We present the case of a 57-year-old male with left hilar squamous cell carcinoma infiltrating the pulmonary artery and in whom a sleeve bronchoplasty and angioplasty were performed using a bovine pericardial conduit. Three days post-operatively, graft thrombosis was detected; thrombectomy and graft reconstruction were performed with revascularisation of the graft.
Presentamos el caso de un varón de 57años con un carcinoma epidermoide hiliar izquierdo que infiltraba la arteria pulmonar y al que se le realizó una broncoplastia en manguito y una angioplastia mediante un conducto de pericardio bovino. En el tercer día postoperatorio se objetivó una trombosis del injerto, realizándose una trombectomía y reconstrucción del injerto con revascularización del mismo.
The use of angioplasty for tumors infiltrating the pulmonary artery can often help avoid pneumonectomy and preserve functioning distal pulmonary parenchyma. However, it is not a risk-free procedure, and diverse complications after this type of intervention have been described in the literature, including bronchopleural fistulas, respiratory distress, pulmonary artery thrombosis, prolonged air leakage and massive hemoptysis.1–3
Clinical CaseWe present the case of a 57-year-old ex-smoker with a history of ischemic heart disease consulting due to hemoptysis. A computed tomography (CT) showed a left hilar mass of 5.6cm in diameter. In the positron emission tomography (PET), the mass had a maximum standard uptake value of 16.7g/ml with lymphadenopathies in stations 4L and 5 and contrast uptake of around 3g/ml. On fiberoptic bronchoscopy, tumoration was observed in the entrance to the upper lobe bronchus. The biopsy returned a diagnosis of epidermoid carcinoma. An EBUS extension study of the lymph node stations 4R and 4L was negative for malignancy.
Dissection and proximal clamping of the pulmonary artery were performed via a left posterolateral thoracotomy. The sulcus was found to have retracted due to tumoration, but the main pulmonary artery and the segment 6 artery could be dissected and radical resection was performed. The principal bronchus and left lower lobar bronchus were dissected and divided. The distal artery was then clamped and the infiltrated pulmonary artery was sectioned. A bronchial anastomosis was constructed between the main bronchus and the lower lobar bronchus with discontinuous sutures using PDS® 3-0. The pulmonary artery was reconstructed with a preformed bovine pericardial conduit with proximal and distal clamping and anastomosis with Prolene™ 5-0. Local and systemic anticoagulation with 5000U heparin sodium was administered before the clamp. When the anastomosis was complete, the air was drained, and the lobe was ventilated and unclamped slowly, ensuring correct flow via the graft.
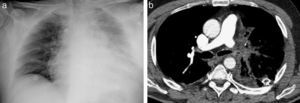
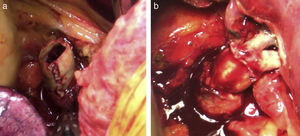
On day 4 after surgery, the patient was breathing normally with pO2 of 75 and 30000ml–1 leukocytes. Alveolar infiltrates in the remaining lobe were observed on X-ray (Fig. 1a). CT angiogram was performed, showing graft thrombosis, so an urgent reintervention was programmed (Fig. 1b and c). A proximal clamp was applied and the vascular suture in the distal anastomosis was removed. The clot was extracted and heparin was administered upstream and downstream from the clamped inferior pulmonary vein. The conduit was cut again and the distal anastomosis reconstructed, with good flow being observed (Fig. 2). The patient progressed well and a CT-angiogram on day 3 after surgery showed flow through the graft with distal filling defects.
The pathology laboratory report on the resected fragment described moderately differentiated epidermoid carcinoma, 6.5cm in diameter, infiltrating the visceral pleura with metastasis in one peribronchial lymph node (T2bN1). Lymphadenopathies in the aortopulmonar, prevascular, tracheobronchial, subcarinal, hilar, paraesophageal and interlobar windows were negative. The patient was discharged on day 27 after surgery, after correct bronchial anastomosis was observed on fiberoptic bronchoscopy.
DiscussionThe use of bovine pericardium for pulmonary artery reconstruction was first described by Rendina et al.2 in 1999. It has great advantages over synthetic material, since it is cheaper, has good resistance and is biocompatible.2,4 It is, however, more difficult to manage. After suturing, it tends to shrink and bend and when blood pressure increases after the clamp is removed, it usually stretches.4 In our case, we think that the complication was caused by bending in the distal suture when the lower lobe was replaced in the hemithorax, due to a technical problem caused by the conduit being excessively long. One case of pulmonary artery thrombosis is described in the literature, in a series from Venuta et al.,3 which was resolved with a pneumonectomy. In our case, this was our first idea when faced with the problem. However, in view of the patient's good clinical status and the good appearance of the lung parenchyma, we decided to attempt thrombectomy. In conclusion, we would like to highlight that thrombectomy with reconstruction of the anastomosis and lobe revascularization is a valid alternative alongside pneumonectomy as surgical treatment of this complication.
Please cite this article as: Peña E, Blanco M, Otero T. Reconstrucción broncovascular con conducto de pericardio bovino y reintervención quirúrgica por trombosis con revascularización. Arch Bronconeumol. 2014;50:42–43.