Chondroid chordoma is an extremely rare tumour with an annual incidence of around 0.1 cases per 100000population. Involvement of the thoracic vertebrae may be present in 2%–5% of cases.
Definitive diagnosis usually requires a suitable distinction between this and other mesenchymal tumours such as chondrosarcomas, so immunohistochemical analysis is virtually mandatory.
In spite of its slow-growing nature, chondroid chordoma tends to relapse, and it may eventually become malignant, often jeopardising the patient's prognosis. Although surgery remains the main therapeutic approach, research into the molecular and genetic aspects of this tumour is ongoing. These new advances are likely to improve future oncology therapies by complementing surgery and radiotherapy, changing the currently poor prognosis.
We report the case of a patient with a chondroid chordoma involving the thoracic vertebrae and pleural cavity, and the treatment performed.
El cordoma condroide de localización vertebral torácica es un tipo de tumor que constituye una auténtica rareza. La incidencia anual del cordoma condroide se cifra en 0,1/100.000habitantes, y la afectación torácica se aprecia en el 2 al 5% de los casos.
Su diagnóstico definitivo se ve complicado por su semejanza con otros tumores como los condrosarcomas, por lo que es preciso acudir al estudio inmunohistoquímico.
Su capacidad de recidiva y la tendencia a la malignización a pesar de su naturaleza de lento crecimiento provocan que su tratamiento, predominantemente quirúrgico, sea de una complejidad nada desdeñable. Su comportamiento evolutivo tan agresivo está siendo motivo de estudio a nivel molecular y genético para la elaboración de nuevas terapias oncológicas médicas con el fin de complementar la cirugía y la radioterapia, cuando estas sean aplicables.
Se presenta un caso de localización torácica vertebral e intrapleural, así como el tratamiento practicado.
Chordoma is a slow-growing malignant tumour originating from remnants of the notochord.1,2 It accounts for 1%–4% of malignant primary bone tumours, 50% of which are located in the sacrococcygeal region.1 Its annual incidence is 0.1/100000 population, and thoracic involvement may be observed in 2%–5% of cases.2
It is the only neoplasm of embryogenic origin that presents in the later decades of life. In the case of the vertebrae, it usually appears in young individuals and is much more aggressive.3 It occurs predominantly in males (2.7/1–1.6/1).1,2Chordomas have a great capacity for recurrence and malignant transformation, despite their slow-growing nature.1–8
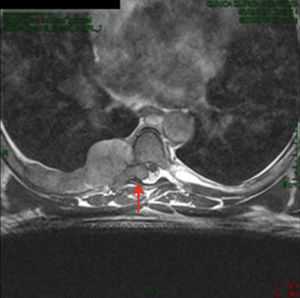
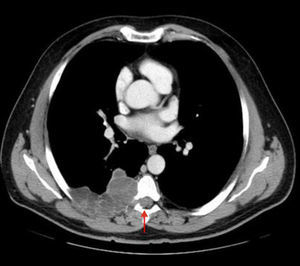
Clinical ObservationA 52-year-old man, with no medical history of interest, presented with a 6-month history of dorsal thoracic pain. As the patient's symptoms did not improve, it was decided to perform magnetic resonance imaging (MRI), following a normal chest radiograph. The diagnosis was costal hydatidosis with intraspinal extension (Fig. 1). Due to questions about the nature of this process, a thoracoabdominal computed tomography (CT) scan was requested, in which an 88mm×60mm×95mm right paravertebral mass was found. It was predominantly cystic with lobulated contours, extrapleural morphology and protruded through the right foramen between the sixth and seventh costal arches towards the spinal canal, extending paravertebrally from the fourth to the seventh right posterior costal arches, involving the extrapleural fat and extending towards the dorsal muscles through the intercostal spaces, with no costal involvement. As a result, the new suspected diagnosis was soft tissue sarcoma (Fig. 2). Fine needle aspiration was carried out (non-diagnostic). Given the intraspinal finding of the mass, it was decided to use a combined neurosurgical and thoracic approach.
Resection and excision of the extradural intraspinal tumour was performed with a D5–D6 laminectomy and en bloc excision of a large tumour attached to the parietal pleura, together with atypical resection of segment 6 and posterior segment of the right upper lobe, adding costal resection of the sixth and seventh ribs and their respective intercostal spaces, as well as the fifth intercostal space. Other lesions contiguous with the large tumour were observed, which required extrapleural resection. Curettage of vertebral zone D6–D7 was performed. Once the whole specimen had been resected en bloc, disseminated lesions could be observed in the diaphragmatic and parietal pleura, suspicious of implants that were shown to be secondary to the lesion. The defect was reconstructed using prosthetic material covered by the trapezius muscle. The patient was discharged on the seventh day post-operatively with satisfactory clinical process and no neurological involvement.
Pathological examination revealed the presence of a 12.8cm×7.3cm chondroid chordoma, which respected the underlying skeletal muscle and resected lung parenchyma.
After treatment with adjuvant radiotherapy and EGFR inhibitors, the disease is currently stable and the patient remains free of neurological symptoms.
DiscussionThe presence of chordomas at the level of the thoracic vertebrae is a rare entity (Table 1). Their main symptom is mechanical pain, but they progress with the onset of neurological symptoms due to their growth.
Chordoma Series With Vertebral Involvement.
| Author | Year | Vertebral/Total Chordomas |
| Utne and Pugh | 1955 | 2/72 |
| Higinbothan | 1967 | 2/46 |
| Cummings | 1983 | 0/34 |
| Volpe | 1983 | 0/25 |
| Rich | 1985 | 1/48 |
| O’Neill | 1985 | 0/34 |
| Amendola | 1986 | 1/21 |
| Azzarelli | 1988 | 0/33 |
| Coffin | 1993 | 2/12 |
| Author | Year | Vertebral Chordomas/Spinal Chordomas |
| Sundaresan | 1979 | 2/54 |
| Meyer | 1984 | 3/21 |
| Bjornsson | 1993 | 7/40 |
| Boriani | 2006 | 1/52 |
CT scans are used to characterise the involvement of the vertebral bodies, presence of a paravertebral tumour, and intraspinal and disc space involvement.1 MRI helps to clarify the epidural extension, spinal cord compression or the presence of epidural metastases.1,5 The use of positron emission tomography (PET) or PET-CT, where the chordoma behaves like a lesion with increased glucose uptake, is very discreetly referenced in the literature, both for the initial diagnosis and for follow-up.9
Depending on its histopathology,4 it can be classified into: classic, chondroid, undifferentiated, sarcomatoid, intradural and intraspinal (mediastinal).
Its diagnosis is confirmed by cytokeratin-positive staining6 and expression of the brachyury gene.7 This gene is a specific biomarker that enables differentiation between chordomas and chondrosarcomas,7,10 and is the object of gene therapy studies. Other alternatives are being investigated along the same line, such as the use of EGFR inhibitors (erlotinib and combined gefitinib-cetuximab), with promising results.8
The ideal treatment is through an aggressive surgical approach, attempting to achieve en bloc resection with the widest free surgical margins possible, otherwise recurrence generally occurs,2,5 although this is not always possible given the extension of the lesion and/or structures affected.
Without adequate margins, adjuvant radiotherapy must be administered to try to increase the hypothetical disease-free survival.1,2 The local recurrence rate is around 26%–68%.2 Chordomas can metastasise in 20%–60% of cases1 (skin, lung, lymphatic system, etc.). The 5-year survival for this tumour is generally between 10% and 70%.1,2,8
Please cite this article as: Royo Crespo I, Rivas de Andrés JJ, Embún Flor R, Cortés Franco S. Cordoma condroide de localización atípica. Arch Bronconeumol. 2013;49:491–493.