Type 1 neurofibromatosis (NF1) is the most common form of neurofibromatosis, a group of genetic disorders of the nervous system that mainly affect the development and growth of neural cell tissues. NF1 occurs in approximately 1 of every 3000 newborns. Transmission to progeny is by the autosomal dominant mode, although up to 50% of new cases occur spontaneously through de novo mutations. The literature describing the association of NF1 with cardiovascular or airway malformations is sparse.1
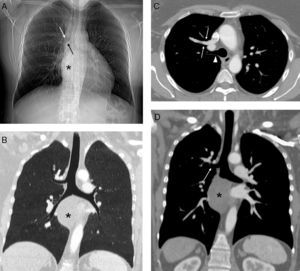
We report a clinical case of a 45-year-old woman with a diagnosis of NF1, non-smoker, with dysphagia due to a posterior mediastinal tumor causing compression of the thoracic esophagus. On magnetic resonance imaging, the tumor was radiologically consistent with right vagal nerve neurogenic tumor. The physical examination only revealed café-au-lait spots on the skin and several scars on her back and abdominal wall from previously resected neurofibromas at these sites. In view of symptoms of progressive dysphagia, we decided to perform surgical resection of the posterior mediastinal tumor. The pre-operative chest X-ray revealed suspected tracheal bronchus (TB) (Fig. 1A), so these examinations were complemented with a chest computed tomography (CT). This confirmed TB, and revealed the unexpected combination of partial anomalous pulmonary venous return (PAPVR), consisting of drainage from the right upper lobe vein into the superior vena cava (Fig. 1B–D).
(A) Chest X-ray showing a mediastinal mass (asterisk) obliterating the pleural-azygos-esophageal line and possible tracheal bronchus (arrows). (B) Minimum intensity projection coronal reconstruction confirming tracheal bronchus. Note the mediastinal mass (asterisk). (C) Axial chest computed tomography (CT) image with intravenous contrast medium, showing anomalous drainage from the right upper lobe pulmonary vein into the superior vena cava (arrows) and the tracheal bronchus (arrowhead). (D) Oblique CT coronal image with intravenous contrast medium showing tracheal bronchus (arrow) and the mediastinal mass (asterisk).
The combination of NF1 with pulmonary development anomalies, either vascular or airway, and their diagnosis in adults is exceptional, and, to our knowledge, this the first report of simultaneous NF1, PAPVR and TB.1 TB is one of the most common abnormalities of the bronchial tree and, despite its name, more often occurs in the right main bronchus than in the trachea itself. TB is generally diagnosed incidentally in asymptomatic patients undergoing bronchoscopy or chest CT for other reasons. It can, however, occasionally cause hemoptysis, recurrent lung infections, or right upper lobe atelectasis in intubated patients in whom the distal end of the endotracheal tube is located at or distal to the origin of the TB.2 PAPVR is a vascular development anomaly consisting of abnormal drainage of one or more pulmonary veins into a systemic vein (the innominate vein, superior vena cava, azygos vein, right atrium, coronary sinus, or inferior vena cava), causing left-to-right shunt. Adults with PAPVR have a risk of developing long-term pre-capillary pulmonary hypertension due to volume overload in the right ventricle.3 The combination of these 2 development anomalies in a single patient is exceptional.4 The association of NF1 with pulmonary development anomalies is very rare (2.3%).1 In a review of vascular and cardiac malformations in 2322 patients with NF1, pulmonary stenosis and aortic coarctation were more prevalent, but no cases of anomalous pulmonary vein drainage (partial or total) were identified.1 Detection of these 2 anatomical variants may have clinical, anesthetic and therapeutic implications in patients scheduled for thoracic surgery. In our case, the anesthetist and the thoracic surgeon were aware of the anomalies, and complete thorascopic resection of the right mediastinal tumor with preservation of the ipsilateral vagal nerve could be planned and successfully performed. Histological examination confirmed a myxoid neurofibroma without atypia. The post-operative period was incident-free, and the patient was discharged 4 days after the intervention.
This is the first description in the scientific literature of TB and PAPVR in an NF1 patient with symptomatic mediastinal neurofibroma, and is therefore an exceptional case.
Please cite this article as: Gorospe Sarasúa L, Saldaña Garrido D, Ayala Carbonero AM. Asociación de bronquio traqueal y drenaje venoso pulmonar anómalo parcial en paciente con neurofibromatosis tipo 1 y neurofibroma del nervio vago ipsilateral. Arch Bronconeumol. 2015;51:305-306.