Pleural disease involves a large number of admissions and long hospital stays. In order to improve this situation, a Pleural Unit (PU) was created in our hospital. Our aim was to analyze the clinical impact of this unit.
Materials and methodsIn this prospective study, we included patients admitted to the PU of the Hospital Universitario Central de Asturias for primary spontaneous pneumothorax (PSP), secondary spontaneous pneumothorax (SSP), complicated parapneumonic pleural effusion (CPPE), and malignant pleural effusion (MPE) between January 2015 and December 2018. We analyzed descriptive parameters, mean length of stay, readmissions at 1 month, need for surgery, and in the CPPE group, in-hospital mortality. The data were compared with those of patients admitted to the respiratory medicine department for the same diseases during the previous two years (2013–2014). We also describe all procedures performed in the PU, in both inpatients and outpatients.
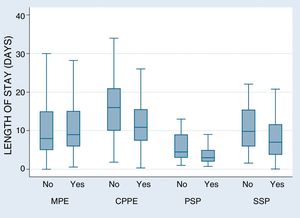
ResultsA total of 741 patients were included, We observed a progressive decrease in total admissions for pleural diseases and mean length of stay (days) (with the exception of MPE), as follows: PSP: from 6.2 to 4.2 (p = 0.004); SSP: 13.2 to 8.6 (p = 0.005), MPE: 10.3 to 12.3 (p = 0.05); and CPPE: 18.3 to 11.3 (p = 0.001) There was a reduction in hospital readmissions at 1 month and in in-hospital mortality due to CPPE in the PU period (14.9% to 5.5%) (p = 0.021).
ConclusionsThe creation of a PU could decrease the number of unnecessary admissions, and reduce mean lengths of stay and, in the case of CPPE, in-hospital mortality.
La patología pleural conlleva un gran número de ingresos y elevadas estancias hospitalarias. Con el fin de mejorar esto, se creó en nuestro hospital una Unidad de Patología Pleural (UPP). Nuestro objetivo es analizar el impacto clínico de dicha unidad.
Material y métodosEstudio prospectivo en el que incluimos a los pacientes ingresados en la UPP del Hospital Universitario Central de Asturias por neumotórax espontáneo primario (NEP), secundario (NES), derrame pleural paraneumónico complicado (DPPC) y derrame pleural maligno (DPM), entre enero de 2015 y diciembre de 2018. Analizamos parámetros descriptivos, estancias medias, reingresos al mes, necesidad de cirugía y, en los DPPC, también la mortalidad hospitalaria. Los datos se compararon con los de los pacientes ingresados por la misma patología en Neumología durante los dos años previos (2013–2014). Describimos además todos los procedimientos realizados en la UPP, tanto ambulatorios como en pacientes ingresados.
ResultadosSe incluyeron 741 pacientes. Objetivamos una disminución progresiva de los ingresos totales por patología pleural y de la estancia media días en dichas patologías, excepto en el DPM: NEP de 6,2 a 4,2 p = 0,004, NES de 13,2 a 8,6 p = 0,005, DPM de 10,3 a 12,3 p = 0,05 y DPPC de 18,3 a 11,3 p = 0,001. Existió una reducción de los reingresos al mes y de la mortalidad hospitalaria por DPPC en el periodo de la UPP 14,9% al 5,5% p = 0,021.
ConclusionesLa creación de una UPP podría disminuir el número de ingresos innecesarios, favoreciendo una reducción de las estancias medias y, en los DPPC, también la mortalidad hospitalaria.
Pleural involvement occurs in a group of conditions that nowadays are highly prevalent. Pleural effusion alone is estimated to affect more than 3000 people per 1000,000 inhabitants1 and comprises 4%–10% of respiratory diseases seen in pulmonology departments. We must also take into account complications, such as pneumothorax and iatrogenic pleural empyema, and other pathological processes that can develop in association with underlying diseases in patients admitted to other departments (thoracic surgery, general surgery, urology, etc.). Pleural disease is so widespread that it is often managed using disparate and heterogeneous criteria, to the extent that some publications2,3 have highlighted the need to create specific pleural units.
There is now broad experience in respiratory medicine in the creation of units dedicated to specific diseases, such as COPD,4 asthma,5 and lung cancer. The implementation of such units has led to a reduction in inappropriate hospital admissions,6 while dedicated lung cancer units have also reduced costs by 62%. Although experience in the field of pleural disease is limited, studies have demonstrated that procedures usually requiring hospital admission can be performed in an outpatient setting.7 Reports in the literature affirm that pleural outpatient units can reduce costs by up to 7.2-fold compared to hospitalization, and also reduce the time required for carrying out the diagnostic tests, with no impact on patient safety.8
The creation of a pleural pathology unit (PPU) makes even more sense in view of the increasingly technical nature of procedures used in the management of this disease. This is particularly true of ultrasonography, which has reduced the rate of complications associated with different pleural procedures,9 although increased complexity in the diagnosis and treatment of these conditions may be challenging for general respiratory physicians.10
The main objective of our study was to evaluate the clinical impact of the creation of a PPU on the 4 most prevalent pleural diseases treated in our respiratory department: primary spontaneous pneumothorax (PSP), secondary spontaneous pneumothorax (SSP), malignant pleural effusion (MPE), and complicated parapneumonic pleural effusion (CPPE), and to assess in-hospital mortality in the latter.
Primary objectives:
- none◦
Analysis of variance of mean hospital stays.
- none◦
Impact on 30-day readmission rate.
- none◦
Impact on the need for surgical treatment (decortication in the case of the CPPE or intervention for persistent air leak in the case of PSP and SSP).
- none◦
Reduction of mortality during hospitalization for CPPE.
In cases in which patients required surgical treatment for resolution of their disease, mean stays also included time under the care of the thoracic surgery department.
Secondary objectives:
Analysis of inpatient and outpatient pleural procedures from the time of implementation of the PPU.
Materials and methodsThe Hospital Central Universitario de Asturias is a tertiary 1039-bed hospital with a catchment area of around 350,000 inhabitants. It is also a reference center for the entire autonomous community (approximately 1,050,000 inhabitants).
In view of the high number of patients with pleural disease in our health area and the considerable number of referrals from other specialties for these conditions, the decision was taken in 2015 to create a PPU with the aim of improving the relationship between hospital departments and the care of patients with pleural disease, promoting outpatient care as far as possible. To this end, the PPU was set up to provide 1) care for outpatients, 2) care for hospitalized patients, and 3) an area specializing in pleural techniques and different invasive procedures. In functional terms, the PPU is part of the interventional unit, staffed by 3 pulmonologists and a full-time nurse. The unit does not have a specific number of beds; pulmonology beds are used, according to care needs.
We performed a prospective study that included all patients admitted to the PPU in our pulmonology department between January 2015 and December 2018.
The study was approved by the Research Ethics Committee of the Principality of Asturias under number 186/18.
Study populationWe selected all patients with PSP, SSP, MPE, and CPPE admitted to the PPU who were not candidates for outpatient treatment. A database containing the study variables was developed, which included all patients who presented any of these diseases on admission.
We analyzed descriptive parameters, mean stays, readmissions at 30 days, need for surgery, and in the CPPE group, in-hospital mortality.
The data were compared with those of patients admitted to the pulmonology department for pleural disease during the 2 years before the creation of the PPU (2013–2014). Thus, we evaluated the electronic health records of patients included in the “Millennium” program, and those who met the inclusion criteria were selected.
Inclusion criteria- 1
PSP: patients with no known lung disease who developed spontaneous pneumothorax.
- 2
SSP: patients with previous lung disease who developed spontaneous pneumothorax.
- 3
CPPE: pleural effusion associated with lung infection. We included all patients who, regardless of the size of the effusion, required chest drain due to: biochemical criteria in pleural fluid analysis, such as pH < 7.2, glucose <40 mg/dl, LDH > 1000 IU; existence of purulent effusion, positive cultures, or the presence of septated PE on imaging tests.
- 4
MPE: patient with known malignancy or malignancy diagnosed during hospitalization who developed malignant pleural effusion, defined by the existence of cytology or pleural biopsy positive for malignancy, or pleural nodules with contrast uptake on PET/CT, even in the absence of cytohistological confirmation.
- 1
Patients who had already been admitted to the pulmonology department of any other hospital in our autonomous community and were subsequently referred to our PPU, due to its status as a reference center.
- 2
Patients who, during hospitalization, developed any complication associated with their admission, such as iatrogenic pneumothorax or CPPE due to nosocomial infection in patients admitted for other reasons.
- 3
Patients who requested voluntary discharge.
Patients were treated according to diagnostic and therapeutic algorithms established by the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR).11
All procedures performed since the creation of the PPU were carried out under ultrasound guidance by unit staff.
Statistical analysisTo select the historical cohort, the study period was determined in function of the number of patients needed to obtain a sample size with a statistical power of 90% and a confidence level of 95% (5% alpha error). The sample universe size was established on the basis of all patients admitted to our department during the study period. Under these assumptions, the sample size was set at 96 patients per study disease, so the period of 2 years prior to the implementation of the PPU was selected for the analysis.
For data analysis, patients were grouped according to disease and whether they were included before or after the creation of the PPU. Quantitative variables were expressed as mean and standard deviation (SD) and qualitative variables as percentages. Quantitative variables were compared using the Student’s t test, while the Chi-squared test was used for qualitative variables. Significance for all comparisons was set at p < 0.05. Statistical analyses were performed using STATA program v15.4.2.
ResultsA total of 12,341 patients were admitted to the pulmonology department during the study period, of which 741 were included in our study: 68.9% were men and average age was 61.7 years (SD 19.4). The number of patients (in parentheses) and the percentage of men for each disease was: MPE (272) 53.3%, CPPE (224) 75.9%, PSP (119) 79%, SSP (126) 81%. Age (SD) of patients, broken down by diseases, was as follows: MPE 70.4 (12.7), CPPE 63.2 (14.7), PSP 31.1 (12.7), SSP 69.2 (15.2).
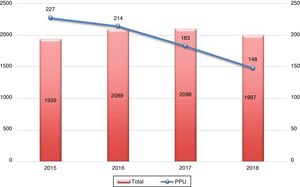
Distribution by number of total admissions to the pulmonology department (including pleural disease) and specifically to the PPU from the time of its creation is summarized in Fig. 1. A progressive decrease in admission of patients with pleural disease can be observed (Fig. 2).
The creation of the PPU resulted in a large number of procedures being performed on an outpatient basis, an effect that increased progressively from the outset. Great advances were also made in the implementation of some techniques, particularly ultrasound-guided procedures, such as peripheral pulmonary lesion biopsies and the placement of different types of chest tubes using either the Argyle or the Seldinger technique (Table 1).
Total procedures performed.
| 2015 | 2016 | 2017 | 2018 | ||
|---|---|---|---|---|---|
| Chest tube | Total | 184 | 195 | 215 | 228 |
| Outpatient | – | – | – | – | |
| Chemical pleurodesis | Total | 17 | 16 | 22 | 13 |
| Outpatient | – | – | – | – | |
| Biopsy of pleuraa and peripheral pulmonary lesions | Total | 21 | 55 | 60 | 36 |
| Outpatient | 9.5 | 21.8 | 43.3 | 44.4 | |
| Diagnostic thoracentesis | Total | 256 | 274 | 308 | 288 |
| Outpatient | 24.6 | 29.2 | 25.6 | 32.9 | |
| Thoracentesis for evacuation | Total | 184 | 221 | 243 | 210 |
| Outpatient | 41.2 | 51.6 | 54.3 | 53.8 | |
| Tunneled catheters | Total | 12 | 28 | 40 | 42 |
| Outpatient | 25 | 53.6 | 70 | 78.6 | |
| Medical thoracoscopy | Total | 4 | 6 | 8 | 4 |
| Outpatient | – | – | – | – |
Totals also include the sum of procedures performed in both inpatients and outpatients in absolute numbers.
In outpatients, the percentage of procedures done on an outpatient basis of the total procedures is indicated.
Only procedures performed in the pleural pathology unit are included; those conducted by medical staff from the pulmonology department during continuous attention shifts are excluded.
We analyzed the average length of stay for the different diseases under study, before and after creation of the PPU, together with the rate of readmissions in the first month and the need for surgical intervention (Table 2). Our results showed a significant reduction in length of hospital stay, with no corresponding increase in the rate of readmissions. In fact, in the case of MPE, significantly fewer patients were readmitted at 1 month after the creation of the PPU.
Mean hospital stays, readmission rates within 30 days after discharge, and need for surgery.
| Mean stay (days) | Readmission (%) | Need for surgery (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| NPPU | PPU | p | NPPU | PPU | p | NPPU | PPU | p | |
| PSP | 6.2 (4.5) | 4.2 (2.9) | 0.004 | 6.3 | 5.7 | 0.6 | 15.6 | 9.2 | 0.33 |
| SSP | 13.2 (11.7) | 8.6 (6.4) | 0.005 | 6.8 | 3.7 | 0.4 | 9.1 | 12.2 | 0.42 |
| CPPE | 18.3 (12.7) | 11.9 (6.8) | 0.001 | 3.8 | 8.2 | 0.27 | 11.7 | 8.9 | 0.49 |
| MPE | 10.3 (7.4) | 12.3 (10) | 0.05 | 9.3 | 2.9 | 0.024 | – | – | – |
Hospital stays are expressed together with standard deviation.
CPPE: complicated parapneumonic pleural effusion; MPE: malignant pleural effusion; NPPU: before the creation of the PPU; PPU: pleural pathology unit; PSP: primary spontaneous pneumothorax; SSP; secondary spontaneous pneumothorax.
Mortality in patients with CPPE decreased significantly after vs. before creation of the PPU (from 14.9% to 5.5% [p = 0.021]). It should be noted that the number of cancer patients with CPPE was very high in our series, both before and after creation of the PPU, with no differences between the study periods (32.1% vs. 30.1% (p = 0.76).
Decortication for CPPE before the PPU was established was required in 11.7% of patients. This rate subsequently fell to 8.9%, but did not reach significance (p = 0.49).
DiscussionInterest in pleural disease has increased steadily in recent years due to the increasing prevalence of these diseases12 and the growing number of pleural procedures available to the specialist. This has generated a need for considerable technical skills, while expanding the diagnostic and therapeutic arsenal and minimizing adverse effects. Thus, the diagnosis and treatment of patients with pleural disease require growing numbers of specifically trained professionals, and the impact of pleural involvement on pulmonology departments continues to grow.
Modern imaging techniques can detect small pleural effusions or pleural thickening requiring drainage at increasingly earlier stages. In some diseases, such as CPPE, diagnosis and early drainage of pleural collections improves prognosis and shortens length of stay.13–15 In diseases such as MPE, the availability of treatments based on results obtained from the molecular analysis of histological samples, together with improved survival rates explain the growing numbers of patients treated and hospitalized for these conditions.16 Several authors have described the technical specialization taking place in pleural disease.10,17 However, it is less common to find references to PPUs integrated into pulmonology departments, such as ours, which offer comprehensive care, including the clinical treatment of all of patients admitted for pleural disease and their interventional procedures. Nor have we found studies assessing the impact of these units on the care of hospitalized patients.
For our study, we selected the most prevalent diseases for which outpatient management was not indicated. We observed an overall decrease in admissions for pleural diseases, probably due to the rapid resolution of problems in the outpatient clinic. Nevertheless, we were unable to reduce the number of admissions or average length of stay in patients with MPE, although we succeeded in significantly reducing 1-month readmission rates. These results might be explained by two factors: first, the tendency to admit to the PPU patients with non-lung cancer MPEs who are usually treated in other departments; and secondly, our department is responsible for palliative care in patients with advanced tumor disease who are not candidates for chemotherapy or who have poor social support systems. These circumstances prevented us from significantly reducing these study parameters.
In contrast, we have been able to significantly reduce mean stays for other “acute” diseases that necessarily require admission, such as PSP, SSP, and CPPE, without producing higher readmission rates, despite the fact that our mean hospital stay figures include patients who subsequently required surgery. About one third of CPPE patients in our series also presented advanced tumor disease with MPE, which probably had a negative impact on mean hospital stays.
We specifically analyzed CPPE mortality, given that mortality in patients admitted for pneumothorax is practically zero, and represents a parameter that is difficult to modify in patients with MPE, given their underlying disease. A significant reduction in CPPE mortality was observed, with lower rates of decortication than those described in the literature for this disease.13,18 Several factors might explain these results, including the administration of fibrinolytic agents in septated CPPE, the systematic use of ultrasound for performing the different pleural procedures, and participation of trained medical and nursing staff in these procedures.
Many diagnostic and therapeutic procedures previously performed in hospitalized patients are now performed in the outpatient setting, and this probably explains the reduction observed in the overall number of admissions. It should be noted here that most inappropriate admissions in a pulmonology department are due to patients waiting for diagnostic tests, results, and interdepartmental consultations.19 This conclusion was also made by Velasco et al.20 in a study carried out in a regional hospital in Asturias, where the greatest number of inappropriate admissions were seen in the pulmonology department, especially in patients with MPE.21
Our study also has several weaknesses. To compare results, we resorted to a historical retrospective cohort. However, given that the study population were all patients admitted to the hospital in the 2 years prior to the creation of the UPP, and that all the diagnostic parameters and other data of interest were recorded in the electronic clinical history, very little information was missing. The study was conducted in a single hospital, with the limitations that this entails for the extrapolation of data. The applicability of results may also be problematic, given the need for professionals trained specifically in the management of thoracic ultrasound and the various pleural procedures, as recommended in various publications.10
However, we believe that the overall experience has been highly satisfactory. The use of homogeneous criteria and the fact that diagnostic and therapeutic procedures are performed by the same professional who manages medical discharge generates a more streamlined system that depends less on the waiting lists of other departments. This has been reflected previously in other diseases in a study by Anton and Sanchis.3
It should also be noted that pleural units are the best environment for teaching the theoretical knowledge and skills required by new medical residents.22 They also provide decent numbers of patients for setting up databases that are useful for clinical research. In the PPU of our hospital, each resident performs a formal 2-month rotation, and also conducts multiple procedures during their specific specialty training periods.
ConclusionsThe creation of a PPU can decrease the number of unnecessary admissions, significantly reduce the length of stays, and decrease mortality in patients with CPPE.
Conflict of interestsThe authors state that they have no conflict of interests.
Please cite this article as: Rodríguez AIE, Clemente MG, Álvarez IR, Valverde TH, Huertas JH, Guillén MA, et al. Impacto clínico de una unidad de patología pleural en un hospital de tercer nivel. Arch Bronconeumol. 2020;56:143–148.