Sarcoidosis is a pleomorphic disease that can present with pulmonary hypertension (PH). What little information is available about the association of these two diseases comes mainly from small series of patients scheduled for transplant. We present four cases of mild pulmonary involvement in whom right catheterisation was performed and PH-specific therapy was administered. After obtaining written consent, a genetic study was performed that showed mutations in PH-related genes in three of the patients. This is the first study of its kind to yield genetic information for this type of PH.
La sarcoidosis es una enfermedad pleomórfica que en ocasiones puede presentar hipertensión pulmonar (HP). Existe poca información sobre la asociación de estas 2 enfermedades, en muchos casos de pequeñas series de pacientes enviados para trasplante. Presentamos 4 casos con afectación pulmonar leve en los que se realizó cateterismo derecho y se utilizó tratamiento específico para HP. Tras consentimiento informado, se hizo un estudio genético que mostró mutaciones en genes relacionados con HP en 3 pacientes. Se trata del primer estudio que proporciona información genética en este tipo de HP.
Pulmonary hypertension (PH) can present as an isolated disease, in most cases without a defined cause, or can be associated with other diseases or exogenous agents, both toxins and drugs. Group 5 of the latest Nice clinical classification of the disease groups PH cases with unclear mechanisms, and encompasses very different diseases or conditions with very different pathogeneses, prognoses and treatment1; sarcoidosis-associated PH, a very pleomorphic disease, is one of these. There is little information on the incidence, underlying changes, clinical presentation and therapeutic response of this type of PH, and in many cases what little there is has come from patients referred to lung transplant referral hospitals, or diagnosed solely by echocardiography.2,3 Like other chronic lung diseases that can progress to respiratory failure, PH (generally mild or moderate) is common in the advanced fibrotic stages of sarcoidosis, and it generally has little impact on prognosis.4 In contrast, the PH observed in patients with lesser pulmonary involvement seems to be associated with significantly lower survival rates, and could perhaps benefit from specific treatment. This PH does not correlate with the severity of the underlying lung disease, and can appear even in the absence of radiological lung changes. Various mechanisms have been proposed to explain its development, such as destruction of the vascular bed and compression of the pulmonary vessels by lymphadenopathies or vasospasm.5 We report on a series of 4 patients diagnosed with sarcoidosis-associated PH using right heart catheterization, in whom pulmonary vasodilator drugs were administered.
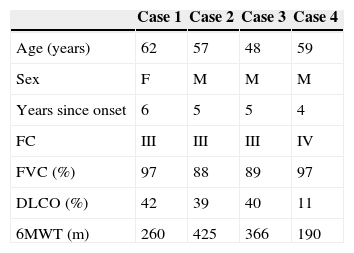
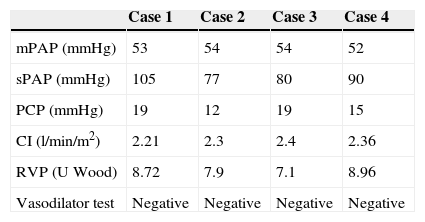
Clinical FindingsFour patients (3 men and 1 woman) were seen in our PH Unit for sarcoidosis diagnosed by transbronchial biopsy and suspected PH between January 2004 and January 2013. Only 1 of the patients (case 4) had extrapulmonary involvement, which consisted of various nodular cutaneous lesions on both forearms; on biopsy, these were found to be histologically consistent with sarcoid granulomas. The clinical characteristics of the patients are shown in Table 1. The diagnosis of sarcoidosis had preceded the onset of PH by a median of 5 years (4–6). The initial symptom was rapidly progressive dyspnea on exertion (time to diagnosis, 5–8 months). Three patients were classified in functional class (FC) III and one in FC IV. Bronchoalveolar lavage performed in 2 patients (2 and 3) showed lymphocytosis with predominantly CD4+ lymphocytes. Lung volumes were normal or near normal in all cases. Single-breath diffusing capacity (DLCO) ranged from 11% to 42% of theoretical values, with a significant decrease with respect to values prior to the onset of the PH (median 28% of the theoretical value). Chest computed tomography (CT) showed lymphadenopathies of less than 3cm in all cases. Three patients had mild or moderate interstitial involvement consisting of peribronchovascular micronodules in cases 2 and 3, and fibrosis predominantly in the middle lung zones in case 4. No pulmonary artery thrombi were detected in any of the patients. All were receiving oral steroid treatment (10–20mg/day of prednisone or equivalent). The systolic pulmonary artery pressure estimated by echocardiography ranged from 68 to 105mmHg, with no significant left heart abnormalities in any of the patients. The distance walked in the 6min walk test (6MWT) varied widely. The hemodynamic parameters obtained from diagnostic catheterization can be seen in Table 2. In all cases, the patient had severe PH, with mean pulmonary artery pressure (mPAP) greater than 50mmHg. Two patients had pre-capillary PH, while the other two were probably mixed disease (pre- and post-capillary).
Patient Characteristics.
| Case 1 | Case 2 | Case 3 | Case 4 | |
|---|---|---|---|---|
| Age (years) | 62 | 57 | 48 | 59 |
| Sex | F | M | M | M |
| Years since onset | 6 | 5 | 5 | 4 |
| FC | III | III | III | IV |
| FVC (%) | 97 | 88 | 89 | 97 |
| DLCO (%) | 42 | 39 | 40 | 11 |
| 6MWT (m) | 260 | 425 | 366 | 190 |
Age: at the time of PH diagnosis.
Years since onset: from diagnosis of sarcoidosis to diagnosis of PH.
FC: functional class; DLCO: CO diffusion as percentage of predicted value; FVC: forced vital capacity as percentage of predicted value; F: female; 6MWT: distance walked in 6min at the time of diagnosis; M: male.
Diagnostic Catheterization Results.
| Case 1 | Case 2 | Case 3 | Case 4 | |
|---|---|---|---|---|
| mPAP (mmHg) | 53 | 54 | 54 | 52 |
| sPAP (mmHg) | 105 | 77 | 80 | 90 |
| PCP (mmHg) | 19 | 12 | 19 | 15 |
| CI (l/min/m2) | 2.21 | 2.3 | 2.4 | 2.36 |
| RVP (U Wood) | 8.72 | 7.9 | 7.1 | 8.96 |
| Vasodilator test | Negative | Negative | Negative | Negative |
CI: cardiac index; mPAP: mean pulmonary artery pressure; sPAP: systolic pulmonary artery pressure; PCP: pulmonary capillary pressure; PVR: pulmonary vascular resistance.
Treatment with bosentan 125mg/12h was started in three cases (cases 1–3), and with tadalafil 40mg/24h in the other. A favorable response was initially observed (improvement of 1 FC and a mean of 80m in the 6MWT) in 3 patients (cases 1, 3 and 4), although a new drug had to be added due to deterioration in cases 1 and 4 at months 5 and 7, respectively (case 1, sildenafil 40mg/8h, and case 4, ambrisentan 5mg/24h); an improvement was observed only in case 4. There was very little response in case 2, so sildenafil and later subcutaneous treprostinil were added. However, the patient continued to deteriorate, and was included on the lung transplant list (36 months after diagnosis). Two patients died: case 1 died 29 months after diagnosis due to vascular disease progression, and case 4 after 9 months (sudden death). Case 3 remains in FC II on monotherapy after 57 months of follow-up.
After obtaining informed consent, a genetic study was carried out on the 4 patients. In case 1, a pathogenic mutation in gene BMPR2 (Bone Morphogenetic Protein Receptor 2), c.1467G>A (p.E489E) was found. Case 2 also had a potentially pathogenic mutation, c.622G>T (p.E208*) in gene KCNA5 (potassium voltage-gated channel, shaker-related subfamily, member 5), one of the voltage-dependent calcium channels that has been implicated in the pathogenesis of PH.6 Case 4 was a carrier of another pathogenic mutation in BMPR2, c. 484G>C (p. A162P).
DiscussionWe present 4 patients with sarcoidosis-associated PH, including clinical data, therapeutic response and genetic study. This is the first study of this kind published in Spain. The prevalence of PH in this disease is not well known, and values ranging from 5% to 74% have been reported, the latter always in patients with very severe disease who have been referred for lung transplant assessment.7 A prospective single-center study with 111 patients diagnosed with sarcoidosis by means of a protocol that included right heart catheterization following a suspicious echocardiography found only 5 cases of PH, one of them post-capillary.8 Although the pathogenesis is not well understood, sarcoid granulomas on the pulmonary vessel walls are known to occur in over 60% of cases,9 and some cases simulating pulmonary veno-occlusive disease have been reported in the literature.10 Due to cardiac and/or venous involvement, PH can have both a pre-capillary (30% of cases) and post-capillary component, as was the case in 2 of our patients. PH is diagnosed equally in both sexes, most often in the sixth decade of life. The initial symptom is usually dyspnea, with a mean survival of slightly less than 6 years.11 Given the paucity of published studies, it is unclear which variables could be associated with the development of PH. It is quite clear, however, that it can present with any degree of lung involvement. There are no studies on the correlation with extrapulmonary forms, either. Our 4 patients had little lung disease and near normal lung volumes at the time of PH diagnosis. A high grade of pulmonary fibrosis has been found to carry a poorer prognosis, although it is difficult to separate the impact of the PH from the fibrosis itself. None of our patients had any major fibrotic lesions, and death or transplant was undoubtedly affected by PH.
The possible involvement of steroid treatment in the evolution of sarcoidosis-associated PH is unclear, and data are contradictory. The few studies investigating various PH-specific drugs usually report hemodynamic improvement, especially in pulmonary vascular resistance and cardiac output, reduction in natriuretic peptides, increase of around 45–55m in the distance walked in the 6MWT, with wide variability and differing results in FC classification. No comparative survival data are available. The outcome was satisfactory and long-term in only 1 of our 4 patients, with a modest response in another 2 cases and no response in the last. A 16-week, multicenter placebo-controlled randomized trial with bosentan was recently published, in which a significant improvement in hemodynamic parameters but no changes in the 6MWT were observed.12
One relevant finding in our series was the discovery of various potentially pathogenic mutations in 3 patients, particularly 2 cases with defects in BMPR2, the main gene associated with the onset of PH; one of the mutations changed the amino acid sequence of the protein and the other affected mRNA processing, producing a defective protein. The mutation detected in the KCNA5 gene causes a stop codon that foreshortens the protein, which may interfere in its physiological role. As far as we know, no other genetic studies have been conducted in patients with sarcoidosis and PH. The presence of these mutations supports the multifactorial etiology of PH and sheds more light on the importance of genetics in the development of the disease.
In conclusion, we present a small series of patients with PH and sarcoidosis treated with PH-specific drugs, with variable response. A genetic study showed some mutations in genes associated with this disease.
FundingThis study has been partly funded by Actelion.
Conflict of InterestsAdolfo Baloira has participated in remunerated meetings organized by Actelion, GSK, Pfizer and Lilly. The other authors declare that they have no conflict of interests.
Please cite this article as: Baloira Villar A, Pousada Fernández G, Núñez Fernández M, Valverde Pérez D. Estudio clínico y molecular de 4 casos de hipertensión pulmonar asociada a sarcoidosis. Arch Bronconeumol. 2015;51:e19–e21.