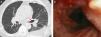
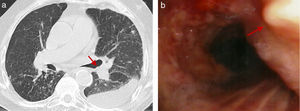
Tracheobronchopathia osteochondroplastica (OT) is a rare benign disorder characterized by the presence of multiple osseous or cartilaginous nodules in the submucosa of the trachea and main bronchi.1 We report the case of a 70 year-old male admitted to our hospital for a left pleural effusion interpreted as metapneumonic and treated with antibiotics. The chest-CT revealed a left pleural effusion, centrilobular lung nodules, and calcified nodular irregularities in the lower portion of the anterior wall of the trachea (Fig. 1a). Blood cultures were positive for Mycobacterium tuberculosis (MT). He was submitted to a bronchofibroscopy, where white ‘rock’ lesions were observed in the trachea and biopsied (Fig. 1b). The histology confirmed the diagnosis of OT. MT was isolated from bronchial secretions and the diagnosis of Pulmonary Tuberculosis was also established. The patient completed 6-months of tuberculostatic treatment and is now asymptomatic. As described in the literature and observed in this case, the diagnosis of OT is usually incidental and the clinical course is benign, with only a few cases requiring local treatment for stenosis or uncontrolled symptoms. It is also worth noting the increased risk of infections2 and the importance of considering this diagnosis when radiological and endoscopic changes described are observed.
Please cite this article as: Sousa M, Silva J, Rodrigues B. Tuberculosis y traqueobroncopatía osteocondroplásica coincidentes en un paciente. Arch Bronconeumol. 2017;53:343.