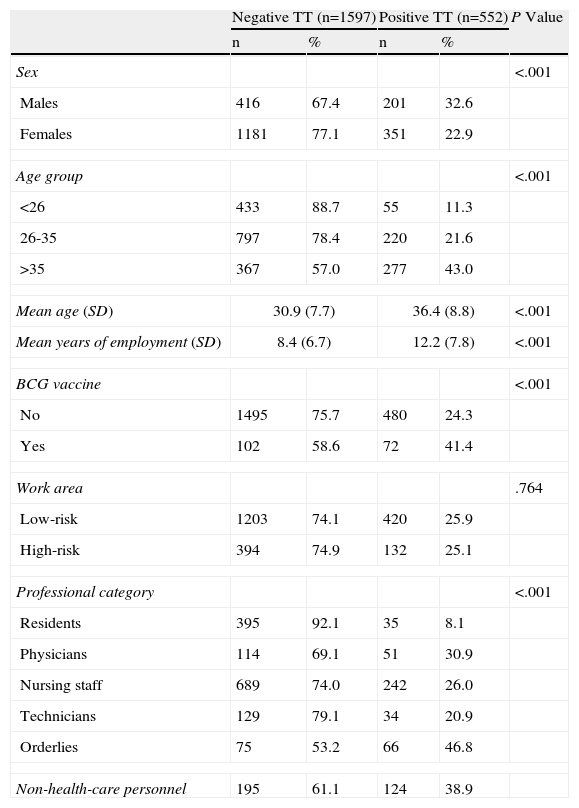
The variables significantly related with a positive baseline TT were sex, age, vaccination with BCG, professional category and years of employment (Table 2). The prevalence of positive TT was higher in males (32.6%), in those vaccinated with BCG (41.4%), in orderlies and in non-health-care personnel. By age groups, the prevalence in the <26 age group was 11.3%, in the 26–35-year-old group 21.6%, and in the >35-year-old group 43% (P<.001). No statistically significant differences were detected according to the risk of the work area.
Risk Factors Associated With Positive TT Done on the First Visit of 2149 Hospital Employees; Univariate Analysis.
| Negative TT (n=1597) | Positive TT (n=552) | P Value | |||
| n | % | n | % | ||
| Sex | <.001 | ||||
| Males | 416 | 67.4 | 201 | 32.6 | |
| Females | 1181 | 77.1 | 351 | 22.9 | |
| Age group | <.001 | ||||
| <26 | 433 | 88.7 | 55 | 11.3 | |
| 26-35 | 797 | 78.4 | 220 | 21.6 | |
| >35 | 367 | 57.0 | 277 | 43.0 | |
| Mean age (SD) | 30.9 (7.7) | 36.4 (8.8) | <.001 | ||
| Mean years of employment (SD) | 8.4 (6.7) | 12.2 (7.8) | <.001 | ||
| BCG vaccine | <.001 | ||||
| No | 1495 | 75.7 | 480 | 24.3 | |
| Yes | 102 | 58.6 | 72 | 41.4 | |
| Work area | .764 | ||||
| Low-risk | 1203 | 74.1 | 420 | 25.9 | |
| High-risk | 394 | 74.9 | 132 | 25.1 | |
| Professional category | <.001 | ||||
| Residents | 395 | 92.1 | 35 | 8.1 | |
| Physicians | 114 | 69.1 | 51 | 30.9 | |
| Nursing staff | 689 | 74.0 | 242 | 26.0 | |
| Technicians | 129 | 79.1 | 34 | 20.9 | |
| Orderlies | 75 | 53.2 | 66 | 46.8 | |
| Non-health-care personnel | 195 | 61.1 | 124 | 38.9 | |
SD: standard deviation; TT: tuberculin test.
In the multivariate analysis, all the risk factors analyzed were statistically significant. The prevalence of TB infection was 1.53 times higher in males (95% CI: 1.2–1.9) and 1.89 in those vaccinated with BCG (95% CI: 1.32–2.71). According to the professional category and in comparison with the resident physicians, the prevalence of TB infection was 2.18 times higher in the nursing staff (95% CI: 1.42–3.38), 2.48 in the technicians (95% CI: 1.39–4.41), 4.94 in the orderlies (95% CI: 2.91–8.37) and 3.74 in non-health-care staff (95% CI: 2.35–5.93). The prevalence increased 1.03 times per each year of higher age (95% CI: 1.01–1.05) and 1.05 times per year of employment (95% CI: 1.04–1.07) (Table 3).
Risk Factors Associated With Positive TT Done on the First Visit in 2149 Hospital Employees; Multivariate Analysis.
| OR | 95% CI | P Value | |
| Sex | |||
| Females | 1 | ||
| Males | 1.53 | 1.2–1.9 | .002 |
| Mean age (SD) years | 1.03 | 1.01–1.05 | <.001 |
| Mean years of employment (SD) | 1.05 | 1.04–1.07 | <.001 |
| BCG vaccine | |||
| No | 1 | ||
| Yes | 1.89 | 1.32–2.71 | .001 |
| Professional category | <.001 | ||
| Residents | 1 | ||
| Physicians | 1.34 | 0.76–2.35 | |
| Nursing staff | 2.18 | 1.42–3.38 | |
| Technicians | 2.48 | 1.39–4.41 | |
| Orderlies | 4.94 | 2.91–8.37 | |
| Non-health-care personnel | 3.74 | 2.35–5.93 | |
SD: standard deviation; TT: tuberculin test.
The baseline prevalence of TB infection throughout the study period was 25.7%, and it was higher in the first years (44.2%) than in the last years (15.8%). In comparison, the mean prevalence in health-care workers in high-income countries is 24% (range 4%–46%). In low-income countries, the mean prevalence is 63% (range 33%–79%).16
The levels found in the present study are very similar to those of the prevalence in the general population in Catalonia in the same periods.17 As the authors of this mentioned study comment, a series of factors should be kept in mind when comparing TB infection data published for the general population. Among others, the main factors are: the TT technique has varied throughout the years; many studies have been done with samples that are not representative of the general population or with very imprecise samples; and, not all studies have contemplated the BCG vaccination. The risk factors associated with positive TT have been sex (male), age, years of employment, vaccination with BCG and professional category. These factors have been found in other studies in which age18–20 and years of employment19–21 reflect a greater possibility of having been in contact with tuberculous patients. The baseline prevalence was higher in non-health-care personnel and orderlies (38.9% and 46.8%, respectively). This may be due to the fact that the mean age of these collectives was higher than that of the health-care staff (mean age among non-health-care personnel was 34 vs 32 among the health-care staff, with a P<.001), although when adjusted for age the prevalence has continued to be higher in these collectives. One explanation could be, on the one hand, that they may have less epidemiological knowledge about the disease and, on the other, that they may have other non-occupational risk factors (place of residence, socioeconomic level) that have not been dealt with in this paper. In a study done in the city of New York,18 a higher baseline prevalence was also found in non-health-care personnel (maintenance, cleaning and security personnel). The authors argued that these workers had brief contact with the patients, but on a daily basis, and that they gave little importance to the use of protection measures, such as masks. In addition, as these professionals historically have not been considered groups at risk for TB, they are not included in training programs about preventive measures.
The percentage of “booster effect” found in our hospital (10.8%) is higher than that reported in other studies,22,23 with percentages of 5.2% and 2.8%, respectively, despite the fact that the epidemiological situation and vaccination with BCG is different in our setting.
The baseline prevalence was higher in the early periods than in the last years of the study. This could be due to various factors: in the initial years, both TB incident cases as well as prevalent cases were detected. Furthermore, there was a reduction in the incidence of patients with TB admitted to the hospital (from 150 annually at the beginning of the study to approximately 50 in recent periods). It may also be related with an improved compliance of the nosocomial TB control measures that have been implemented in the hospital over the course of the study period.24–26
It has been reported that when there are fewer patients admitted with TB, there is a delay in diagnosis.27 Along this line, in recent years ten contact studies have been done in our hospital in health-care workers who had experienced accidental occupational exposure to bacilliferous patients without measures of protection. Out of the 133 professionals studied, 5 cases of tuberculin conversion were detected and no cases of TB related to the exposure were found (unpublished data). Practically all these accidental exposures have been due to delay in the diagnosis of TB in patients. From the information available, we have seen that the maximum time without diagnosis was 2 weeks, with a mean of 8.4 days.
The higher prevalence data in the early periods could also be partially explained by the vaccination with BCG (the percentage of BCG vaccine recipients was higher in the early years). In Catalonia, between 1965 and 1980, millions of people were vaccinated. Although the vaccination history is registered systematically and the presence of the corresponding scar is verified, some individuals may have been included with positive TT due to the vaccine, and consequently the TB infection may have been overestimated.
One must also keep in mind the influence of immigration in recent years on the prevalence of infection and on the incidence of TB in the general population and that it may also have had an influence on health-care staff. This has happened in the United States,28 where it was found that the factors that are independently associated with the conversion of TT in health-care personnel were having been born outside of the United States and having a TT in an occupational contact study. In our setting and in our hospital, the number of immigrant staff members is still low but has been growing in recent years.
Lastly, it must also be taken into account that the community risk was not analyzed, and therefore we cannot rule out TB infection community transmission. The data were not adjusted for either area of residence of the workers or for socioeconomic level. According to Sepkowitz,29 in hospitals where few annual TB cases are admitted is where the community transmission could be more important than occupational transmission in hospital workers.
In summary, the data provide information about the evolution of TB infection among the employees at a third-level hospital over the course of a 20-year period. The prevalence of TB among the hospital staff is high, although it did decline over the period studied, which also coincided with a lower TB incidence in the reference community and fewer patients admitted with TB. In spite of this, due to the fact that when the number of patients admitted drops, the delay in diagnosis increases, it is important to continue with TB vigilance and control programs for hospital employees in order to determine the tuberculin state. At the same time, these programs should include training for health-care personnel, especially centered on the identification of the signs and symptoms of TB, its transmission mechanisms and the nosocomial prevention measures for the disease.
Conflict of InterestsThe authors declare having no conflict of interests.
Please cite this article as: Casas I, et al. Estudio de la infección tuberculosa en trabajadores de un hospital general universitario. Factores asociados y evolución en 20 años. Arch Bronconeumol. 2011;47:541–6.