COPD and emphysema due to alpha-1 antitrypsin deficiency (AATD) are the first and fourth indications for lung transplantation worldwide, respectively. Despite this, there is little information regarding the health status of these patients at the time of transplantation.
MethodsPatients who received a lung transplant in the Hospital Vall d’Hebron between July 1993 and August 2013 were identified and data from the evaluation prior to the transplant were collected.
ResultsA total of 217 patients who received a lung transplant for COPD and 19 in whom the indication was AATD were included. These patients were severely impaired at the time of the evaluation for lung transplantation, although the trend in recent years has been to evaluate patients at earlier stages of the disease.
Baseline characteristics were similar in both groups except that patients with AATD were younger [43 (7.7) vs 53.6 (6.1) years old, P<.001], with less exposure to tobacco [23.9 (15) vs 50 (29) packs-year, P<.002] and lower PCO2 [41.7 (7.6) vs 47.9 (9.7) mmHg, P<.004].
ConclusionsThe number of patients receiving a lung transplant for COPD has progressively increased and the tendency is to perform the evaluation in earlier stages of the disease. Patients receiving transplants for COPD and AATD had similar characteristics at the time of the evaluation, although AATD patients were younger and had less exposure to tobacco and lower PCO2.
La EPOC y el enfisema secundario a déficit de alfa-1 antitripsina (DAAT) son la primera y la cuarta causa de trasplante pulmonar en el mundo, respectivamente, a pesar de lo cual disponemos de poca información sobre la situación en la que estos pacientes llegan al trasplante.
MétodosSe identificó a los pacientes trasplantados por EPOC y por enfisema secundario a DAAT en el Hospital Vall d’Hebron entre julio de 1993 y agosto de 2013 y se recogieron datos de la evaluación previa al trasplante.
ResultadosSe incluyó a un total de 217 pacientes trasplantados por EPOC y 19 por enfisema secundario a DAAT. Los pacientes evaluados para trasplante por estas enfermedades presentaban una afectación grave de su enfermedad aunque en los últimos años se observó una tendencia a realizar la evaluación en estadios más precoces. Ambos grupos presentaban características similares, excepto que los pacientes con DAAT eran más jóvenes (43 [7,7] vs. 53,6 [6,1] años; p<0,001), con un menor consumo de tabaco (23,9 [15] vs. 50 [29] paquetes/año; p=0,002) y menor PCO2 (41,7 [7,6] vs. 47,9 [9,7] mmHg, p=0,004).
ConclusionesEl número de pacientes trasplantados por EPOC ha aumentado progresivamente, observándose una tendencia a realizar la evaluación de trasplante en estadios más tempranos de la enfermedad. Los pacientes evaluados para trasplante por EPOC y por enfisema secundario a DAAT presentan características similares, aunque estos últimos eran más jóvenes, tenían un menor consumo de tabaco y menor PCO2.
A total of 37581 lung transplants were carried out worldwide between January 1995 and June 2012, 12602 (33.5%) of which were due to chronic obstructive pulmonary disease (COPD), the most common reason for lung transplant, followed by idiopathic pulmonary fibrosis and cystic fibrosis. The COPD group does not include patients undergoing transplant for emphysema secondary to alpha-1 antitrypsin deficiency (AATD), which itself is the fourth indication for lung transplant, with 2182 transplants conducted during this period, accounting for 5.8% of the total.1
AATD is a genetic disease that is associated with low levels of alpha-1 antitrypsin (AAT) in blood and tissues, and predisposes the individual to lung and liver disease.2 AATD emphysema is the most common potentially fatal congenital disease in adulthood, and is also the most common cause of morbidity and mortality in patients with severe AATD. Up to one third of patients have significant disability at a young age due to the respiratory disease, and survival of these patients is lower than that of the general population.3 It is usually detected in advanced stages of the disease, so it is highly underdiagnosed.4
Medical treatment of patients with AATD emphysema should include pharmacological and non-pharmacological measures common to COPD patients. Moreover, purified AAT from donor plasma for intravenous administration has been available since 1987. The aim is to raise AAT levels in plasma and lung interstitium to prevent destruction of the parenchyma, and arrest the progression of emphysema in selected patients.2
Patients with COPD with or without AATD who present with significant functional deterioration may benefit from lung transplantation, primarily to improve survival, although there is little information on transplantation for AATD.5 The aim of this study was to describe the characteristics of patients with AATD emphysema on their arrival for lung transplantation compared to those of patients who received a transplant for COPD. We also describe any changes observed in the clinical characteristics of patients evaluated for transplantation from the start of the lung transplant program to the present day.
MethodsA cross-sectional observational study was conducted in patients evaluated for lung transplantation for COPD with and without AATD in Hospital Universitari Vall d’Hebron (Barcelona, Spain) between July 1993 and August 2013.
The study was carried out according to the principles of the Declaration of Helsinki and current regulations for conducting research studies in human subjects. Patient confidentiality was maintained at all times, in compliance with Spanish law 15/1999 on Data Protection.
The following data were collected at the time of the transplant evaluation: medical history, sociodemographic and clinical data, and the findings of lung function tests, arterial blood gases and 6-minute walk test (6-MWT).
Lung function tests were carried out using the MasterLab system (MasterLab, Jaegger, Germany), following the recommendations of the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR).6 The 6-MWT, standardized according to international recommendations, was used to evaluate exercise capacity.7
Statistical AnalysisBefore analysis, quality control was carried out to identify anomalous data in each variable. Frequency and valid percent were determined in the case of the qualitative variables. Central tendency (mean, median), position (quartiles) and dispersion measures (standard deviation and interquartile range [IQR]) were calculated for the quantitative variables.
In the case of qualitative variables, patient characteristics were compared according to the year of transplant or group (COPD with or without AATD) using the Chi-squared test or Fisher's test (if the observed frequency was <5). In the case of ordinal variables, the linear trend was determined using Kendall's Tau-c coefficient. Quantitative variables were compared using the Student's t-test (<2 categories) and analysis of variance (ANOVA) (in the case of variables >2 categories), linear trend test and multiple comparisons test (Scheffé). Analysis was performed using the SPSS 19.0 statistics package (Chicago, IL, USA). A significant difference was determined for all tests based on a P value <.05.
ResultsA total of 695 lung transplants were performed in Hospital Vall d’Hebron from1993 to 2013. Of these, 31.2% (n=217) were carried out in patients with COPD and 8% (n=19) in patients with AATD emphysema. Patients with AATD had homozygous PiZZ phenotype in 18 cases, and 1 was homozygous for the rare PiYbarcelona8 variant.
Patients included in the study had a mean age of 53.1 (SD: 6.6) years at the time of the lung transplant evaluation, and 80% (n=189) were men. As regard smoking, 95.3% of patients were former smokers and 2.1% were current smokers; mean cumulative tobacco exposure was 48 pack-years (SD: 29). Mean FEV1 (%) was 22.3% (SD: 8.8%). Arterial blood gases showed PO2 60mmHg (SD: 10.8) and PaCO2 47.4mmHg (SD: 9.7). The mean distance walked in the 6-MWT was 231.4m (SD: 86.6). A total of 87.2% of patients were on long-term home oxygen therapy.
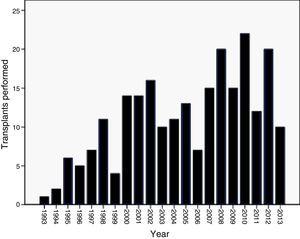
A trend toward an annual increase in the number of lung transplants for COPD was observed, with a higher frequency in 2008, 2010 and 2012 (Fig. 1).
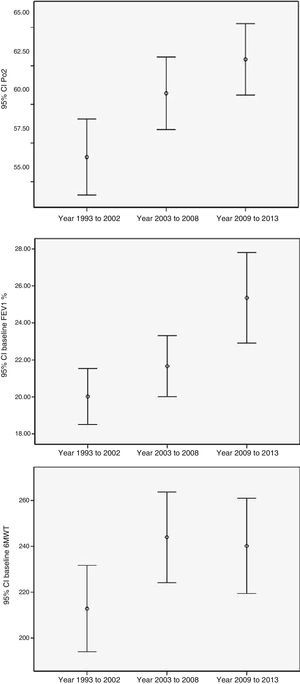
To measure trends over time in patients referred for lung transplantation, the study was divided into 3 periods. Patients evaluated for transplantation in the last period (2009–2013) were older (P=.001), with a lower percentage of men (P=.001), with less FEV1 decline (L and %) (P=.038 and P<.001, respectively), better exercise tolerance measured using the 6MWT (P=.050) and higher PO2 (P=.001) (Table 1) (Fig. 2).
Clinical Characteristics of the Patients Evaluated for Transplant According to Period.
| Variables | Period1993–2002No.=80 | Period2003–2008No.=77 | Period2009–2013No.=79 | P |
|---|---|---|---|---|
| Age (years) | 50.9 (7.4) | 54.2 (6.2) | 54.3 (5.5) | .001 |
| Sex (male); n (%) | 73 (91.3) | 61 (80.3) | 54 (68.4) | .001 |
| Smoker (former smoker); n (%) | 73 (91.3) | 75 (98.7) | 76 (96.2) | .189 |
| Tobacco exposure (pack-years) | 43.5 (27) | 50.3 (32.7) | 50.4 (29) | .252 |
| FEV1 (l) | 0.67 (0.24) | 0.69 (0.2) | 0.81 (0.4) | .038a |
| FEV1 (%) | 20.0 (6.8) | 21.7 (7.2) | 25.4 (10.9) | <.001a |
| FVC (l) | 1.64 (0.5) | 1.69 (0.6) | 1.9 (0.7) | .157a |
| FVC (%) | 40.8 (13.9) | 39.9 (13) | 44.3 (12.6) | .097 |
| Walk test (m) | 212.8 (83.5) | 244.0 (82.1) | 240.2 (91.3) | .05a |
| PaCO2 (mmHg) | 48.0 (10.6) | 48.0 (9.5) | 46.0 (8.8) | .338 |
| PO2 (mmHg) | 56.6 (11.1) | 60.7 (10.3) | 62.9 (10.3) | .001 |
| Home oxygen; n (%) | 67 (83.8) | 63 (84) | 74 (93.7) | .105 |
Values in bold are statistically significant.
On comparing the characteristics of patients with AATD emphysema and COPD, the only differences observed were that patients with AATD were younger on average (43 [7.7] vs 53.6 [6.1] years; P<.001), had less tobacco exposure (23.9 [15] vs 50 [29] pack-years; P=.002) and lower PCO2 (41.7 [7.6] vs 47.9 [9.7] mmHg; P=.004) (Table 2).
Demographic and Clinical Characteristics of Patients Evaluated for Transplant by Group.
| AATD patientsNo.=19Mean (SD) | COPD patientsNo.=217Mean (SD) | Pa | |
|---|---|---|---|
| Age (years) | 48.1 (7.7) | 53.6 (6.3) | .002 |
| Sex (male); n (%) | 17 (89.5) | 172 (79.3) | .380 |
| Tobacco exposure (%) (current smokers+former smokers) | 18 (94.8) | 212 (97.7) | .208 |
| Pack-years | 23.9 (15) | 50 (28.9) | <.001 |
| FEV1 (l) | 0.689 (0.2) | 0.734 (0.4) | .687 |
| FEV1 (%) | 20.2 (5.7) | 22.5 (8.9) | .305 |
| FVC (l) | 1.962 (0.6) | 1.734 (0.7) | .170 |
| FVC (%) | 44.4 (12.1) | 41.5 (13.3) | .356 |
| 6-min walk test (m) | 199.2 (91.3) | 234.4 (85.8) | .114 |
| PO2 (mmHg) | 59.4 (6.3) | 60.1 (11.1) | .788 |
| PaCO2 (mmHg) | 41.7 (7.6) | 47.9 (89.7) | .004 |
| Oxygen therapy; n (%) | 17 (89.5) | 188 (87) | .999 |
Values in bold are statistically significant.
The results of this study show that the number of transplants performed for COPD increased in parallel with the number of total transplants. Patients with COPD had very severe disease at the time of their transplant evaluation, although the current trend is to evaluate patients at earlier stages. Patients receiving transplants for COPD or AATD emphysema had similar characteristics at the time of the evaluation, except that the latter were younger, with less cumulative tobacco exposure.
This study found that the number of transplants performed for COPD in our hospital echoes the increase observed in other countries, reaching a peak in 2010–2012. However, the number of transplants carried out for AATD has declined since the start of the transplant program, and accounts for only 2% of the total. In other countries, the number of transplants performed for this reason have remained stable, with rates varying from 6% worldwide to 9% in Sweden,5 even though the number of new diagnoses of AATD emphysema has fallen in Sweden, probably due to the significant drop in smoking rates.5 The reduction in the number of lung transplants for AATD observed in our hospital may be due to improvements in quality of life and symptoms thanks to new treatments for COPD, and particularly to greater accessibility to intravenous AAT augmentation therapy, which has been shown to reduce the decline in FEV1,9–11 loss of lung density12,13 and probably also the frequency of exacerbations14 in these patients.
In our series, at the time of the evaluation, patients receiving a transplant for COPD with or without AATD had very severe disease, with a mean FEV1 of 22.4%. Eighty-nine percent were receiving long-term home oxygen therapy for chronic respiratory failure, and a tendency toward hypercapnia was observed, with a mean PCO2 of 47.4mmHg.
On analyzing the characteristics by study period, it was observed that in recent years (2009–2013), patients were older and arrived at the transplant evaluation with a better functional status, higher FEV1, better 6MWT exercise tolerance, and higher PO2. This could be because the increase in the number of transplants has made this a more widely accepted therapeutic option. As a result, specialists are more aware of this alternative, and tend to refer patients to specialized units at an early stage of the disease. Moreover, the increase in demand has meant that the age limit for receiving a transplant has increased and, with this, the mean age of the patients.
On comparing the characteristics between both groups, patients who received a transplant for AATD emphysema or COPD had similar characteristics at the time of the transplant evaluation. The only differences were that patients with AATD had less tobacco exposure and were younger at the time of the evaluation, which is to be expected given the predisposition to early emphysema associated with this disease.2 These differences have also been observed in patients receiving long-term home oxygen therapy, as patients with AATD were also younger and had fewer comorbidities.15 Our data are consistent with information available in the Spanish registry of patients with AATD (REDAAT), which showed a mean age of 50.5 years and cumulative tobacco exposure of 26.7 pack-years16 at the time of inclusion in the registry; these data are also similar to those in the Italian register.17 In contrast, patients with COPD without AATD had a higher PCO2, probably because patients with AATD have predominantly basal emphysema, which results in less deterioration of gas exchange than apical emphysema.18,19
Lung transplantation is considered a valid therapeutic option for patients with COPD and those with emphysema secondary to AATD. According to the latest data from the International Society of Heart and Lung Transplantation (ISHLT) registry, the median survival of patients receiving lung transplants for all causes is 5.5 years, or 7.7 years for those who survive the first year post-transplant. Patients receiving transplants for COPD and AATD have a median survival of 5.4 and 6.3 years, respectively (6.8 and 8.4 years for those who survive the first year).1 Despite this, there is still little information on the progress of patients who receive a transplant for AATD. In one recent series in Sweden, data on 83 patients with AATD who received a transplant between 1990 and 2010 were collected from the national Swedish AATD registry and compared with a control group of 70 patients with AATD who had not received a transplant. A significant survival benefit was observed in patients with PiZZ who had received a transplant, compared to non-transplant patients.5
In conclusion, patients with AATD emphysema come to the transplant evaluation in a similarly serious condition to other COPD patients, but at a younger age and with less tobacco exposure. Although the number of all-cause transplants has increased gradually since 1993, the number performed for AATD had fallen in our hospital, probably due to improvements in specific disease management and better access to augmentation therapy. In any event, early diagnosis of AATD is essential to prevent pulmonary emphysema from progressing, as recommended in clinical practice guidelines.2,20
Authors’ ContributionsDaniela Giacoboni participated in the study design, data collection and preparation of the database. Miriam Barrecheguren and Esther Rodríguez participated in the evaluation and follow-up of patients with alpha-1 antitrypsin deficiency and COPD. Cristina Esquinas participated in the statistical analysis. Cristina Berastegui, Manuel López-Meseguer and Carlos Bravo participated in the evaluation of patients for lung transplantation. Pietro Pirina participated in the study design. Marc Miravitlles participated in the study design and in the evaluation and follow-up of patients with alpha-1 antitrypsin deficiency. Antonio Roman participated in the study design and in the evaluation of patients for lung transplantation. All the authors have read and approve the data presented and have contributed to the drafting of the manuscript.
Conflict of InterestsMarc Miravitlles has received speaker's fees for educational events organized by Boehringer Ingelheim, Pfizer, AstraZeneca, Novartis, Grifols and Takeda, and for scientific consultancy from Boehringer Ingelheim, Pfizer, GlaxoSmithKline, AstraZeneca, Novartis, Almirall, Gebro Pharma and Takeda.
Daniela Giacoboni of the Institute of Respiratory Diseases, Sassari University (Italy) is the recipient of an unrestricted Erasmus Placement fellowship grant in Hospital Vall d’Hebron, Barcelona (Spain). Laboratorios Grifols funds the Catalan Center for Excellence in Alpha-1 antitrypsin.
Please cite this article as: Giacoboni D, Barrecheguren M, Esquinas C, Rodríguez E, Berastegui C, López-Meseguer M, et al. Características de la población candidata a trasplante pulmonar por enfermedad pulmonar obstructiva crónica y por enfisema secundario a déficit de alfa 1 antitripsina. Arch Bronconeumol. 2015;51:379–383.